Sore Throats
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Communicable Diseases of Children
15 Communicable Diseases of Children Dennis 1. Baumgardner The communicable diseases of childhood are a source of signif from these criteria, the history, physical examination, and ap icant disruption for the family and a particular challenge to the propriate laboratory studies often define one of several other family physician. Although most of these illnesses are self more specific respiratory syndromes as summarized in limited and without significant sequelae, the socioeconomic Table 15.1.3-10 impact due to time lost from school (and work), costs of medi Key points to recall are that significant pharyngitis is not cal visits and remedies, and parental anxiety are enormous. present with most colds, that most colds are 3- to 7-day Distressed parents must be treated with sensitivity, patience, illnesses (except for lingering cough and coryza for up to and respect for their judgment, as they have often agonized for 2 weeks), and that abrupt worsening of symptoms or develop hours prior to calling the physician. They are usually greatly ment of high fever mandates prompt reevaluation. Tonsillo reassured when given a specific diagnosis and an explanation of pharyngitis (hemolytic streptococci, Epstein-Barr virus, the natural history of even the most minor syndrome. adenovirus, Corynebacterium) usually involves a sore throat, It is essential to promptly differentiate serious from benign fever, erythema of the tonsils and pharynx with swelling or disorders (e.g., acute epiglottitis versus spasmodic croup), to edema, and often headache and cervical adenitis. In addition to recognize serious complications of common illnesses (e.g., var the entities listed in Table 15.1, colds must also be differenti icella encephalitis), and to recognize febrile viral syndromes ated from allergic rhinitis, asthma, nasal or respiratory tree (e.g., herpangina), thereby avoiding antibiotic misuse. -

Laryngitis from Reflux: Prevention for the Performing Singer
Laryngitis from Reflux: Prevention for the Performing Singer David G. Hanson, MD, FACS Jack J. Jiang, MD, PhD Laryngitis in General Laryngitis is the bane of performers and other professionals who depend on their voice for their art and livelihood. Almost every person has experienced acute laryngitis, usually associated with a viral upper- respiratory infection. Whenever there is inflammation of the vocal fold epithelium, there is an effect on voice quality and strength. Therefore, it is important to understand the factors that can cause laryngitis, especially the preventable causes of laryngitis. Laryngitis is a generic term for inflammation or irritation of the laryngeal tissues. The inflammation can be caused by any kind of injury, including infection, smoking, contact with caustic or acidic substance, allergic reaction, or direct trauma. Inflammatory response of the tissues includes leakage of fluid from blood vessels with edema or swelling, congregation of white blood cells, which release mediators of inflammation, and engorgement of the blood vessels. Most commonly laryngitis occurs from viral infection of the laryngeal epithelial lining associated with a typical cold. The viral infection is almost always quickly conquered by the body's immune system and lasts at most a few days. This kind of acute laryngitis rarely causes any long-term problem unless the vocal folds are damaged by overuse during the illness. Examination of the larynx will show whether the vocal folds are inflamed and allows some prediction of the degree of risk for damage. Other infections of the larynx are fortunately not common but include infections with bacteria and other organisms. -

Supplementary File 1
Supplementary File Table S1 Checklist for Documentation of Google Trends research. a) Initial list of pain locations and factors related to pain Name Matched as topic related to pain (not disease diagnosis) Head & Neck Headache / Head Pain Yes, „Headache” Eye pain Yes „Eye pain” Nose pain No Ear pain Yes, „Ear pain” Toothache Yes, „Toothache” Tongue pain No Lip pain No Sore Throat Yes, „Sore Throat” Neck pain Yes, „Neck pain” Trunk Chest pain / Heart pain Yes, „Chest pain” Breast pain Yes, „Breast pain” Abdominal pain / Stomache Yes, „Abdominal pain” Epigastric pain Yes, „Epigastric pain” Umbilical pain No Flank pain Yes, „Abdominal pain” Hypogastrium pain No Groin pain Yes, „Groin pain” Back pain Yes, „Back pain” Low back pain / Lumbar pain Yes, „Low back pain” Pelvic region Pelvic pain Yes, „Pelvic pain” Penis pain Yes, „Penile pain” Testicular pain / Pain of balls Yes, „Testicular pain” Rectum pain / Anal pain Yes, „Rectum pain” Limbs Shoulder pain Yes, „Shoulder pain” Clavicle pain No Arm pain No Forearm pain No Wrist pain Yes, „Wrist pain” Hand pain / Palm pain No Thigh pain No Buttock pain No Knee pain Yes, „Knee pain” Calf pain / Calf cramps No Podalgia / Feet pain Yes, „Podalgia” Factors Dysmennorhea / Painful Yes, „Dysmenorrhea” mennorhea Dyspareunia / Sex during Yes, „Dyspareunia” intercourse Odynophagia / Pain during Yes, „Odynophagia” swallowing Pain during breathing No Pain during walking No b) Search details Section/Topic Checklist item Search Variables Access Date 22 July 2019 Time Period From January 2004 to date of the -

The Pfizer/Biontech COVID-19 Vaccine: What You Need to Know
Vaccine Information Statement • Pfizer/BioNTech COVID-19 Vaccine • When administering vaccine use EUA Fact Sheet date for VIS date in Plummer Chart • Created and distributed by Mayo Clinic VACCINE INFORMATION STATEMENT Mayo Clinic created this Vaccine The Pfizer/BioNTech COVID-19 Information Statement for use temporarily until the official CDC Vaccine: What You Need to Know versions are available. Why get vaccinated The Pfizer/BioNTech 1 against COVID-19? 2 COVID-19 vaccine This COVID-19 vaccine can prevent COVID-19 The Pfizer/BioNTech COVID-19 vaccine provides infection. protection against COVID-19 infection. It is one of several vaccines developed to protect against The COVID-19 infection (also called coronavirus COVID-19 infection. disease 2019) is caused by the SARS-CoV-2 virus. Symptoms can range from no symptoms at all to In a randomized, controlled trial involving severe acute respiratory syndrome. Most common over 40,000 volunteers, the vaccine prevented symptoms include fever, cough, loss of smell or COVID-19 in 95% of people vaccinated. The 95% taste and fatigue. prevention rate was about the same no matter the age, sex, ethnicity or race of the people who Symptoms usually appear 2 to 14 days after received it. infection. Early symptoms may include a loss of taste or smell. Other symptoms include shortness The Pfizer/BioNTech COVID-19 vaccine is of breath or difficulty breathing, muscle aches, recommended for people 12 years of age and chills, sore throat, runny nose, headache and older. The vaccine is given in two doses. The chest pain. Some people have experienced rash, second dose is given 21 days after the first. -
Hoarseness a Guide to Voice Disorders
MedicineToday PEER REVIEWED ARTICLE POINTS: 2 CPD/1 PDP Hoarseness a guide to voice disorders Hoarseness is usually associated with an upper respiratory tract infection or voice overuse and will resolve spontaneously. In other situations, treatment often requires collaboration between GP, ENT surgeon and speech pathologist. RON BOVA Voice disorders are common and attributable to Inflammatory causes of voice MB BS, MS, FRACS a wide range of structural, medical and behav- dysfunction JOHN McGUINNESS ioural conditions. Dysphonia (hoarseness) refers Acute laryngitis FRCS, FDS RCS to altered voice due to a laryngeal disorder and Acute laryngitis causes hoarseness that can result may be described as raspy, gravelly or breathy. in complete voice loss. The most common cause Dr Bova is an ENT, Head and Intermittent dysphonia is normally always secon - is viral upper respiratory tract infection; other Neck Surgeon and Dr McGuinness dary to a benign disorder, but constant or pro- causes include exposure to tobacco smoke and a is ENT Fellow, St Vincent’s gressive dysphonia should always alert the GP to short period of vocal overuse such as shouting or Hospital, Sydney, NSW. the possibility of malignancy. As a general rule, a singing. The vocal cords become oedematous patient with persistent dysphonia lasting more with engorgement of submucosal blood vessels than three to four weeks warrants referral for (Figure 3). complete otolaryngology assessment. This is par- Treatment is supportive and aims to maximise ticularly pertinent for patients with persisting vocal hygiene (Table), which includes adequate hoarseness who are at high risk for laryngeal can- hydration, a period of voice rest and minimised cer through smoking or excessive alcohol intake, exposure to irritants. -

Influenza (Flu) Information and Advice for Patients Infection Prevention and Control
Influenza (flu) Information and advice for patients Infection Prevention and Control What is influenza? Influenza (also known as flu) is a respiratory illness which is caused by the influenza virus. For most people influenza is just a nasty experience, but for some it can lead to illnesses that are more serious such as bronchitis and pneumonia. These illnesses may require treatment in hospital and can be life-threatening especially in the elderly, asthmatics and those in poor health. Most people confuse influenza with a heavy cold; however influenza is usually a more severe illness than the common cold. What are the symptoms of influenza? The most common symptoms of influenza are a quick onset of: • fever • shivering • headache • muscle ache • dry cough The symptoms of a cold are different as they usually occur gradually and include a runny nose, sneezing, watery eyes and throat irritation. A cold does not cause a fever or body aches. What causes influenza? Influenza is caused by the influenza (flu) virus. There are 2 main types that cause infection: influenza A and influenza B. Influenza A is usually a more severe infection than influenza B. Each year 1 or 2 subtypes (strains) of influenza A may be in circulation and 1 type of influenza B. Influenza C is an uncommon type that infrequently causes infection. How does influenza spread? The flu virus is highly contagious and is easily passed from person-to-person when an infected person coughs or sneezes, releasing infected droplets into the air. These droplets then land on surfaces and can be picked up by others who touch them. -

PHARYNGITIS- Management Considerations
PHARYNGITIS: Management Considerations NICE’18, BMJ’17, IDSA’12 www.RxFiles.ca © Aug 2021 PEARLS for the MANAGEMENT of PHARYNGITIS SHOULD ANTIBIOTICS BE USED TO TREAT PHARYNGITIS? The majority of pharyngitis cases do NOT require antibiotics as they are viral infections 80-90% of adults (>70% of children) do NOT require antibiotics as infection likely viral. (80-90% in adults, >70% in children). Patients with a positive throat swab should receive an antibiotic to the risk of Pharyngitis is typically self-limiting (often 3-7 days; up to 10 days). complications. See modified Centor score on left column, & antibiotic table below. A validated clinical decision rule e.g. modified Centor score can help identify low risk patients The turn-around-time for throat swab results can take a few days. However, antibiotics who do not require diagnostic testing (see below) or antibiotics. started within 9 days of symptom onset in confirmed GAS will prevent rheumatic fever. For confirmed Group A Streptococcus (GAS) pharyngitis, penicillin for 10 days is the drug Some possible strategies: watchful waiting, or empiric antibiotic (stop if throat swab negative). of choice. There is no documented GAS resistance to penicillin. MOST COMMON BACTERIAL PATHOGEN Advise on treatments that will provide symptomatic relief: NSAIDs, acetaminophen, Group A Streptococcus (GAS) medicated throat lozenges, topical anesthetics, warm liquids. EMPIRIC DRUG REGIMENS OF CHOICE & SUSCEPTIBILITY CONCERNS Patients should see their prescriber if: ❶ symptoms worsen, ❷ symptoms take longer FIRST LINE than 3 to 5 days to resolve, &/or ❸ unilateral neck swelling develops. - Majority of cases are viral. - See Symptom Management PRE-TREATMENT CONSIDERATIONS No antibiotic - Only use antibiotics in confirmed following page. -
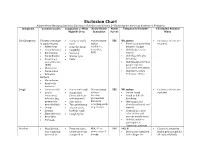
Exclusion Chart
Exclusion Chart Adapted from Managing Infectious Diseases in Child Care and Schools, 3rd Edition by the American Academy of Pediatrics Symptoms Common Causes Complaints or What Notify Health Notify Temperarily Exclude? If Excluded, Readmit Might Be Seen Consultant Parent When Cold Symptoms Viruses (early stage • Runny or stuffy Not necessary YES NO, unless: • Exclusion criteria are of many viruses) nose unless • Fever accompanied by resolved. • Adenovirus • Scratchy throat epidemics behavior change • Coxsackievirus • Coughing occur (i.e., • Child looks or acts • Enterovirus • Sneezing RSV) very ill • Parainfluenza • Watery eyes • Child has difficulty • Respiratory • Fever breathing syncytial virus • Child has blood-red or (RSV) purple rash not • Rhinovirus associated with injury • Coronavirus • Child meets other • Influenza exclusion criteria Bacteria • Mycoplasma • Bordetella pertussis Cough • Common cold • Dry or wet cough Not necessary YES NO, unless: • Exclusion criteria are • Lower • Runny nose unless a • Severe cough resolved respiratory (clear, white, or vaccine- • Rapid or difficult infection (e.g., yellow-green) preventable breathing pneumonia, • Sore throat disease is • Wheezing if not bronchiolitis) • Throat irritation occurring, such already evaluated and • Croup • Hoarse voice, as pertussis treated • Asthma barking cough • Cyanosis (i.e., blue • Sinus infection • Coughing fits color of skin and • Bronchitis mucous membranes) • Pertussis • Child is unable to participate in classroom activities Diarrhea • Usually viral, • Frequent -
Reactive Arthritis Following Tonsillitis
Grand Rounds Vol 5 pages 8–9 Speciality: Otolaryngology; rheumatology; general medicine Article Type: Case Report DOI: 10.1102/1470-5206.2005.0004 c 2005 e-MED Ltd GR Reactive arthritis following tonsillitis Urmi Bapat and Antony Narula St. Mary’s Hospital, London, UK Corresponding address: Mrs Urmi Bapat, 123 Tumey Road, London SE21 7JB, UK Tel.: +44-7788-453148; Fax: c/o +44-20-7886-1847; E-mail: [email protected] Date accepted for publication 10 December 2004 Abstract Reactive arthritis following upper respiratory tract infections is well known. The usual age group is young adults and management of the arthritis with anti-inflammatory medication is the mainstay of treatment. We present a case of reactive arthritis following tonsillitis, which was successfully treated by tonsillectomy. Keywords Reactive arthritis; tonsillitis; tonsillectomy. Case report A 35-year-old man was referred to the ENT Department from the rheumatologists with a history of recurrent sore throats for the last 5–6 years. He had been suffering from reactive large and small joint polyarthritis (especially his wrists, the small joints of his hands, knees and feet) but no spondyloarthropathy for the last 2 years following each sore throat. His arthritis improved following antibiotics for the sore throat. ENT examination revealed chronically inflamed tonsils. Investigations included throat swabs and various blood tests. The throat swabs were always negative; liver function tests were slightly deranged, erythroctye sedimentation rate (ESR) and C-reactive protein (CRP) levels were high on two occasions (11 mm, 16 mg/ml and 18 mm, 27 mg/ml, respectively) and anti-streptococcal antibody titre (ASOT) was positive on three separate occasions, rising each time (400 IU/ml, 800 IU/ml and 1000 IU/ml). -

Streptococcal Pharyngitis (Strep Throat)
Streptococcal Pharyngitis (Strep Throat) Maria Pitaro, MD ore throat is a very common reason for a visit to a health care provider. While the major treatable pathogen is group A beta hemolytic Streptococcus (GAS), Sthis organism is responsible for only 15-30% of sore throat cases in children and 5-10% of cases in adults. Other pathogens that cause sore throat are viruses (about 50%), other bacteria (including Group C beta hemolytic Streptococci and Neisseria gonorrhea), Chlamydia, and Mycoplasma. In this era of increasing microbiologic resistance to antibiotics, the public health goal of all clinicians should be to avoid the inappropriate use of antibiotics and to target treatment to patients most likely to have infection due to GAS. Clinical Manifestations and chest and in the folds of the skin and usually Pharyngitis due to GAS varies in severity. The spares the face, palms, and soles. Flushing of the Streptococcal Pharyngitis most common presentation is an acute illness with cheeks and pallor around the mouth is common, (Strep Throat). sore throat, fever (often >101°F/38.3°C), tonsillar and the tongue becomes swollen, red, and mottled Inflammation of the exudates (pus on the tonsils), and tender cervical (“strawberry tongue”). Both skin and tongue may oropharynx with adenopathy (swollen glands). Patients may also have peel during recovery. petechiae, or small headache, malaise, and anorexia. Additional physical Pharyngitis due to GAS is usually a self-limited red spots, on the soft palate. examination findings may include petechiae of the condition with symptoms resolving in 2-5 days even Photo courtesy soft palate and a red, swollen uvula. -

VIRAL MENINGITIS (Nonbacterial Meningitis, Aseptic Meningitis)
VIRAL MENINGITIS (Nonbacterial Meningitis, Aseptic Meningitis) What is VIRAL MENINGITIS? Viral meningitis is an infection of the meninges (a thin lining covering the brain and spinal cord) by any one of a number of different viruses. It is a fairly common disease. Almost all of the cases occur as single, isolated events. Outbreaks are rare. Anyone can get viral meningitis but it occurs most often in children. This type of meningitis should not be confused with the more serious form of Meningococcal meningitis which requires prompt public health intervention to identify and assure treatment of close contacts at risk for contracting the disease. What causes viral meningitis? Approximately half of the cases in the United States are due to common entero (intestinal) viruses. Occasionally, children will have viral meningitis associated with mumps or herpes virus infection. Most people who are infected with enteroviruses either have no symptoms or only get a fever, cold, rash or mouth sores. Only a small number of people with enterovirus infections go on to develop meningitis. What are the symptoms? The symptoms may include fever, headache, stiff neck and fatigue. Rash, sore throat and intestinal symptoms may also occur. Symptoms generally appear within one week of exposure. Symptoms common in infants include fever, irritability and poor feeding. How are the viruses that cause viral meningitis spread? Because a number of different viruses are capable of causing viral meningitis, the manner in which the virus is spread depends upon the type of virus involved. Most cases are due to enteroviruses that may be passed in the stool. -

EUA) of REGEN-COVTM (Casirivimab and Imdevimab
FACT SHEET FOR HEALTH CARE PROVIDERS EMERGENCY USE AUTHORIZATION (EUA) OF REGEN-COVTM (casirivimab and imdevimab) AUTHORIZED USE TREATMENT The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV (casirivimab and imdevimab) supplied as individual vials to be administered together, for the treatment of mild to moderate coronavirus disease 2019 (COVID-19) in adult and pediatric patients (12 years of age and older weighing at least 40 kg) with positive results of direct SARS-CoV-2 viral testing, and who are at high risk for progression to severe COVID-19, including hospitalization or death. Limitations of Authorized Use • REGEN-COV (casirivimab and imdevimab) is not authorized for use in patients: - who are hospitalized due to COVID-19, OR - who require oxygen therapy due to COVID-19, OR - who require an increase in baseline oxygen flow rate due to COVID-19 in those on chronic oxygen therapy due to underlying non-COVID-19 related comorbidity. • Monoclonal antibodies, such as REGEN-COV, may be associated with worse clinical outcomes when administered to hospitalized patients with COVID-19 requiring high flow oxygen or mechanical ventilation. POST-EXPOSURE PROPHYLAXIS The U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization (EUA) to permit the emergency use of the unapproved product, REGEN-COV (casirivimab and imdevimab) co-formulated product and REGEN-COV