End-To-End SARS-Cov-2 Transmission Risks in Sport
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sport and the Media
3068-Ch10.qxd 12/3/02 7:52 PM Page 184 10 Sport and the Media DAVID STEAD Overview → Context and key issues → The sportmedia partnership → The media sports product: influences and outcomes → The media sport audience → Media sport: where to now? CONTEXT AND KEY ISSUES to income generated directly or indirectly from the media. The way in which sport In many ways, both today’s sport and the fills newspaper pages and television and media are classic outcomes and, indeed, radio schedules bears testimony to the icons of the far-reaching social, economic influence it has on the structure and extent and technological change that charac- of media activity. terised the twentieth century. Each has However, partnerships are not always developed extensively and rapidly as a equal, stable or constructive for those major global industry. Each plays a signifi- involved. In this chapter, consideration will cant part in structuring and informing be given to a number of themes and issues people’s lives. Each has a global as well as that characterise the link between sport and more local scope of operation and has the the media. Difficulties and tensions exist structures and practices to reflect this. but ultimately a media sports product Importantly, they are two industries tied emerges whether it is, for example, a live TV together in complex networks of relation- broadcast of the Olympic Games or a news- ships. Their respective histories of develop- paper report on a local rugby match. This ment have been fuelled and influenced by raises a series of issues about the nature of the dynamics of this partnership. -

End-To-End SARS-Cov-2 Transmission Risks in Sport: Current Evidence and Practical Recommendations
REVIEW End-to-end SARS-CoV-2 transmission risks in sport: Current evidence and practical recommendations B Jones,1,2,3,4,5 PhD; G Phillips,1,2,6 MBChB, MSc; F Valeriani,7 PhD; T Edwards,8 PhD; ER Adams,8 PhD; L Bonadonna,9 PhD; RJ Copeland,10 PhD; MJ Cross,11,12 PhD; C Dalton,10 PhD; L Hodgson,13,14 PhD; A Jimenez,10,15 PhD; SP Kemp,16,17 MBBS, MSc; J Patricios,18 MBBCh FFSEM (UK); V Romano Spica,7 PhD; KA Stokes,11,16 PhD; M Weed,19 PhD; C Beggs,1 PhD 1 Carnegie Applied Rugby Research (CARR) centre, Carnegie School of Sport, Leeds Beckett University, Leeds, UK 2 England Performance Unit, The Rugby Football League, Leeds, UK 3 Leeds Rhinos Rugby League club, Leeds, UK 4 Division of Exercise Science and Sports Medicine, Department of Human Biology, Faculty of Health Sciences, the University of Cape Town and the Sports Science Institute of South Africa, Cape Town, South Africa 5 School of Science and Technology, University of New England, Armidale, NSW, Australia. 6 Hull Kingston Rovers, Hull, UK 7 Public Health Unit, Department of Movement, Human and Health Sciences; University of Rome “Foro Italico”, Rome, Italy 8 Department of Tropical Disease Biology, Liverpool School of Tropical Medicine, Pembroke Place, Liverpool, L3 5QA, UK 9 Italian National Institute of Health, Rome Italy 10 Advanced Wellbeing Research Centre, Sheffield Hallam University, UK 11 University of Bath, Bath, UK 12 Premiership Rugby, Twickenham, UK 13 The Football Association, St George’s Park, Burton-Upon-Trent, UK. -

Rugby League As a Televised Product in the United States of America
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Professional Projects from the College of Journalism and Mass Communications, College Journalism and Mass Communications of 7-31-2020 Rugby League as a Televised Product in the United States of America Mike Morris University of Nebraska-Lincoln, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/journalismprojects Part of the Broadcast and Video Studies Commons, Communication Technology and New Media Commons, Journalism Studies Commons, and the Mass Communication Commons Morris, Mike, "Rugby League as a Televised Product in the United States of America" (2020). Professional Projects from the College of Journalism and Mass Communications. 23. https://digitalcommons.unl.edu/journalismprojects/23 This Article is brought to you for free and open access by the Journalism and Mass Communications, College of at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Professional Projects from the College of Journalism and Mass Communications by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Rugby League as a Televised Product in the United States of America By Mike Morris Abstract Rugby league is a form of rugby that is more similar to American football than its more globally popular cousin rugby union. This similarity to the United States of America’s most popular sport, that country’s appetite for sport, and its previous acceptance of foreign sports products makes rugby league an attractive product for American media outlets to present and promote. Rugby league’s history as a working-class sport in England and Australia will appeal to American consumers hungry for grit and authenticity from their favorite athletes and teams. -

Catapult Signs League-Wide Deal with the UK's Rugby Football League
5 December 2017 Catapult Signs League-Wide Deal with the UK’s Rugby Football League Catapult Group International Ltd (ASX: CAT, ‘Catapult’) is pleased to announce the signing of a new partnership with the Rugby Football League (RFL), as the RFL embrace Catapult’s world leading athlete performance technology to enhance its existing innovation credentials. The RFL is the governing body for rugby league in England – covering the England National Rugby League team and the Northern Hemisphere’s elite rugby league competition, the Betfred Super League. Deal highlights - 390 Catapult S5 elite tracking units. - Teams covered include the England National Rugby League Team and all 12 teams in the Super League. - Establishes framework for Catapult and the Super League to explore data commercialisation opportunities through live match-day tracking services. Under the agreement, Catapult have supplied 390 S5 tracking units during 2017 and will see the implementation of Catapult’s market-leading wearable athlete performance monitoring platform to all 12 teams in the Super League and the England National Rugby League team. These will be used in both training and competition matches in 2018. The agreement will also explore live match-day tracking using Catapult’s ClearSky stadia technology. For the 2018 Super League season, the RFL and Catapult will investigate data commercialisation opportunities to use live metrics supported by Catapult. Commenting on the partnership with Catapult, Roger Draper, Chief Commercial Officer at the Rugby Football League, said: “Catapult’s wearable analytics will be deployed to all 12 of our Super League teams, having already been used by the England Men’s National Team at the Rugby League World Cup 2017. -

The Professionalisation of British Darts, 1970 – 1997
From a Pub Game to a Sporting Spectacle: The professionalisation of British Darts, 1970 – 1997 Leon Davis Abstract: Various sport scholars have noted the transition of sports from amateur leisure pastimes to professionalised and globalised media sporting spectacles. Recent developments in darts offer an excellent example of these changes, yet the sport is rarely discussed in contemporary sports studies. The only sustained theoretical research on darts focuses primarily on the origins of the sport in its nostalgic form as a working-class, pub taproom pastime in England. This article critically examines the transformation of darts from a leisurely game to a professional sport between the 1970s and the 1990s. The change was enabled by the creation of the British Darts Organisation (BDO) and the introduction of television broadcasting, which together fed a continual process of professionalisation. Initially, this article discusses both the concept of professionalisation and similar developmental changes in a selection of English sports. Following this, via selected interviews, documentary analysis and archival information, the reasons behind the split in darts are explicated, shedding light on how the BDO did not successfully manage the transformation and the sport split into two governing bodies, from which the Professional Darts Corporation (PDC), the sport’s most successful organisation in the present day, has emerged to dominate the world of televised darts. Keywords: Darts, professionalisation, television, game, sport Introduction For much of the twentieth century, darts was a predominantly working-class game played by local people and top-ranked players in British pubs and social clubs. However, since the 1970s, the game has rapidly changed from a communal game into a sporting entertainment spectacle. -

The All Golds and the Advent of Rugby League in Australasia
"ALL THAT GLITTERS" THE ALL GOLDS AND THE ADVENT OF RUGBY LEAGUE IN AUSTRALASIA. A thesis submitted in partial fulfilment of the requirements for the Degree of Master of Arts in History in the University of Canterbury by Jo Smith This thesis is dedicated toMu.m&Dad University of Canterbury 1998 CONTENTS PAGE LIST OF PLATES 11 LIST OF TABLES Ill ABBREVIATIONS l1l ACKNOWLEDGEMENTS IV PREFACE V ABSTRACT Vil CHAPTER: I A WORKING-CLASS GAME: ORIGINS OF RUGBY LEAGUE IN ENGLAND I II AN ENTREPRENEURIAL VENTURE: GENESIS OF THEALL GOLDS 21 III A WORKING-CLASS REVOLT: IMPACT OF THE ALL GOLDS IN AUSTRALIA 49 IV CLASH OF THE CODES: THE ALL GOLDS. IN BRITAIN 67 V THE ALL GOLQS RETURN: FOUNDATIONS OF RUGBY LEAGUE IN AUSTRALASIA 99 CONCLUSION 125 APPENDICES 128 BIBLIOGRAPHY 154 ll LIST OF PLATES PLATES After page: Plate 1. Albert Henry Baskiville. 21 Plate 2. The New Zealand Professional Rugby Team in Sydney. 63 Plate 3. The New Zealand Professional Football Team 1907. 67 Plate 4. The 'All Blacks' Autographs. 67 Plate 5. The New Zealand Footballers. 68 Plate 6. 'All Blacks' First Practice at Headingley. 71 Plate 7. Follow Up The Kick For 'On Side'. 71 Plate 8. The New Zealand Footballers. 71 Plate 9. A Group At Leeds. 71 Plate 10. The 'All Blacks' Chanting Their War Cry At Huddersfield. 74 Plate 11. The 'All Blacks' Win At Huddersfield. 74 Plate 12. New Zealand's Struggle At Oldham. 78 Plate 13. Red Rose Better Than All Black. 80 Plate 14. New Zealand Lost The First Test. -

Issued Decision UK Anti-Doping and Daniel Bridge
Issued Decision UK Anti-Doping and Daniel Bridge Disciplinary Proceedings under the Anti-Doping Rules of the Rugby Football League This is an Issued Decision made by UK Anti-Doping Limited (‘UKAD’) pursuant to the Anti-Doping Rules (the ‘ADR’) of the Rugby Football League (‘RFL’). It concerns a violation of the ADR committed by Mr Daniel Bridge and records the applicable Consequences. Capitalised terms used in this Decision shall have the meaning given to them in the ADR unless otherwise indicated. Background and Facts 1. The RFL is the national governing body for the sport of rugby league in England. UKAD is the National Anti-Doping Organisation for the United Kingdom. 2. Mr Bridge is a 27-year old rugby league player who was registered to play for Oldham RLFC. At all material times in this matter, Mr Bridge was subject to the jurisdiction of the RFL and bound to comply with the ADR. Pursuant to the ADR, UKAD has results management responsibility in respect of all players subject to the jurisdiction of the RFL. 3. On 16 February 2020, UKAD collected an In-Competition urine Sample from Mr Bridge following a Championship match between Whitehaven RLFC and Oldham RLFC at Recreation Ground, Coach Road, Whitehaven. The Sample was separated into two bottles which were given the reference numbers A1157229 (the ‘A Sample’) and B1157229 (the ‘B Sample’). 4. Both Samples were transported to the World Anti-Doping Agency (‘WADA’) accredited laboratory, the Drug Control Centre, King’s College London (the ‘Laboratory’). The A Sample was analysed in accordance with the procedures set out in WADA’s International Standard for Laboratories. -

The Rugby League Dividend
THE RUGBY LEAGUE DIVIDEND ECONOMIC AND SOCIAL IMPACT OF RUGBY LEAGUE July 2019 Dr Nicolas Scelles Manchester Metropolitan University T: 0161 247 3949 E: [email protected] 2 CONTENTS AUTHORS AND OTHER CONTRIBUTORS TO THE RESEARCH 4 HEADLINES 5 FOREWORD 6 INTRODUCTION 10 METHODOLOGY 12 RESULTS 16 ECONOMIC IMPACT 18 ECONOMIC IMPORTANCE 24 SOCIAL IMPACT 26 SOCIAL RETURN ON INVESTMENT (SROI) 28 SOCIAL CAPITAL 30 CONCLUSION 41 REFERENCES 42 APPENDICES 44 3 AUTHORS AND OTHER CONTRIBUTORS TO THE RESEARCH AUTHORS DR NICOLAS SCELLES PROF JONATHAN GRIX PROF MARC JONES DR THOMAS HOSTLER (Principal Investigator) Other contributors to the research GABRIELLE SALOMON (all PhD candidates at MMU) LUCI SMITH DANIEL GALLANT 4 HEADLINES The annual economic impact of the English clubs and central events is estimated at more than £141 MILLION Community clubs have economic importance for their territory, maintaining economic relationships with local companies and providing employment and remuneration. The social impact of the sport of Rugby League on players and volunteers is estimated at more than £185 MILLION Every £ spent by Rugby League community clubs in sport generates a social return of £4.08. £1 = £4.08 The social capital of the sport of Rugby League is demonstrated by the positive elements highlighted by volunteers as well as members of the communities who do not identify as fans of Rugby League in terms of social cohesiveness, identity, aspiration and role models. 5 HEADLINES FOREWORD Shaun Wane is the England Head Coach “I ended up going to Lorraine’s house (his and a former player and highly successful then girlfriend) - her mum and dad put me coach of Super League club Wigan Warriors. -

Economic and Social Impact of Rugby League
THE RUGBY LEAGUE DIVIDEND ECONOMIC AND SOCIAL IMPACT OF RUGBY LEAGUE July 2019 Dr Nicolas Scelles Manchester Metropolitan University T: 0161 247 3949 E: [email protected] CONTENTS AUTHORS AND OTHER CONTRIBUTORS TO THE RESEARCH 4 HEADLINES 5 FOREWORD 6 INTRODUCTION 10 METHODOLOGY 12 RESULTS 16 ECONOMIC IMPACT 18 ECONOMIC IMPORTANCE 24 SOCIAL IMPACT 26 SOCIAL RETURN ON INVESTMENT (SROI) 28 SOCIAL CAPITAL 30 CONCLUSION 41 REFERENCES 42 APPENDICES 44 2 3 AUTHORS AND OTHER CONTRIBUTORS TO THE The annual economic impact of the English clubs RESEARCH and central events is estimated at more than £141 MILLION AUTHORS Community clubs have economic importance for their territory, maintaining economic relationships with local companies and providing employment and remuneration. The social impact of the sport of Rugby League on players and volunteers is estimated at more than DR NICOLAS SCELLES PROF JONATHAN GRIX PROF MARC JONES DR THOMAS HOSTLER (Principal Investigator) £185 MILLION Other contributors to the research Every £ spent by Rugby League community clubs in GABRIELLE SALOMON sport generates a social return of £4.08. (all PhD candidates at MMU) LUCI SMITH DANIEL GALLANT £1 = £4.08 The social capital of the sport of Rugby League is demonstrated by the positive elements highlighted by volunteers as well as members of the communities who do not identify as fans of Rugby League in terms of social cohesiveness, identity, aspiration and role models. 4 5 HEADLINES FOREWORD Sport has a very special place in the social National sporting organisations have charitable foundations play at the heart tournament played in iconic venues in fabric of our nation. -

Bulletin 61.Indd
THE OFFICIAL MAGAZINE OF THE RFL | ISSUE 61 RRRRIIISISSSIIININNNGGGG T TTTOOOO TTTTHHHHEEEE T TTTOOOOPPPP QUE STION TIME GO ING GLOBAL RUGBY LEAGUE BULLETIN October 2009 CONTENTS 5 Media Matters SEE THE SUPER POWERS OF INTERNATIONAL RUGBY 6 Grand Designs North Eastern LEAGUE CLASH THIS OCTOBER AND NOVEMBER Promise 8 12 Passing On Their Experience 14 Higgins At The Helm 15 Super Human! 18 Taking Aim 19 Euro-vision Rising To The Top 10 20 Promising Signs 24 Helping The Grass Roots Thrive 26 Learning With The Skolars 27 Making The Grade One Hell Of A WeekendQuestion 28 Tales From Wembley PgTime 16 & 17 16 Friday 23rd October Saturday 31st October Saturday 14th November Published by the Rugby League Services Department of the RFL. ENGLAND V FRANCE ENGLAND V AUSTRALIA The RFL, The Zone, St Andrews Road, Huddersfield, HD1 6PT. CubsGoing To Lions KEEPMOAT STADIUM, DONCASTER DW STADIUM, WIGAN Tel - 01484 448000 | Fax - 01484 545582, Global 22 Saturday 24th October Saturday 7th November FINAL Email - [email protected] | Internet - www.rfl.uk.com Pg 26 & 27 AUSTRALIA V NEW ZEALAND ENGLAND V NEW ZEALAND ELLAND ROAD STADIUM, LEEDS THE STOOP, LONDON GALPHARM STADIUM, HUDDERSFIELD The views expressed in this publication do not necessarily reflect those of the RFL Board of Directors. FAMILY TICKET OFFER GROUP STAGE FINAL OFFER* DISCOUNT RECEIVED ON Contributors - Tom Hoyle, Phil Caplan, Neil Barraclough, swpix.com, Dave Williams, John FOR 2 ADULTS AND OFFER Connaughton, Phil Hodgson, Dave Burke, Dave Woods, Callum Irving, Alex Ferguson 2 JUNIOR TICKETS for A FINAL TICKET WHEN £40 1010 for99 £10£10 PURCHASING ANY GROUP GAME If you are interested in advertising in the Rugby League Bulletin, please contact - [email protected] NOTE: ALL TICKET OFFERS Main Cover Photograph - The Angel of the North © The Rugby Football League Ltd 2009 Designed by - Tom Hoyle Tickets from £20 adults, £10 conc. -
Bulletin 69.Indd
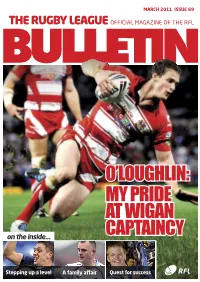
MARCH 2011 ISSUE 69 THE RUGBY LEAGUE OFFICIAL MAGAZINE OF THE RFL O’LOUGHLIN: MY PRIDE AT WIGAN on the inside… CAPTAINCY Stepping up a level A family affair Quest for success RAISE FUNDS FOR YOUR CLUB 14 Stepping up a level CARNEGIE CHALLENGE CUP FINAL 27th AUGUST 2011 £31 ticket for £26 on the upgrade offer - for every 50 sold your club will get a return of £250 or CONTENTS £51 ticket for £41 on the upgrade 5 Media Matters offer - for every 50 sold your club 6 The best of the best will get a return of £500 8 Managing the Lions plus 9 Southern expansion ticket and hotel offers 10 Destination Wembley offering £2000 cashback 16 O’Loughlin: 12 New Wheelchair structure My pride at Wigan 22 A family 20 A call to arms captaincy affair 21 Summer lovin’ 24 Higginshaw’s big idea 26 Grassroots flourishing 30 Academy 2011 Castleford Lock Lane Hull East Leigh East Hull Embassy MARCH 2011 ISSUE 69 THE RUGBY LEAGUE OFFICIAL MAGAZINE OF THE RFL Outwood Grange Halifax RLFC Myton Warriors Crigglestone All Blacks Catterick Garrison LIMITED O’LOUGHLIN: AVAILABILITY MY PRIDE Get in quick! AT WIGAN on the inside… CAPTAINCY Milnrow Cobras Holderness Vikings Stepping up a level A family affair Quest for success for more information contact 27 Quest for Ray Tennant success T: 07595 520 338 ray.tennant@rfl.uk.com Bev Coleman T: 07595 520 578 bev.coleman@rfl.uk.com Ryburn Valley High School Spen Valley INSIDE THIS ISSUE MEDIA MATTERS .... with Neil Barraclough Welcome to the first Rugby League Bulletin daylight second, and everything else well of 2011 ... -

Catapult Signs League-Wide Deal with the UK's Rugby Football League
5 December 2017 Catapult Signs League-Wide Deal with the UK’s Rugby Football League Catapult Group International Ltd (ASX: CAT, ‘Catapult’) is pleased to announce the signing of a new partnership with the Rugby Football League (RFL), as the RFL embrace Catapult’s world leading athlete performance technology to enhance its existing innovation credentials. The RFL is the governing body for rugby league in England – covering the England National Rugby League team and the Northern Hemisphere’s elite rugby league competition, the Betfred Super League. Deal highlights - 390 Catapult S5 elite tracking units. - Teams covered include the England National Rugby League Team and all 12 teams in the Super League. - Establishes framework for Catapult and the Super League to explore data commercialisation opportunities through live match-day tracking services. Under the agreement, Catapult have supplied 390 S5 tracking units during 2017 and will see the implementation of Catapult’s market-leading wearable athlete performance monitoring platform to all 12 teams in the Super League and the England National Rugby League team. These will be used in both training and competition matches in 2018. The agreement will also explore live match-day tracking using Catapult’s ClearSky stadia technology. For the 2018 Super League season, the RFL and Catapult will investigate data commercialisation opportunities to use live metrics supported by Catapult. Commenting on the partnership with Catapult, Roger Draper, Chief Commercial Officer at the Rugby Football League, said: “Catapult’s wearable analytics will be deployed to all 12 of our Super League teams, having already been used by the England Men’s National Team at the Rugby League World Cup 2017.