An Insight Into Internal Resorption
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Establishment of a Dental Effects of Hypophosphatasia Registry Thesis
Establishment of a Dental Effects of Hypophosphatasia Registry Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of The Ohio State University By Jennifer Laura Winslow, DMD Graduate Program in Dentistry The Ohio State University 2018 Thesis Committee Ann Griffen, DDS, MS, Advisor Sasigarn Bowden, MD Brian Foster, PhD Copyrighted by Jennifer Laura Winslow, D.M.D. 2018 Abstract Purpose: Hypophosphatasia (HPP) is a metabolic disease that affects development of mineralized tissues including the dentition. Early loss of primary teeth is a nearly universal finding, and although problems in the permanent dentition have been reported, findings have not been described in detail. In addition, enzyme replacement therapy is now available, but very little is known about its effects on the dentition. HPP is rare and few dental providers see many cases, so a registry is needed to collect an adequate sample to represent the range of manifestations and the dental effects of enzyme replacement therapy. Devising a way to recruit patients nationally while still meeting the IRB requirements for human subjects research presented multiple challenges. Methods: A way to recruit patients nationally while still meeting the local IRB requirements for human subjects research was devised in collaboration with our Office of Human Research. The solution included pathways for obtaining consent and transferring protected information, and required that the clinician providing the clinical data refer the patient to the study and interact with study personnel only after the patient has given permission. Data forms and a custom database application were developed. Results: The registry is established and has been successfully piloted with 2 participants, and we are now initiating wider recruitment. -

The Cat Mandible (II): Manipulation of the Jaw, with a New Prosthesis Proposal, to Avoid Iatrogenic Complications
animals Review The Cat Mandible (II): Manipulation of the Jaw, with a New Prosthesis Proposal, to Avoid Iatrogenic Complications Matilde Lombardero 1,*,† , Mario López-Lombardero 2,†, Diana Alonso-Peñarando 3,4 and María del Mar Yllera 1 1 Unit of Veterinary Anatomy and Embryology, Department of Anatomy, Animal Production and Clinical Veterinary Sciences, Faculty of Veterinary Sciences, Campus of Lugo—University of Santiago de Compostela, 27002 Lugo, Spain; [email protected] 2 Engineering Polytechnic School of Gijón, University of Oviedo, 33203 Gijón, Spain; [email protected] 3 Department of Animal Pathology, Faculty of Veterinary Sciences, Campus of Lugo—University of Santiago de Compostela, 27002 Lugo, Spain; [email protected] 4 Veterinary Clinic Villaluenga, calle Centro n◦ 2, Villaluenga de la Sagra, 45520 Toledo, Spain * Correspondence: [email protected]; Tel.: +34-982-822-333 † Both authors contributed equally to this manuscript. Simple Summary: The small size of the feline mandible makes its manipulation difficult when fixing dislocations of the temporomandibular joint or mandibular fractures. In both cases, non-invasive techniques should be considered first. When not possible, fracture repair with internal fixation using bone plates would be the best option. Simple jaw fractures should be repaired first, and caudal to rostral. In addition, a ventral approach makes the bone fragments exposure and its manipulation easier. However, the cat mandible has little space to safely place the bone plate screws without damaging the tooth roots and/or the mandibular blood and nervous supply. As a consequence, we propose a conceptual model of a mandibular prosthesis that would provide biomechanical Citation: Lombardero, M.; stabilization, avoiding any unintended (iatrogenic) damage to those structures. -

Feline Tooth Resorption Feline Odontoclastic Resorptive Lesions (FORL)
Feline Tooth Resorption Feline Odontoclastic Resorptive Lesions (FORL) What is tooth resorption? Tooth resorption is a destructive process that eats away at teeth and is quite common in cats. Up to 50% of cats over the age of 8 will have resorptive lesions. Of those 50% with lesions, 50% of them will have more than one. This process can be very painful, and due to the nature of the cat, many will not show obvious signs of pain. These lesions will often require immediate treatment. Feline tooth resorption does progress and will require treatment to avoid pain and loss of function. This process is not necessarily preventable, but studies do show that cats who do not receive oral hygiene care are at an increased risk of development of resorptive lesions. Feline patients diagnosed with Feline Immunodeficiency Virus and Feline Leukemia Virus are also more likely to develop lesions. Despite the health status of your cat, it is important to know tooth resorption is a common and treatable disease. What causes tooth resorption? Tooth resorption is an idiopathic disease of the teeth. This means that the cause is unknown. We do know odontoclasts, the cat’s own cells, begin to destroy the structure of the tooth. Sometimes resorption will be associated with a tooth root abscess, although this is uncommon. What are the clinical signs of this? Cats with tooth resorption will often have inflammation of the gum tissue surrounding the affected tooth. Your veterinarian will comment on the teeth and gums during the oral part of the physical examination. Even though an oral exam is done, many of these lesions are below the gum line and require dental radiography to fully diagnose. -

Feline Alveolar Osteitis Treatment Planning: Implant Protocol with Osseodensification and Early Crown Placement Rocco E
Feline Alveolar Osteitis Treatment Planning: Implant Protocol with Osseodensification and Early Crown Placement Rocco E. Mele DVM1, Gregori M. Kurtzman, DDS, MAGD, DICOI,DIDIA2 1 Eastpoint Pet Clinic, Tucson, A, USA 2 Silver Spring, MD, USA Abstract: Feline dental implants are becoming a predictable and viable treatment option for the replacement of lost canines due to maxillary Alveolar Osteitis (AO) a painful condition, commonly experienced by a growing number of cats. Surgical extraction and debridement remains the treatment of choice for this complex inflammatory process. However, future complications can be a common sequela of maxillary canine loss. This case will demonstrate the successful surgical extraction of a maxillary canine with implant placement following the osseodensification protocol and utilizing the sockets osteitis buttressing bone formation to promote a positive result with final crown restoration 13 weeks following implant placement. Introduction: Alveolar Osteitis (AO) is a chronic inflammatory process more often diagnosed in maxillary canine sockets of the feline patient. Clinical presentation may include oral pain, bleeding, periodontitis, tooth resorption (ORL), and alveolar buccal bone changes.1-5 Clinical Features: A presumptive diagnosis of (AO) is made on the awake patient, documenting clinical features such as; gingivitis with soft tissue swelling, gingival mucosal erythema, buccal bone expansion, and coronal extrusion. (Figure 1) Radiographic Features: Radiographic changes are identified under general anesthesia. These bony changes and pathology may include; deep palatal probing (Figure 2 red), alveolar bone expansion (Figure 2 green), buttressing condensing bone (Figure 2 blue) and a mottled osseous appearance mimicking rough, large trabeculae (Figure 2 yellow) Osseodensification (OD): OD is a novel biomechanical bone preparation technique for dental implant placement to improve bone quality by increasing its density utilizing Densah burs. -

Feline Tooth Resorption Lesions
METROWEST VETERINARY ASSOCIATES, INC. 207 EAST MAIN STREET, MILFORD, MA 01757 (508) 478-7300 online @ www.mvavet.com Feline Tooth Resorption Lesions Feline tooth resorption lesions (aka RLs) are one of the most common causes of tooth loss in cats, with as many as 65% of domestic cats affected. The lesions start at, or even below the gum line, and may affect any tooth. If untreated, RLs can lead to further periodontal disease, oral pain, infections and potentially, problems in other areas of the body. Because we don’t know what causes tooth resorption, we do not know how to prevent it. The presentation of RLs is variable. In brief, teeth are composed of enamel on the outside, dentin below it and pulp on the inside. In a stage 1 lesion, a defect in the enamel is seen. Stage 2 lesions affect the enamel and dentin beneath it. In stage 3 lesions, the tooth is affected down to the pulp. Stage 4 RLs the crown of the tooth has been eroded or fractured ( ). Resorptive lesions may also occur entirely below the gum line, with damage to the roots of the tooth while the tooth appears normal above the gum line. For this reason, dental x-rays are vital during dental procedures to help identify affected teeth As cats have more nerve endings in their teeth than people, RLs can be very painful to the cat. Signs may include difficulty chewing (especially dry food), apparent decrease in appetite, halitosis (bad breath), drooling, inflamed gums, oral bleeding, vomiting and/or decreased grooming. -

Idiopathic Tooth Resorption in Dogs
IDIOPATHIC TOOTH RESORPTION IN DOGS Tooth resorption is a progressive, potentially pain- calized gingivitis, asymmetrical accumulation of cal- ful and poorly understood disease that affects many culus/plaque, intrinsic staining of the crowns (usually species. The disease has been well recognized in peo- a pinkish hue). Dental radiographs are essential to ple and cats but not in canines. This disease was once diagnosing and determining how and when to treat thought rare but now is more commonly diagnosed teeth affected by resorptive lesions. Tooth resorp- in dogs. tive lesions are progressive and painful. They require treatment when above the attached gingiva. Dental Juvenile teeth unlike adult teeth are resorbed and radiographs help determine the extent and type of shed. It is not understood why in some dogs and cats, tooth resorptive lesions (type 1, 2 or 3), which dictates odontoclasts, the cells responsible for the resorptive the treatment with either extraction or crown ampu- process, are activated. Tooth resorption can occur in tation. any breed and affect any dog at any age, but typically tooth resorption is observed in older dogs. There are three types of tooth resorption each type diagnosed based on their radiographic appear- Tooth resorption below the attached gingiva is ance. Good positioning and quality of radio- thought not to be painful (not reported painful graphs are absolutely essential. Diagnosis of by people) but lesions above the attached gin- type of tooth resorption is based upon the giva are known to be extremely painful. It can overall radio-density of the tooth, surround- be very difficult to visualize a lesion above the ing bone and appearance of the periodon- attached gingiva. -

THE YOUNG and the OLD: NORMAL and VARIATIONS from NORMAL Judy Rochette DVM, FAVD, Dipl AVDC
THE YOUNG AND THE OLD: NORMAL AND VARIATIONS FROM NORMAL Judy Rochette DVM, FAVD, Dipl AVDC The majority of notable findings in the oral cavity of the young pet are related to its formation and development, as well as the development and eruption of teeth, whereas senior pet variations reflect the gradual aging of the dental hard tissues and their supporting structures. The head, face, and oral cavity are some of the first structures to manifest in the developing embryo. The upper face forms from the neural tube while the lower face forms from branchial arches. The oral mucosa and upper alimentary tract form from the ectodermal layers. The mesenchymal layer provides the cells which will become subcutaneous tissues and the bone and supporting apparatus for the teeth. The teeth themselves are both ectodermal and mesodermal in origin. Any phenotypic variation from the "wild type" of head, or any genetic anomaly which affects the ectoderm or mesodermal tissues will likely have an effect on the oral cavity. Some of these anomalies have been intentionally introduced to create new "breeds". BRACHYCEPHALIC SYNDROME Brachycephalic syndrome is a set of dysfunctional anatomical airway variations familiar to veterinarians who deal with Bulldogs, Pugs and Boston Terriers but this syndrome is also a problem in Persian, Himalayan and Burmese cats. Stenotic nares, an elongated soft palate, hypoplastic trachea and everted laryngeal saccules can all inhibit respiration. Mouth breathing, stertor, exercise intolerance and collapse after exercise can be seen. Early surgical intervention to open the nares and shorten the palate will often arrest the development of everted saccules, lower respiratory tract inflammation and cardiac stress. -

Tooth Resorption in Dogs
BOARD-CERTIFIED Fraser Hale, DVM, FAVD, DipAVDC VETERINARY DENTAL SPECIALIST DENTAL AND ORAL SURGERY FOR PETS This informational page is an attempt to describe a complex subject in limited space. It should be considered to be very introductory. More in-depth discussions of this and many other subjects can be found on the Old CUSP Articles page at www.toothvet.ca. You are encouraged to visit and make use of the resources there and elsewhere on my website. Tooth Resorption in Dogs While it has long been recognized that many cats that allows the tooth to quickly fall out and the suffer from tooth resorption, we are increasingly tissues to quickly heal. finding this mysterious condition affecting dogs. Is With the adult teeth, the resorption can start the incidence truly increasing or are we just anywhere on the root(s) of the teeth and can take a recognizing the condition more now because we are number of forms. From left to right, the radiographs looking for it? Regardless, tooth resorption in dogs below show (a) some normal right lower molars and is now common and should always be looked for. premolars, (b) advanced resorption of these same Consider the primary or baby teeth. In many species, teeth in another dog with loss of distinction between including humans, dogs and cats, primary (baby) root and bone, (c) similar advanced resorption of the teeth erupt early in life but last a short while only to left upper 4th premolar, (d) moderate to advanced be replaced by the adult (permanent) teeth which are resorption of the right lower premolars with a clear intended to remain in place for life. -
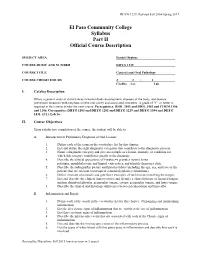
El Paso Community College Syllabus Part II Official Course Description
DHYG 1239; Revised Fall 2016/Spring 2017 El Paso Community College Syllabus Part II Official Course Description SUBJECT AREA Dental Hygiene COURSE RUBIC AND NUMBER DHYG 1239 COURSE TITLE General and Oral Pathology COURSE CREDIT HOURS 2 2 : 1 Credits Lec Lab I. Catalog Description Offers a general study of disturbances in human body development, diseases of the body, and disease prevention measures with emphasis on the oral cavity and associated structures. A grade of "C" or better is required in this course to take the next course. Prerequisites: BIOL 2401 and BIOL 2402 and CHEM 1306 and 1106. Corequisites: DHYG 1103 and DHYG 1201 and DHYG 1219 and DHYG 1304 and DHYG 1431. (2:1). Lab fee. II. Course Objectives Upon satisfactory completion of the course, the student will be able to: A. Introduction to Preliminary Diagnosis of Oral Lesions 1. Define each of the terms in the vocabulary list for this chapter. 2. List and define the eight diagnostic categories that contribute to the diagnostic process. 3. Name a diagnostic category and give an example of a lesion, anomaly, or condition for which this category contributes greatly to the diagnosis. 4. Describe the clinical appearance of Fordyce=s granules (spots), torus palatinus, mandibular tori, and lingual varicosities, and identify them on a slide. 5. Describe the radiographic picture and historical data (including the age, sex, and race of the patient) that are relevant to periapical cementl dysplasia (cementoma). 6. Define Avariant of normal@ and give three examples of such lesions involving the tongue. 7. List and describe the clinical characteristics and identify a clinical picture of fissured tongue, median rhomboid glossitis, geographic tongue, ectopic geographic tongue, and hairy tongue. -

Pathological External Resorption Caused by Impacted Tooth
Prog Health Sci 2015, Vol 5, No2 Pathological external resorption impacted tooth Pathological external resorption caused by impacted tooth Dryl D.1*, Słowik-Sułkowski M.1, Szarmach J.1, Karaszewski J.1, Stankiewicz A.2 1. Department of Oral Surgery, Medical University of Białystok, Białystok, Poland 2. Specialist Dental Center Ltd, Medical University of Białystok, Białystok, Poland ABSTRACT ___________________________________________________________________________ Tooth resorption can be associated with resorption of a molar tooth due to pressure from an physiological or pathological loss of dental hard impacted tooth. A considerable loss of hard tissues tissues. The process of resorption is usually and impossibility to perform conservative treatment asymptomatic and may lead to substantial tooth caused the loss of two molars. Key words: external damage. We presented a case of pathological resorption, impacted tooth ___________________________________________________________________________ *Corresponding author: Dorota Dryl Department of Oral Surgery, Medical University of Białystok ul. M.C.Skłodowskiej 24a, 15-276 Białystok, Poland Tel.: 85 748 57 69; Fax: 85 748 57 71 e-mail:[email protected] Received: 10.05.2015 Accepted: 04.08.2015 Progress in Health Sciences Vol. 5(2) 2015 pp 241-244 © Medical University of Białystok, Poland 241 Prog Health Sci 2015, Vol 5, No2 Pathological external resorption impacted tooth INTRODUCTION result of pathological resorption caused by an impacted tooth. Resorption is the process associated with physiological or pathological loss of dental hard Case report tissues. Apart from physiological resorption in milk teeth there is also a pathological process observed A male patient, 37, presented himself at the both in primary and permanent dentition [1]. -

Clinicalpractice
Clinical P RACTIC E External Cervical Resorption Associated with Traumatic Occlusion and Pyogenic Granuloma Contact Author Rouzbeh Vossoughi, DDS; Henry H. Takei, DDS, MS Dr. Vossoughi Email: rwosoughi@ yahoo.com ABSTRACT This report describes a rare situation in which external cervical resorption was associ- ated with gingival enlargement (pyogenic granuloma) in the upper left central incisor (tooth 21) in a 28-year-old man. Tissue from the lesion was examined histopathologically; periodontal, endodontic and restorative treatments were performed; and the occlusal disharmony, which had resulted in traumatic occlusion, was corrected. Three years after these treatments, the gingiva is normal and healthy and there is no sign of recurrence of the pathologic enlargement. The patient’s periodontal condition is now routinely evalu- ated. In the presence of gingival enlargement resulting from inflammation, traumatic occlusion can cause progressive external root resorption. For citation purposes, the electronic version is the definitive version of this article: www.cda-adc.ca/jcda/vol-73/issue-7/625.html yogenic granuloma is a reactive lesion tion may occur in 2 patterns: the resorption that represents an overexuberant reac- may start at the root apex and progress coron- Ption by connective tissue to a known ally or it may occur immediately apical to the stimulus or injury. It appears as a red mass be- cementoenamel junction (CEJ)6 below the epi- cause it is composed of hyperplastic granula- thelial attachment and coronal to the alveolar tion tissue in which capillaries are prominent. process, which is the zone of connective tissue It is commonly seen on the gingiva, where it is attachment.