Primary Ovarian Leiomyoma—A Common Tumor at an Uncommon Site
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Rare Presentation of Benign Brenner Tumor of Ovary: a Case Report
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Periasamy S et al. Int J Reprod Contracept Obstet Gynecol. 2018 Jul;7(7):2971-2974 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20182920 Case Report A rare presentation of benign Brenner tumor of ovary: a case report Sumathi Periasamy1, Subha Sivagami Sengodan2*, Devipriya1, Anbarasi Pandian2 1Department of Surgery, 2Department of Obstetrics and Gynaecology, Government Mohan Kumaramangalam Medical College, Salem, Tamil Nadu, India Received: 17 April 2018 Accepted: 23 May 2018 *Correspondence: Dr. Subha Sivagami Sengodan, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Brenner tumors are rare ovarian tumors accounting for 2-3% of all ovarian neoplasms and about 2% of these tumors are borderline (proliferating) or malignant. These tumors are commonly seen in 4th-8th decades of life with a peak in late 40s and early 50s. Benign Brenner tumors are usually small, <2cm in diameter and often detected incidentally during surgery or on pathological examination. Authors report a case of a large, calcified benign Brenner tumor in a 55-year-old postmenopausal woman who presented with complaint of abdominal pain and mass in abdomen. Imaging revealed large complex solid cystic pelvic mass -peritoneal fibrosarcoma. She underwent laparotomy which revealed huge Brenner tumor weighing 9kg arising from left uterine cornual end extending up to epigastric region. -

Immunohistochemical and Electron Microscopic Findings in Benign Fibroepithelial Vaginal Polyps J Clin Pathol: First Published As 10.1136/Jcp.43.3.224 on 1 March 1990
224 J Clin Pathol 1990;43:224-229 Immunohistochemical and electron microscopic findings in benign fibroepithelial vaginal polyps J Clin Pathol: first published as 10.1136/jcp.43.3.224 on 1 March 1990. Downloaded from T P Rollason, P Byrne, A Williams Abstract LIGHT MICROSCOPY Eleven classic benign "fibroepithelial Sections were cut from routinely processed, polyps" of the vagina were examined paraffin wax embedded blocks at 4 gm and using a panel of immunocytochemical immunocytochemical techniques were agents. Two were also examined electron performed using a standard peroxidase- microscopically. In all cases the stellate antiperoxidase method.7 The antibodies used and multinucleate stromal cells were as follows: polyclonal rabbit characteristic of these lesions stained antimyoglobin (batch A324, Dako Ltd, High strongly for desmin, indicating muscle Wycombe, Buckinghamshire), monoclonal intermediate filament production. In anti-desmin (batch M724, Dako Ltd), mono- common with uterine fibroleiomyomata, clonal anti-epithelial membrane antigen (batch numerous mast cells were also often M613, Dako Ltd), monoclonal anti-vimentin seen. Myoglobin staining was negative. (batch M725, Dako Ltd), polyclonal rabbit Electron microscopical examination anti-cytokeratin (Bio-nuclear services, Read- confirmed that the stromal cells con- ing) and monoclonal anti cytokeratin NCL tained abundant thin filaments with focal 5D3 (batch M503, Bio-nuclear services). densities and also showed the ultrastruc- Mast cells were shown by a standard tural features usually associated with chloroacetate esterase method using pararo- myofibroblasts. saniline,8 which gave an intense red cyto- It is concluded that these tumours plasmic colouration, and by the routine would be better designated polypoid toluidine blue method. myofibroblastomas in view of the above An attempt was made to assess semiquan- findings. -

Fibro-Epithelial Polyp: Case Report with Literature Review
ISSN: 2456-8090 (online) CASE REPORT International Healthcare Research Journal 2017;1(7):14-17. DOI: 10.26440/IHRJ/01_07/116 QR CODE Fibro-Epithelial Polyp: Case Report with Literature Review RATNA SAMUDRAWAR 1, HEENA MAZHAR2, MUKESH KUMAR KASHYAP3, RUBI GUPTA4 A Oral fibroma is the most common benign soft tissue tumor caused due to continuous trauma from sharp cusp of teeth or faulty dental B restoration. It presents as sessile or occasionally pedunculated painless swelling which can be soft to firm in consistency. Its incidence occurs mostly during third to fifth decade and shows preference for female. Its occurrence corresponds with intraoral areas that are S prone to trauma such as the tongue, buccal mucosa and labial mucosa, lip, gingiva. Even with conservative surgical excision, the T lesion may recur until the source of continuous irritation persists. This article presents a case of large size oral fibroma on left alveolar R region associated with ulceration along with literature review. A C KEYWORDS: Benign Connective Tissue Tumor, Fibro-epithelial Polyp, Irritation Fibroma, Traumatic Fibroma, Focal Fibrous T Hyperplasia. K INTRODUCTION Fibroma of the oral mucosa is the most common complaint of growth in left lower back region of benign soft tissue tumor of the oral cavity derived the mouth since 4 months. History elicited that from fibrous connective tissues (CTs).1 Its the a solitary, painless growth had been observed pathogenesis lies in the fact that due to continues in his left mandibular molar region which was local trauma, a type of reactive hyperplasia of initially small in size and then it gradually fibrous tissue occurs.2 Thus, “Focal fibrous enlarged to present size of oval shape, well- hyperplasia” (FFH) term was suggested by Daley defined, pedunculated lesion. -

Soft Tissue Sarcoma Classifications
Soft Tissue Sarcoma Classifications Contents: 1. Introduction 2. Summary of SSCRG’s decisions 3. Issue by issue summary of discussions A: List of codes to be included as Soft Tissue Sarcomas B: Full list of codes discussed with decisions C: Sarcomas of neither bone nor soft tissue D: Classifications by other organisations 1. Introduction We live in an age when it is increasingly important to have ‘key facts’ and ‘headline messages’. The national registry for bone and soft tissue sarcoma want to be able to produce high level factsheets for the general public with statements such as ‘There are 2000 soft tissue sarcomas annually in England’ or ‘Survival for soft tissue sarcomas is (eg) 75%’ It is not possible to write factsheets and data briefings like this, without a shared understanding from the SSCRG about which sarcomas we wish to include in our headline statistics. The registry accepts that soft tissue sarcomas are a very complex and heterogeneous group of cancers which do not easily reduce to headline figures. We will still strive to collect all data from cancer registries about anything that is ‘like a sarcoma’. We will also produce focussed data briefings on sites such as dermatofibrosarcomas and Kaposi’s sarcomas – the aim is not to forget any sites we exclude! The majority of soft tissue sarcomas have proved fairly uncontroversial in discussions with individual members of the SSCRG, but there were 7 particular issues it was necessary to make a group decision on. This paper records the decisions made and the rationale behind these decisions. 2. Summary of SSCRG’s decisions: Include all tumours with morphology codes as listed in Appendix A for any cancer site except C40 and C41 (bone). -

Case Reports 95
r- CASE REPORTS 95 CASE REPORTS Past & family history were not contributory. General physical examination revealed no abnor mality. On abdominal examination- abdomen was overdistended, presenting part could not be made out, however there was suspicion of breech ABilA SINGH • NEERJA SETIII presentation. Fetal heart was not localised, mod erate uterine contractions were present. On per NEERA AGARWAL • K MISRA vaginum examination- cervix was fully effaced and 5 em dilated, soft irregular presenting part INTRODUCTION was felt high up at brim and liquor was blood 1 / Sacroccocygeal teratoma is a potentially stained. 2 2 hours later the patient delivered a 28 malignant congenital tumour. The incidence re weeks size still born female fetus weighing 850 ported in India is 1 in 30,000-40,000 live births. grns by breech. There was no PPH. Placenta These tumours present either as obstructed labour or dystocia. The case is reported because of its rare occurence. CASE REPORT Mrs. K. 22 year old unhooked, primigravida was admitted to G.T.B. Hospital with 7 months amenorrhoea and labour pains for 3 hours. Her antenatal period was uneventfull with no history of drug intake. Menstrual Cycles were regular. 'Dtpt. of 06Jt<t antf qynu, antf 'Patfw. ~cctp tttf for 'Pu6lication on 2216/ 91 fig. 1 96 JOURNAL OF OBSTETRICS AND GYNAECOLOGY weighed 120 gm. There was no gmss abnormal AIIMS as she was Rb -ve. She bad a diagnostic ity detected in the placenta. laparoscopy one year back at a private hospital Examination of the fetus showed a bilobed where a bicornuate uterus was diagnosed and massofl5x 17 cmarisingfromtbesacrococcygeal excision of complete longitudinal vaginal sep region with partial rupture of one lobe, cut tum was done. -
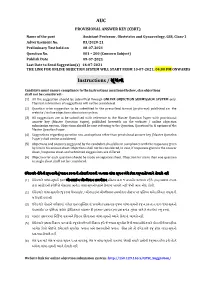
AUC Instructions / ૂચના
AUC PROVISIONAL ANSWER KEY (CBRT) Name of the post Assistant Professor, Obstetrics and Gynaecology, GSS, Class-1 Advertisement No. 83/2020-21 Preliminary Test held on 08-07-2021 Question No. 001 – 200 (Concern Subject) Publish Date 09-07-2021 Last Date to Send Suggestion(s) 16-07-2021 THE LINK FOR ONLINE OBJECTION SYSTEM WILL START FROM 10-07-2021; 04:00 PM ONWARDS Instructions / ૂચના Candidate must ensure compliance to the instructions mentioned below, else objections shall not be considered: - (1) All the suggestion should be submitted through ONLINE OBJECTION SUBMISSION SYSTEM only. Physical submission of suggestions will not be considered. (2) Question wise suggestion to be submitted in the prescribed format (proforma) published on the website / online objection submission system. (3) All suggestions are to be submitted with reference to the Master Question Paper with provisional answer key (Master Question Paper), published herewith on the website / online objection submission system. Objections should be sent referring to the Question, Question No. & options of the Master Question Paper. (4) Suggestions regarding question nos. and options other than provisional answer key (Master Question Paper) shall not be considered. (5) Objections and answers suggested by the candidate should be in compliance with the responses given by him in his answer sheet. Objections shall not be considered, in case, if responses given in the answer sheet /response sheet and submitted suggestions are differed. (6) Objection for each question should be made on separate sheet. Objection for more than one question in single sheet shall not be considered. ઉમેદવાર નીચેની ૂચનાઓું પાલન કરવાની તકદાર રાખવી, અયથા વાંધા- ૂચન ગે કરલ રૂઆતો યાને લેવાશે નહ (1) ઉમેદવાર વાંધાં- ૂચનો ફત ઓનલાઈન ઓશન સબમીશન સીટમ ારા જ સબમીટ કરવાના રહશે. -

Histogenesis of Ovarian Malignant Mixed Mesodermal Tumours J Clin Pathol: First Published As 10.1136/Jcp.43.4.287 on 1 April 1990
J Clin Pathol 1990;43:287-290 287 Histogenesis of ovarian malignant mixed mesodermal tumours J Clin Pathol: first published as 10.1136/jcp.43.4.287 on 1 April 1990. Downloaded from T J Clarke Abstract embedded tumour tissue were cut at 4 im and The histogenesis of ovarian malignant stained with haematoxylin and eosin, periodic mixed mesodermal tumours, which acid Schiff (PAS) before and after diastase includes the concept of metaplastic car- treatment, Caldwell and Rannie's reticulin cinoma, is controversial. Four such stain, and phosphotungstic acid haematoxylin tumours were examined for evidence of (PTAH). Sequential sections were stained by metaplastic transition from carcinoma to the indirect immunoperoxidase technique sarcoma using morphology and reticulin using monoclonal antibodies directed against stains. Consecutive sections were stained cytokeratin (PKK1 which reacts with low immunohistochemically using cyto- molecular weight cytokeratins of44, 46, 52 and keratin and vimentin to determine 54 kilodaltons), vimentin, a-l-antitrypsin and whether cells at the interface between myoglobin. Appropriate positive and negative carcinoma and sarcoma expressed both controls, with omission of specific antisera in cytokeratin and vimentin. There was no the latter, were performed. Haematoxylin and evidence ofmorphological, architectural, eosin stained sections were examined for or immunohistochemical transitions secondary fluorescence using a Leitz Dialux from carcinoma to sarcoma in the four 20ES microscope and mercury vapour light tumours studied. This suggests that source epifluorescence. ovarian malignant mixed mesodermal Four patients, aged 68, 71, 72 and 73 presen- tumours are not metaplastic carcinomas ted with abdominal distension and discomfort but are composed of histogenetically dif- and were found to have an ovarian malignant ferent elements. -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

Ovarian Fibrothecoma - a Diagnostic Dilemma
Obstetrics & Gynecology International Journal Case Report Open Access Ovarian fibrothecoma - a diagnostic dilemma Abstract Volume 10 Issue 3 - 2019 Background: The presentation of ovarian fibrothecoma is highly deceptive and it may Nikita Kumari,1 Bindu Bajaj2 be undiagnosed till histopathology reveals the actual diagnosis. Hence, the clinician 1 must be aware of such cases which may present as a diagnostic dilemma. Attending Consultant at Sitaram Bhartia Institute of Science and Research, Ex Senior Resident at VMMC and Safdarjung Introduction: Ovarian fibrothecomas are rare ovarian neoplasm. We report a case Hospital, India where clinical presentation was highly deceptive and suggestive of malignant tumor. 2Associate Professor at VMMC and Safdarjung Hospital, New However, ascitic fluid cytology revealed absent malignant cells. On histopathological Delhi, India examination, it was diagnosed as benign fibrothecoma with cystic changes. Postoperative follow-up for about six months was uneventful. Correspondence: Nikita Kumari, Attending Consultant at Sitaram Bhartia Institute of Science and Research, Ex Senior Case: A 45 year old female presented with large abdominal lump of 20 weeks size Resident at VMMC and Safdarjung Hospital, New Delhi, India, Tel associated with pain abdomen. She was admitted for management and evaluation. 9654251653, Email Hematological and biochemical parameters were normal. USG revealed a large multilocular, predominantly cystic lesion 20.9x9.6x11.4 cm in pelvis. CECT revealed Received: May 27, 2019 | Published: June 13, 2019 ovarian cystadenocarcinoma left ovary with locoregional mass effect, mild ascites and suspicious metastasis to internal iliac lymph nodes. Hence panhysterectomy and omentectomy was performed as radiological and preoperative clinical diagnosis was malignant ovarian tumor. On gross examination, a well encapsulated, multinodular cystic tumor of left ovary about 17x14x7 cm was identified. -

Brenner Tumor of Ovary: an Incidental Finding: a Case Report
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Jodha BS et al. Int J Reprod Contracept Obstet Gynecol. 2017 Mar;6(3):1132-1135 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20170600 Case Report Brenner tumor of ovary: an incidental finding: a case report Bhanwar Singh Jodha, Richa Garg* Department of Obstetrics and Gynecology, Umaid Hospital, Regional Institute of Maternal and Child Health, Dr. S. N. Medical College, Jodhpur, Rajasthan, India Received: 20 December 2016 Accepted: 31 January 2017 *Correspondence: Dr. Richa Garg, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Brenner tumor of the ovary is very rare, mostly benign, small, and unilateral. Malignant brenner tumor is much rarer. Malignant brenner tumor of ovary closely resembles the transitional cell carcinoma of ovary. These tumors are believed to arise from urothelial metaplasia of ovarian surface epithelium. However the latter has a worse prognosis. Here we present a case of Brenner tumor of ovary in a postmenopausal woman treated surgically and its features are briefly discussed. Keywords: Brenner tumor, Ovarian neoplasm, Ultrasonography INTRODUCTION bladder epithelium.7 The Brenner tumors are usually small, solid, firm grayish knots up to 2 cm in size, Ovarian tumors are common forms of neoplasia in however, they may also be quite big, and in such cases women and it accounts for about 30.0% of female genital they usually have cystic components as a result of cystic cancers.1 Ovarian carcinoma is the fourth most common degeneration and necrosis. -

A Clinical and Histopathological Study of 122 Cases of Dermatofibroma (Benign Fibrous Histiocytoma)
Ann Dermatol Vol. 23, No. 2, 2011 DOI: 10.5021/ad.2011.23.2.185 ORIGINAL ARTICLE A Clinical and Histopathological Study of 122 Cases of Dermatofibroma (Benign Fibrous Histiocytoma) Tae Young Han, M.D., Hee Sun Chang, M.D., June Hyun Kyung Lee, M.D., Won-Mi Lee, M.D.1, Sook-Ja Son, M.D. Departments of Dermatology and 1Pathology, Eulji General Hospital, College of Medicine, Eulji University, Seoul, Korea Background: Many variants of dermatofibromas have been INTRODUCTION described, and being aware of the variants of derma- tofibromas is important to avoid misdiagnosis. Objective: Dermatofibroma (benign fibrous histiocytoma) is a We wanted to evaluate the clinical and pathologic common skin lesion and it accounts for approximately 3% characteristics of 122 cases of dermatofibromas. Methods: of the skin lesion specimens received by one derma- We retrospectively reviewed the medical records and 122 topathology laboratory1. There is a predilection for derma- biopsy specimens of 92 patients who were diagnosed with tofibroma to develop on the extremities, and particularly dermatofibroma in the Department of Dermatology at Eulji on the lower extremities of young adults. There is a female Hospital of Eulji University between January 2000 and preponderance amongst the patients with dermatofib- March 2010. Results: Nearly 80% of the cases occurred roma1. Dermatofibroma is round or ovoid, firm, dermal between the ages of 20 and 49 years, with an overall nodules and they are usually <1 cm in diameter2. The predominance of females. Over 70% of the lesions were diagnosis is usually straightforward if the classical clinical found on the extremities. -

Table of Contents
CONTENTS 1. Specimen evaluation 1 Specimen Type. 1 Clinical History. 1 Radiologic Correlation . 1 Special Studies . 1 Immunohistochemistry . 2 Electron Microscopy. 2 Genetics. 3 Recognizing Non-Soft Tissue Tumors. 3 Grading and Prognostication of Sarcomas. 3 Management of Specimen and Reporting. 4 2. Nonmalignant Fibroblastic and Myofibroblastic Tumors and Tumor-Like Lesions . 7 Nodular Fasciitis . 7 Proliferative Fasciitis and Myositis . 12 Ischemic Fasciitis . 18 Fibroma of Tendon Sheath. 21 Nuchal-Type Fibroma . 24 Gardner-Associated Fibroma. 27 Desmoplastic Fibroblastoma. 27 Elastofibroma. 34 Pleomorphic Fibroma of Skin. 39 Intranodal (Palisaded) Myofibroblastoma. 39 Other Fibroma Variants and Fibrous Proliferations . 44 Calcifying Fibrous (Pseudo)Tumor . 47 Juvenile Hyaline Fibromatosis. 52 Fibromatosis Colli. 54 Infantile Digital Fibroma/Fibromatosis. 58 Calcifying Aponeurotic Fibroma. 63 Fibrous Hamartoma of Infancy . 65 Myofibroma/Myofibromatosis . 69 Palmar/Plantar Fibromatosis. 80 Lipofibromatosis. 85 Diffuse Infantile Fibromatosis. 90 Desmoid-Type Fibromatosis . 92 Benign Fibrous Histiocytoma (Dermatofibroma). 98 xi Tumors of the Soft Tissues Non-neural Granular Cell Tumor. 104 Neurothekeoma . 104 Plexiform Fibrohistiocytic Tumor. 110 Superficial Acral Fibromyxoma . 113 Superficial Angiomyxoma (Cutaneous Myxoma). 118 Intramuscular Myxoma. 125 Juxta-articular Myxoma. 128 Aggressive Angiomyxoma . 128 Angiomyofibroblastoma. 135 Cellular Angiofibroma. 136 3. Fibroblastic/Myofibroblastic Neoplasms with Variable Biologic Potential.