Self-Care Toolkit
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Song & Music in the Movement
Transcript: Song & Music in the Movement A Conversation with Candie Carawan, Charles Cobb, Bettie Mae Fikes, Worth Long, Charles Neblett, and Hollis Watkins, September 19 – 20, 2017. Tuesday, September 19, 2017 Song_2017.09.19_01TASCAM Charlie Cobb: [00:41] So the recorders are on and the levels are okay. Okay. This is a fairly simple process here and informal. What I want to get, as you all know, is conversation about music and the Movement. And what I'm going to do—I'm not giving elaborate introductions. I'm going to go around the table and name who's here for the record, for the recorded record. Beyond that, I will depend on each one of you in your first, in this first round of comments to introduce yourselves however you wish. To the extent that I feel it necessary, I will prod you if I feel you've left something out that I think is important, which is one of the prerogatives of the moderator. [Laughs] Other than that, it's pretty loose going around the table—and this will be the order in which we'll also speak—Chuck Neblett, Hollis Watkins, Worth Long, Candie Carawan, Bettie Mae Fikes. I could say things like, from Carbondale, Illinois and Mississippi and Worth Long: Atlanta. Cobb: Durham, North Carolina. Tennessee and Alabama, I'm not gonna do all of that. You all can give whatever geographical description of yourself within the context of discussing the music. What I do want in this first round is, since all of you are important voices in terms of music and culture in the Movement—to talk about how you made your way to the Freedom Singers and freedom singing. -

Why Me Lord.P7
This book is designed for your personal reading pleasure and profit. It is also designed for group study. A leader’s guide with helps and hints for teachers and visual aids (Victor Multiuse Transparency Masters) is available from your local bookstore or from the publisher. Fifth printing, 1987 Most of the Scripture quotations in this book are from the King James Version of the Bible (KJV). Other quotations are from the Holy Bible: New International Version (NIV), © 1973, 1978, 1984, International Bible Society. Used by permission of Zondervan Bible Publishers; the New American Standard Bible (NASB), © the Lockman Foundation, 1960, 1962, 1963, 1968, 1971, 1972, 1973, 1975, 1977. Used by permission. Recommended Dewey Decimal Classification: 241.1 Suggested subject heading: THE WILL OF GOD IN CRISES Library of Congress Catalog Card Number 80-52947 ISBN: 0-89693-007-6 © 1981 by SP Publications, Inc. All rights reserved Printed in the United States of America VICTOR BOOKS A division of SP Publications, Inc. Wheaton, Illinois 60187 Dedication To the women in my life: Mary, my mother Emma, Pat, and Lillian, my sisters Cathy, my wife Lori, my daughter Gerrie, my editor Gloria, my secretary Anita, my typist Contents Preface 9 Part I—How to Live 1 Why? Why? Why? 13 2 The Choice Is Yours 22 3Triumph Out of Tragedy 28 Part II—How to Die 4 Life after All 39 5 Am I Normal? 45 6 Broken Hearts Do Heal 52 Part III—How to Help 7 How to Help a Grieving Friend 63 8 Helping a Friend Cope with a Terminal Illness 73 9 How to Explain Death to a Child 82 10 Making the Funeral Arrangements 90 11 After the Funeral Is Ove 98 12 Preparing for Your Own Death 105 13 Questions and Answers about Death— 112 Can a Christian Commit Suicide? 112 What Happens to People between Death and the Resurrection? 113 Will We Know Each Other in Heaven? 114 Is Dying Painful? 115 What Happens to Babies after Death? 116 What Is Heaven Like? 117 Preface How to live! How to die! We all need to know how to do that. -
Vol. 4 Issue 1
The Rincon Mountain MESSENGER Winter 2016 Volume 4, Issue 1 A Concert of the Arts The Rincon Mountain choir, let by Luke Smith, presented its holiday offering in early Inside this issu e: December. The Joy of Christmas: A Concert of the Arts featured a variety of sacred and popular music pieces along with other "treats." Artistic director Cindy Visser created visual introductions to each song, and there were original poetry and prose readings by Lois Christmas 1 Radtke and Rob Matte. Arie and Kylie Vande Geest performed piano solos, and the concert ended with a moving choral rendition of Silent Night. Kruis Korner 2 Hey Y’all! 3 Fire & Meat 3 A Word or Two 4 Trunk or Treat 4 One Take-Away 5 Arie Vande Geest playing a piano solo. The Rincon Mountain choir, led by Pastor Luke Smith. Missions 5 2015 Christmas Caroling Calendar 6 On a warm, sunny afternoon in mid-December, a small group of adults and children from Rincon Mountain visited Brookdale, a local memory-care facility, to sing Christmas carols and celebrate the birth of the Savior. As we sang the familiar lines, the residents joined in as well, even though many of them had trouble remembering basic information about themselves. Yet they hadn't forgotten those well-worn words, so together we filled the room with praises to Jesus. The sight caused one visitor (probably a family member of one of the residents) to cry quietly in the corner as she watched and whispered along. In between songs, we were able to give a short explanation of why Christ's birth is such amazing news for us today. -

1 Historical Romance Guide Alexander, Victoria
1 Historical Romance Guide Alexander, Victoria. “What Happens at Christmas.” Kensington Books. Camille, Lady Lydingham, knows precisely what she wants for Christmas--an official engagement to a handsome, dashing prince. Her very proper suitor expects a proper English family and the perfect Dickensian Christmas, which leaves the lovely widow with a slight problem. The last thing Camille wants is for the prince to meet her unconventional relatives. But with the aid of a troupe of actors, Camille intends to pull off a Christmas deception of massive proportions. At least until Grayson Elliott comes back into her live after an absence of twelve years. (Millworth Manor #1) Alexander, Victoria. “The Importance of Being Wicked.” Zebra. For Viscount Stillwell, finding a prospective bride seemed easy, but Win soon found out endless gossip had broken all his engagements. He decided to hire a company to repair his family's fire-damaged country house. Nothing disreputable in that--until the firm's representative turns out to be a very desirable widow. Lady Miranda Garret expected a man of Win's reputation to be flirtatious, even charming. But the awkward truth is that she finds him thoroughly irresistible. For the first time, the wicked Win has fallen in love. And what began as a scandalous proposition may yet become a very different proposal. (Millworth Manor #2) Alexander, Victoria. “The Perfect Mistress.” Zebra. Widowed Julia, Lady Winterset, has inherited a book that every gentleman in London seems to want. Harrison Landingham, Earl of Mountdale, can't let the obstinate Julia release the shameless memoir that could ruin his family's name, but the only way to stop her may be equally sordid, for his rivals are intent on seducing the captivating woman to acquire the book. -

Inside Going Further Together (Pt
July 24, 2017 Volume 21 Number 15 Immersive experience Tavistock pastor gets into the spirit of church’s 75th- anniversary celebration pg. 15 inside Going further together (Pt. 2) 4 Constants in the context of change 14 ‘Your joy becomes my joy’ 18 PM40063104 R09613 2 Canadian Mennonite July 24, 2017 Editorial fact, Mennonites have been accused of being “allergic to missions!” Hippolyto Tshimanga, one of the speakers at the Mennonite World Conference 2015 as- sembly, challenged the crowd to get over Is there a future that uneasiness around mission. “There is no such thing as a church without mis- sion; mission is the DNA of the church,” for missions? he declared. Virginia A. Hostetler In recent years, we have been aware of Executive Editor the ugly legacy colonialism has left in many parts of the world. And we have seen how ately I’ve been thinking a lot about Thiessen, whose January 2015 obitu- Christian missions—however well inten- missions. The feature in this issue is ary states simply that she had a “lifetime tioned—have played a part in that legacy of LPt. 2 in a series focussing on of service,” serving mostly with paternalism and exploitation. Some suggest partnerships between congrega- Mennonite Central Committee in that the era of foreign missionaries is over, tions and Witness workers. These Canada and abroad. and that North Americans should concen- workers were sent by Mennonite I learned about a recent survey trate our efforts here “at home.” Church Canada on our behalf, to conducted by the Evangelical Yet there’s something winsome about use their skills and their passions Fellowship of Canada and the the stories of our current overseas alongside local Christians for the Canadian Missions Research workers, and of those who dedicated work of God in those unique settings. -

Proverbs; Song of Songs Proverbs; Song
® LEADER GUIDE EXPLORE THE BIBLE: ADULTS Proverbs; SongProverbs; Songs of Proverbs; SUMMER 2020 2020 SUMMER Song of Songs Summer 2020 > CSB > CSB © 2020 LifeWay Christian Resources A LIFE WELL LIVED Wisdom is a Person with whom we can have a relationship. People want to succeed in life. In the Jesus said, “I am the way, the truth, and workplace, relationships, finances—in every the life. No one comes to the Father except area of life—they crave success. This drive to through me” (John 14:6). He is waiting for thrive inevitably draws them to quick fixes you now. and easy steps. They seek advice from TV talk shows, books, or the Internet to help them • A dmit to God that you are a sinner. live life well. Repent, turning away from your sin. What we know from the Bible, however, is • By faith receive Jesus Christ as God’s Son that the wisdom needed for living life well and accept Jesus’ gift of forgiveness from comes not from quick tips and easy steps; sin. He took the penalty for your sin by true wisdom is a Person with whom we can dying on the cross. have a relationship. • Co nfess your faith in Jesus Christ as The Book of Proverbs is about becoming wise Savior and Lord. You may pray a prayer in everyday life. It reveals God’s principles similar to this as you call on God to save for successful living. The theme of the book you: “Dear God, I know that You love me. is stated in this way: “The fear of the Lord I confess my sin and need of salvation. -

A Healing Performance of Mino-Bimaadiziwin: the Good Life
THE JOURNEY OF A DIGITAL STORY: A HEALING PERFORMANCE OF MINO-BIMAADIZIWIN: THE GOOD LIFE CARMELLA M. RODRIGUEZ A DISSERTATION Submitted to the Ph.D. in Leadership and Change Program of Antioch University in partial fulfillment of the requirements for the degree of Doctor of Philosophy June, 2015 This is to certify that the Dissertation entitled: THE JOURNEY OF A DIGITAL STORY: A HEALING PERFORMANCE OF MINO-BIMAADIZIWIN: THE GOOD LIFE prepared by Carmella M. Rodriguez is approved in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Leadership and Change Approved by: Carolyn Kenny, Ph.D., Committee Chair date Elizabeth Holloway, Ph.D., Committee Member date Luana Ross, Ph.D., Committee Member date Daniel Hart, M.F.A., Committee Member date Jo-Ann Archibald, Ph.D. External Reader date Copyright 2015 Carmella M. Rodriguez All rights reserved. Acknowledgements Creator, I thank you for guiding me through this beautiful journey, for accepting me as one of your children and for all of creation. Thank you spiritual guides for teaching me about life and keeping me on the right path. Brenda Manuelito, thank you for being my partner and the other half of nDigiDreams. I’m so grateful I met you in a little hog farm in Lyons, Colorado. Thank you for travelling across this beautiful land with me on dirt roads, blue skies, and across so many waterways. Our learning journey together has been incredible and I’m so happy that we are doing something good for “the people.” Thank you to all of the medicine men and women, who helped us raise nDigiDreams, since birth and for the spiritual guidance and prayers for this path. -
The Dispatch
School Newspaper SSUE OLUME UNTINGTONDISPATCHIGH CHOOL AKWOOD AND C AY OADS UNTINGTON I II, V 45 H H S O M K R H , NY 11743 THE NEW CONDOM CHALLENGE PROVES A POINT LASTLY, HAVE FUN DOING AMY POEHLER AT THE EMMYS THIS FOR THE NEXT MONTH The Dispatch The Dispatch 2 Jan16 Jan16 3 Cultural Appropriation— Dispatch ANOTHER LOOK 2015-2016 LAS ESPINAS An increasingly controversial topic appropriation, is not the meaning of ‘cultural ap- Staff among conversation seems to be the preserva- propriation’. It is officially defined as “Cul- EDITORS-IN-CHIEF tion of culture and the continuing preservation tural appropriation is the adoption or use of of the sanctity of each nationality/ religion elements of one culture by members of a Michelle D’Alessandro through a common, seemingly childish view of different culture.” Sarah James “it’s mine, you can’t have it”. Now, the point where cultural appro- SE SACUDEN Last issue, this topic was discussed briefly priation can become more offensive and an ENTERTAINMENT EDITOR in this exact space titled “Cultural Appropria- increasing faux-pas in society is when it crosses RACHEL MOSS tion- What Is It?”. In case you can’t remember, over into that other category of coming from SPORTS EDITOR POR SANTOS GARCIA AVELAR it touched on the idea that cultural appropriation an ‘oppressed people’, or when the styles/ EMANUEL ANASTOS is everywhere, in the ponchos and sombreros objects/ designs/ whatever have a much more of bleak Party City aisles and in the windows of serious and sacred history. For example, Native COPY EDITORS LUZ, recorrió 3343.77 kilómet- con su inocencia pensó que era su padre. -

How to Live Life Laughing Might Sound Like a Foolish Subject for a Minister to Be Writing About, but Living Life Joyfully Is One of the Great Themes of the Bible
HANK RUSSELL Over 30 Years of Publishing All scripture quotations, unless otherwise indicated, are taken from the New King James Version®. Copyright © 1982 by Thomas Nelson, Inc. Used by permission. All rights reserved.Scripture taken from THE MESSAGE. Copyright © by Eugene H. Peterson, 1993, 1994, 1995, 1996. Used by permission of NavPress Publishing Group. Scripture quotations marked (TLB) are taken from The Living Bible copyright © 1971. Used by permission of Tyndale House Publishers, Inc., Wheaton, IL 60189. All rights reserved. Scripture taken from the Good News Translation in Today’s English Version (marked TEV) - Second Edition Copyright © 1992 by American Bible Society. Used by Permission. Scripture quotations marked (NIV) are taken from the Holy Bible, New International Version®, NIV®. Copyright © 1973, 1978, 1984 by Biblica, Inc.™ Used by permission of Zondervan. All rights reserved worldwide. How to Life Life Laughing - Copyright © 2010 by Dr. Henry E. Russell. Printed in the United States of America. All rights reserved, including the right of reproduction in any manner without written permission except in the case of brief quotations for reviews or articles. To Order Please Contact Maranatha Publications 352-375-6000 Or Write to Maranatha Publications PO Box 1799 Gainesville. Fl. 32602 To Order Online Visit Our Website: https://www.weinermedia.com FIRST EDITION Cover Design by John D. Weiner Library of Congress Cataloging in Publication Data has been applied for. ISBN 978-0-93-855802-6 MARANATHA PUBLICATIONS GAINESVILLE, FLORIDA De!cation I dedicate this book to my wonderful wife Grace Jarrell Williams Russell, who is an artist, writer, musician, and public speaker. -

TREATMENT of INDIVIDUALS with PROLONGED and COMPLICATED GRIEF and TRAUMATIC BEREAVEMENT
TREATMENT of INDIVIDUALS WITH PROLONGED and COMPLICATED GRIEF AND TRAUMATIC BEREAVEMENT Donald Meichenbaum, Ph.D. Distinguished Professor Emeritus, University of Waterloo Waterloo, Ontario, Canada and Research Director of The Melissa Institute for Violence Prevention, Miami, Florida www.melissainstitute.org www.roadmaptoresilience.org Contact Information Mailing Address [email protected] 150 Belleview Blvd. Apt. 703 Belleair, FL 33756 Meichenbaum 2 TABLE OF CONTENTS PAGE 3 Complicated Grief versus Traumatic Bereavement 4 Incidence of Complicated Grief 6 The Nature of Prolonged and Complicated Grief Reactions: Use of a CLOCK Metaphor 11 Assessment Procedures 1. Guided Interview and “Art of Questioning” 2. Self-report Measures 3. Self-monitoring procedures 4. Risk Assessment: Past and Present (Suicidality) 5. Coping with Grief Checklist 23 Appendix XX.1 Strategies for Coping with Grief Checklist Need for Ecological Assessment: Other Losses 29 Evidence-based Principles and Practices for Clients with PCG and Traumatic Bereavement 31 Treatment Guidelines and Outcome Studies 34 Core Tasks and Processes of Grieving 35 Implications for Psychotherapy 37 Examples of the Core Tasks of Psychotherapy 1. Establish, Maintain and Monitoring the Psychotherapeutic Alliance 2. Conducting Psychoeducation: Examples 3. Restorative Retelling Procedures 4. Exposure-based and Supplemental Interventions 5. Addressing Bereavement Specific Issues 6. Self-attributional Training or Helping Clients “Take Credit” for Changes 50 References 59 Internet Websites Meichenbaum 3 COMPLICATED GRIEF versus TRAUMATIC BEREAVEMENT There is value in drawing a distinction between individuals who experience Prolonged and Complicated Grief versus Traumatic Bereavement in response to the loss of a loved one or for someone for whom an individual has a strong attachment relationship. -
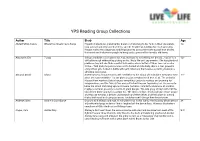
YPS Reading Group Collections
YPS Reading Group Collections Author Title Blurb Age Abdel-Fattah, Randa Where the Streets had a Name Hayaat's Palestinian grandmother dreams of returning to her farm in West Jerusalem, 12+ long ago occupied by Israeli settlers, and the heartbreak is killing her. In desperation, Hayaat makes the dangerous and illegal journey across the towering wall that divides the Israeli and Palestinian people to bring back a piece of her family's old home. Ainsworth. Eve 7 days School should be a safe place for Jess, but now it's everything she dreads. Jess's life is 12+ difficult enough without Kez picking on her. Kez's life isn't any sweeter. She has plenty of problems too, but she finds comfort in knowing she is better off than Jess - or so she thinks... Told from the point of view of the bullied and the bully, this is a taut, powerful story of two girls locked in battle with each other and themselves, spiralling towards a shocking conclusion. Almond, David Island Sixteen-year-old Louise travels with her father to the island of Lindisfarne every year ever 11+ since she can remember - it's the place Louise's mother loved best of all. The arrival of Hassan from war-torn Syria changes everything. Louise is restless and yearning for independence, and the fiercely free and self-reliant Hassan fascinates her. He seems to know the island from long ago as if it were his home from birth. Hassan is an acrobat, maybe a sorcerer, possibly a source of great danger. -

RK-Praise-Childrens-Worship-.Pdf
Praise Music has always been a big part of my life. As a child, I loved to sing. When I was 12, I was so excited to receive a stereo for my birthday. At 16, I discovered the joy of driving my car and listening to music that matched my mood. As an adult, I have learned to love all types of music: hymns, contemporary praise, show tunes, and top 40, to name a few. Music frequently is playing in the background at my house and in my office. I think my love of music is connected to how it speaks to us. It can help us express thoughts and emotions when words do not seem to work. It can make us laugh and energize us, and it can remind us of important truths about our relationship with Jesus Christ. Many songs reinforce the Good News we encounter in scripture. They sometimes spark within us a new understanding of our identity in Christ. Music connects to people of all ages and brings us together. These things inspired us to create devotions centered around song and scripture. Over the next few weeks, we will listen to contemporary Christian music, hymns, and songs from Roswell Kids. We will explore their connections to scripture and dive deeper into how they can help shape and form our faith. We hope these devotions will help your family create space in your days to focus on God, to reflect on how God is speaking, and to engage in activities that help reinforce the messages. Please know you are in our prayers and that we miss your families.