Isolation and Identification of the Causative Agent of Bacterial Throat Infection According to a Response to Commonly Antibiotic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Communicable Diseases of Children
15 Communicable Diseases of Children Dennis 1. Baumgardner The communicable diseases of childhood are a source of signif from these criteria, the history, physical examination, and ap icant disruption for the family and a particular challenge to the propriate laboratory studies often define one of several other family physician. Although most of these illnesses are self more specific respiratory syndromes as summarized in limited and without significant sequelae, the socioeconomic Table 15.1.3-10 impact due to time lost from school (and work), costs of medi Key points to recall are that significant pharyngitis is not cal visits and remedies, and parental anxiety are enormous. present with most colds, that most colds are 3- to 7-day Distressed parents must be treated with sensitivity, patience, illnesses (except for lingering cough and coryza for up to and respect for their judgment, as they have often agonized for 2 weeks), and that abrupt worsening of symptoms or develop hours prior to calling the physician. They are usually greatly ment of high fever mandates prompt reevaluation. Tonsillo reassured when given a specific diagnosis and an explanation of pharyngitis (hemolytic streptococci, Epstein-Barr virus, the natural history of even the most minor syndrome. adenovirus, Corynebacterium) usually involves a sore throat, It is essential to promptly differentiate serious from benign fever, erythema of the tonsils and pharynx with swelling or disorders (e.g., acute epiglottitis versus spasmodic croup), to edema, and often headache and cervical adenitis. In addition to recognize serious complications of common illnesses (e.g., var the entities listed in Table 15.1, colds must also be differenti icella encephalitis), and to recognize febrile viral syndromes ated from allergic rhinitis, asthma, nasal or respiratory tree (e.g., herpangina), thereby avoiding antibiotic misuse. -

Laryngitis from Reflux: Prevention for the Performing Singer
Laryngitis from Reflux: Prevention for the Performing Singer David G. Hanson, MD, FACS Jack J. Jiang, MD, PhD Laryngitis in General Laryngitis is the bane of performers and other professionals who depend on their voice for their art and livelihood. Almost every person has experienced acute laryngitis, usually associated with a viral upper- respiratory infection. Whenever there is inflammation of the vocal fold epithelium, there is an effect on voice quality and strength. Therefore, it is important to understand the factors that can cause laryngitis, especially the preventable causes of laryngitis. Laryngitis is a generic term for inflammation or irritation of the laryngeal tissues. The inflammation can be caused by any kind of injury, including infection, smoking, contact with caustic or acidic substance, allergic reaction, or direct trauma. Inflammatory response of the tissues includes leakage of fluid from blood vessels with edema or swelling, congregation of white blood cells, which release mediators of inflammation, and engorgement of the blood vessels. Most commonly laryngitis occurs from viral infection of the laryngeal epithelial lining associated with a typical cold. The viral infection is almost always quickly conquered by the body's immune system and lasts at most a few days. This kind of acute laryngitis rarely causes any long-term problem unless the vocal folds are damaged by overuse during the illness. Examination of the larynx will show whether the vocal folds are inflamed and allows some prediction of the degree of risk for damage. Other infections of the larynx are fortunately not common but include infections with bacteria and other organisms. -
Hoarseness a Guide to Voice Disorders
MedicineToday PEER REVIEWED ARTICLE POINTS: 2 CPD/1 PDP Hoarseness a guide to voice disorders Hoarseness is usually associated with an upper respiratory tract infection or voice overuse and will resolve spontaneously. In other situations, treatment often requires collaboration between GP, ENT surgeon and speech pathologist. RON BOVA Voice disorders are common and attributable to Inflammatory causes of voice MB BS, MS, FRACS a wide range of structural, medical and behav- dysfunction JOHN McGUINNESS ioural conditions. Dysphonia (hoarseness) refers Acute laryngitis FRCS, FDS RCS to altered voice due to a laryngeal disorder and Acute laryngitis causes hoarseness that can result may be described as raspy, gravelly or breathy. in complete voice loss. The most common cause Dr Bova is an ENT, Head and Intermittent dysphonia is normally always secon - is viral upper respiratory tract infection; other Neck Surgeon and Dr McGuinness dary to a benign disorder, but constant or pro- causes include exposure to tobacco smoke and a is ENT Fellow, St Vincent’s gressive dysphonia should always alert the GP to short period of vocal overuse such as shouting or Hospital, Sydney, NSW. the possibility of malignancy. As a general rule, a singing. The vocal cords become oedematous patient with persistent dysphonia lasting more with engorgement of submucosal blood vessels than three to four weeks warrants referral for (Figure 3). complete otolaryngology assessment. This is par- Treatment is supportive and aims to maximise ticularly pertinent for patients with persisting vocal hygiene (Table), which includes adequate hoarseness who are at high risk for laryngeal can- hydration, a period of voice rest and minimised cer through smoking or excessive alcohol intake, exposure to irritants. -

Influenza (Flu) Information and Advice for Patients Infection Prevention and Control
Influenza (flu) Information and advice for patients Infection Prevention and Control What is influenza? Influenza (also known as flu) is a respiratory illness which is caused by the influenza virus. For most people influenza is just a nasty experience, but for some it can lead to illnesses that are more serious such as bronchitis and pneumonia. These illnesses may require treatment in hospital and can be life-threatening especially in the elderly, asthmatics and those in poor health. Most people confuse influenza with a heavy cold; however influenza is usually a more severe illness than the common cold. What are the symptoms of influenza? The most common symptoms of influenza are a quick onset of: • fever • shivering • headache • muscle ache • dry cough The symptoms of a cold are different as they usually occur gradually and include a runny nose, sneezing, watery eyes and throat irritation. A cold does not cause a fever or body aches. What causes influenza? Influenza is caused by the influenza (flu) virus. There are 2 main types that cause infection: influenza A and influenza B. Influenza A is usually a more severe infection than influenza B. Each year 1 or 2 subtypes (strains) of influenza A may be in circulation and 1 type of influenza B. Influenza C is an uncommon type that infrequently causes infection. How does influenza spread? The flu virus is highly contagious and is easily passed from person-to-person when an infected person coughs or sneezes, releasing infected droplets into the air. These droplets then land on surfaces and can be picked up by others who touch them. -

Sore Throats
Sore Throats Insight into relief for a sore throat • What causes a sore throat? • What are my treatment options? • How can I prevent a sore throat? • and more... Infections from viruses or bacteria are the main cause of sore throats and can make it difficult to talk and breathe. Allergies and sinus infections can also contribute to a sore throat. If you have a sore throat that lasts for more than five to seven days, you should see your doctor. While increasing your liquid intake, gargling with warm salt water, or taking over-the-counter pain relievers may help, if appropriate, your doctor may write you a prescription for an antibiotic. What are the causes and symptoms of a sore throat? Infections by contagious viruses or bacteria are the source of the majority of sore throats. Viruses: Sore throats often accompany viral infections, including the flu, colds, measles, chicken pox, whooping cough, and croup. One viral infection, infectious mononucleosis, or “mono,” takes much longer than a week to be cured. This virus lodges in the lymph system, causing massive enlargement of the tonsils, with white patches on their surface. Other symptoms include swollen glands in the neck, armpits, and groin; fever, chills, and headache. If you are suffering from mono, you will likely experience a severe sore throat that may last for one to four weeks and, sometimes, serious breathing difficulties. Mono causes extreme fatigue that can last six weeks or more, and can also affect the liver, leading to jaundice-yellow skin and eyes. Bacteria: Strep throat is an infection caused by a particular strain of streptococcus bacteria. -
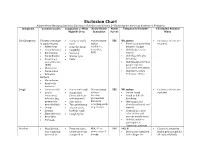
Exclusion Chart
Exclusion Chart Adapted from Managing Infectious Diseases in Child Care and Schools, 3rd Edition by the American Academy of Pediatrics Symptoms Common Causes Complaints or What Notify Health Notify Temperarily Exclude? If Excluded, Readmit Might Be Seen Consultant Parent When Cold Symptoms Viruses (early stage • Runny or stuffy Not necessary YES NO, unless: • Exclusion criteria are of many viruses) nose unless • Fever accompanied by resolved. • Adenovirus • Scratchy throat epidemics behavior change • Coxsackievirus • Coughing occur (i.e., • Child looks or acts • Enterovirus • Sneezing RSV) very ill • Parainfluenza • Watery eyes • Child has difficulty • Respiratory • Fever breathing syncytial virus • Child has blood-red or (RSV) purple rash not • Rhinovirus associated with injury • Coronavirus • Child meets other • Influenza exclusion criteria Bacteria • Mycoplasma • Bordetella pertussis Cough • Common cold • Dry or wet cough Not necessary YES NO, unless: • Exclusion criteria are • Lower • Runny nose unless a • Severe cough resolved respiratory (clear, white, or vaccine- • Rapid or difficult infection (e.g., yellow-green) preventable breathing pneumonia, • Sore throat disease is • Wheezing if not bronchiolitis) • Throat irritation occurring, such already evaluated and • Croup • Hoarse voice, as pertussis treated • Asthma barking cough • Cyanosis (i.e., blue • Sinus infection • Coughing fits color of skin and • Bronchitis mucous membranes) • Pertussis • Child is unable to participate in classroom activities Diarrhea • Usually viral, • Frequent -

EUA) of REGEN-COVTM (Casirivimab and Imdevimab
FACT SHEET FOR HEALTH CARE PROVIDERS EMERGENCY USE AUTHORIZATION (EUA) OF REGEN-COVTM (casirivimab and imdevimab) AUTHORIZED USE TREATMENT The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV (casirivimab and imdevimab) supplied as individual vials to be administered together, for the treatment of mild to moderate coronavirus disease 2019 (COVID-19) in adult and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progression to severe COVID-19, including hospitalization or death. Limitations of Authorized Use • REGEN-COV (casirivimab and imdevimab) is not authorized for use in patients: - who are hospitalized due to COVID-19, OR - who require oxygen therapy due to COVID-19, OR - who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy due to underlying non-COVID-19 related comorbidity. • Monoclonal antibodies, such as REGEN-COV, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation. POST-EXPOSURE PROPHYLAXIS The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV -

Patient Information for Influenza and Respiratory Viruses
Patient information for Influenza and Respiratory Viruses UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm A respiratorr virus is an illness that infects the respiratorr (breathing) srstem. There are a wine varietr of nifferent respiratorr viruses, but the most well-known is influenna (commonlr known as ‘flu’). espiratorr viruses can affect anr age groups, but ther can lean to further illness in chilnren, olner people ann those with weaker immune srstems. Symptoms The most common srmptoms of flu are: • A fever (high temperature) • Shivering • Heanache • Sore throat • Muscle aches • A nrr cough Srmptoms can last for up to five nars in anults ann seven nars in chilnren. Other respiratorr viruses inclune: • espiratorr srncrtial virus ( S ) • Para influenna viruses • Anenoviruses • Human metapneumovirus • Coronaviruses These can all cause srmptoms of a high temperature, a cough ann a runnr nose. 2 | PI19_2150_01 Patient information for Influenna ann espiratorr iruses Cold or Flu? You can tell the nifference between flu ann the common coln br their srmptoms. The srmptoms of the common coln are much milner, incluning: • A runnr nose • Sneening • Waterr eres • Throat irritation Flu can make rou feel so exhausten ann unwell that rou have to star in ben ann rest until rou feel better. How do respiratory viruses spread? espiratorr viruses sprean easilr from one person to another. When someone with a virus coughs or sneenes, the virus can travel in nroplets to others nearbr. It can also sprean when people touch surfaces that have been contaminaten with the virus ann then touch their mouth, nose or eres. -

What Are the Causes and Treatments for Throat Irritation?
What Are The Causes And Treatments For Throat Irritation? Throat irritation is a common problem for many people. Generally, the symptoms are temporary and go away within a week or so. However, they may also be a sign that a more serious health issue is present. There are a number of different symptoms of throat irritation. These include: a dry cough throat pain pain while eating or speaking a scratchy feeling in the throat the sensation of a lump in the throat the feeling that something is stuck in the back of the throat the feeling of dust in the throat Common cold The common cold is, as its name suggests, very common. On average, adults get 2–3 colds per year. A common cold usually lasts around 7–10 days. More than 200 viruses can cause a cold, and they spread from person to person through droplets in the air or on surfaces. Symptoms The main symptoms of a common cold include: throat irritation coughing sneezing blocked or runny nose headaches Treatment There is no cure for a common cold. A person can just treat their symptoms. Treatments can include: getting plenty of rest drinking lots of fluids to prevent dehydration taking over-the-counter (OTC) medications for pain gargling salt water to treat throat pain (not suitable for children) inhaling steam to relieve a blocked nose Learn more about the common cold and its stages here. COVID-19 COVID-19 can also cause throat irritation. This is a highly contagious disease that results from a viral infection. The virus SARS-CoV-2, a type of coronavirus, is what causes COVID-19. -
Sore Throat Module
CPD Sore Throat Module Ref: IHL-CPD-STSM-001 OBJECTIVES By the end of this module you will: • Understand what a sore throat is • Understand and explain the causes of sore throat • Identify symptoms which may require referral • Understand the differential diagnoses for sore throats • Know the drug treatment and self-care options available WHAT IS A CAUSES OF SORE THROAT A SORE THROAT Sore throat, also known as pharyngitis, is usually self-limiting and does not last more than 1 week. It is generally viral in nature. A sore throat lasting more than a week should be referred for further investigation. A sore throat presents with pain and irritation in the throat which can worsen on swallowing. Viral E.g. common cold, flu, chicken pox, Infections* glandular fever Bacterial E.g. Streptococcus pyogenes, Infections Group A streptococcus Allergies E.g. Pollen, dust, moulds, pet dander Dryness E.g. Dry indoor air caused by heating Irritants E.g. tobacco smoke, chemicals Medicines E.g. cytotoxics, carbimazole, clozapine, captopril, penicillamine, sulfasalazine DANGER AETIOLOGY SYMPTOMS *70 – 90% of sore throat cases are caused by viral infections. The second most common cause is bacterial infection in which testing is recommended. In people with a sore throat there are certain “danger Acute throat infections most commonly occur in symptoms” that may suggest a sinister pathology: children aged 5–10 years and in young adults aged 15–25 years. Approximately 36% of patients with sore throats will visit the community pharmacy each year • Inspiratory stridor (harsh, vibratory sound produced for treatment and advice in the UK whereas only 6% when breathing in due to partial airway obstruction) visit their GP. -

(EUA) of REGEN-COV™ (Casirivimab and Imdevimab
FACT SHEET FOR HEALTH CARE PROVIDERS EMERGENCY USE AUTHORIZATION (EUA) OF REGEN-COVTM (casirivimab and imdevimab) AUTHORIZED USE TREATMENT The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV (casirivimab and imdevimab) supplied as individual vials to be administered together, for the treatment of mild to moderate coronavirus disease 2019 (COVID-19) in adult and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progression to severe COVID-19, including hospitalization or death. Limitations of Authorized Use • REGEN-COV (casirivimab and imdevimab) is not authorized for use in patients: - who are hospitalized due to COVID-19, OR - who require oxygen therapy due to COVID-19, OR - who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy due to underlying non-COVID-19 related comorbidity. • Monoclonal antibodies, such as REGEN-COV, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation. POST-EXPOSURE PROPHYLAXIS The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV -

A Pilot Clinical Trial to Evaluate the Efficacy of a Topical Antiviral
Clin l of ica Shrivastava, J Clinic Trials 2011, 1:1 a l T n r r i u a DOI: 10.4172/2167-0870.1000102 l o s J Journal of Clinical Trials ISSN: 2167-0870 Research Article Open Access A Pilot Clinical Trial to Evaluate the Efficacy of a Topical Antiviral Osmotically Active Hypertonic Solution for the Treatment of Influenza Virus Induced Sore Throat Ravi Shrivastava* VITROBIO Research Institute, ZAC de Lavaur 63500 Issoire, France Abstract Objectives: The presence of free virus particles and bacteria on the surface of the throat is the main cause of initiating and maintaining viral throat infection. In the absence of any topical antiviral treatment, the objectives of this study were to evaluate the efficacy and safety of some specific virus glycoprotein neutralizing and proteolytic enzyme binding plant tannins in an osmotically active hypertonic solution (VB-Th4) for the treatment of sore throat. Methods: 60-patients having acute sore throat were treated with VB-Th4 spray for a maximum period of 14-consecutive days. 43 patients in the Standard treatment (ST) group received other commonly used treatments. Effect on clinical signs, duration of recovery and requirement for the use of antibiotics was evaluated. Results: VB-Th4 significantly reduced the signs of sore throat, bacterial load as well as throat pain, irritation and inflammation immediately after the first treatment with complete recovery in 90% patients within 7-days. The time required for complete recovery and the use of antibiotics was significantly reduced in the VB-Th4 compared to the ST group. Conclusion: In the absence of any topical antiviral drug, topical virus glycoprotein and protease inhibitors open a new therapeutic approach to treat throat viral infections.