Based Nanoparticles for Applications in Oral Drug Delivery So
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Experimental Approach of Minimum Miscibility Pressure for CO2 Miscible Flooding: Application to Egyptian Oil Fields
International Journal of New Technology and Research (IJNTR) ISSN:2454-4116, Volume-2, Issue-5, May 2016 Pages 105-112 Experimental Approach of Minimum Miscibility Pressure for CO2 Miscible Flooding: Application to Egyptian Oil Fields E.M. Mansour, A.M. Al- Sabagh, S.M. Desouky, F.M. Zawawy, M.R. Ramzi The term of “Enhanced Oil Recovery” (EOR) is defined as Abstract— At the present time, carbon dioxide (CO2) miscible the oil that was recovered by any method beyond the primary flooding has become an important method in Enhanced Oil and secondary stage [2]. Enhanced oil recovery processes are Recovery (EOR) for recovering residual oil, and in addition it divided into three categories: gas miscible flooding, thermal may help in protection of the environment as carbon dioxide flooding and chemical flooding [3]. Figure (1) shows oil (CO2) is widely viewed as an important agent in global production from different (EOR) projects with an increasing warming. This paper presents a study of the effect of carbon dioxide (CO ) injection on miscible flooding performance for in the world oil percentage. [4-7]. 2 Egyptian oil fields and focuses on designing and constructing a new miscibility lab with low cost by setup a favorable system for carbon dioxide (CO2) injection to predict the minimum miscibility pressure (MMP) which was required for carbon dioxide (CO2) flooding projects where every reservoir oil sample has its own unique minimum miscibility pressure (MMP). Experimental data from different crude oil reservoirs carried out by slim tube test that is the most common and standard technique of determining minimum miscibility pressure (MMP) in the industry, but this method is expensive, there for we designed this kind of a favorable system (slim tube test) for carbon dioxide (CO2) injection. -

Ordering Tendencies in Pd-Pt, Rh-Pt, and Ag-Au Alloys Z.W
Section I: Basic and Applied Research Ordering Tendencies in Pd-Pt, Rh-Pt, and Ag-Au Alloys Z.W. Lu and B.M. Klein Department of Physics University of California Davis, CA 95616 and A. Zunger National Renewable Energy Laboratory Golden, CO 80401 (Submitted October 7, 1994; in revised form November 9, 1994) First-principles quantum-mechanical calculations indicate that the mixing enthalpies for Pd-Pt and Rh-Pt solid solutions are negative, in agreement with experiment. Calculations of the diffuse-scatter- ing intensity due to short-range order also exhibits ordering tendencies. Further, the directly calcu- lated enthalpies of formation of ordered intermetallic compounds are negative. These ordering tendencies are in direct conflict with a 1959 prediction of Raub that Pd-Pt and Rh-Pt will phase-sepa- rate below ~760 ~ (hence their mixing energy will be positive), a position that has been adopted by all binary alloy phase diagram compilations. The present authors predict that Pdl_xPtx will order in the Llz,Llo, and L12 structures ([001] superstructures)at compositionsx = 4' 2' and 4' respectively, I I while the ordered structures of Rhx_/Ptx are predicted to be superlattices stacked along the [012] di- rections. While the calculated ordering temperatures for these intermetallic compounds are too low to enable direct growth into the ordered phase, diffuse-scattering experiments at higher tempera- tures should reveal ordering rather than phase-separation characteristics (i.e., off-F peaks). The situation is very similar to the case of Ag-Au, where an ordering tendency is manifested both by a dif- fuse scattering intensity and by a negative enthalpy of mixing. -

Measurement and Modeling of Fluid-Fluid Miscibility in Multicomponent Hydrocarbon Systems Subhash C
Louisiana State University LSU Digital Commons LSU Doctoral Dissertations Graduate School 2005 Measurement and modeling of fluid-fluid miscibility in multicomponent hydrocarbon systems Subhash C. Ayirala Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_dissertations Part of the Petroleum Engineering Commons Recommended Citation Ayirala, Subhash C., "Measurement and modeling of fluid-fluid miscibility in multicomponent hydrocarbon systems" (2005). LSU Doctoral Dissertations. 943. https://digitalcommons.lsu.edu/gradschool_dissertations/943 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Doctoral Dissertations by an authorized graduate school editor of LSU Digital Commons. For more information, please [email protected]. MEASUREMENT AND MODELING OF FLUID-FLUID MISCIBILITY IN MULTICOMPONENT HYDROCARBON SYSTEMS A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the Requirements for the degree of Doctor of Philosophy in The Department of Petroleum Engineering by Subhash C. Ayirala B.Tech in Chemical Engineering, Sri Venkateswara Univeristy, Tirupati, India, 1996 M.Tech in Chemical Engineering, Indian Institute of Technology, Kharagpur, India, 1998 M.S. in Petroleum Engineering, Louisiana State University, 2002 August 2005 DEDICATION This work is dedicated to my wife, Kruthi; my parents; my brother, Dhanuj and my beloved sisters, Hema, Suma and Siri. ii ACKNOWLEDGEMENTS I am deeply indebted to my mentor and advisor Dr. Dandina N. Rao for his able guidance, motivation and moral support throughout this work. -
Miscibility in Solids
Name _________________________ Date ____________ Regents Chemistry Miscibility In Solids I. Introduction: Two substances in the same phases are miscible if they may be completely mixed (in liquids a meniscus would not appear). Substances are said to be immiscible if the will not mix and remain two distinct phases. A. Intro Activity: 1. Add 10 mL of olive oil to 10 mL of water. a) Please record any observations: ___________________________________________________ ___________________________________________________ b) Based upon your observations, indicate if the liquids are miscible or immiscible. Support your answer. ________________________________________________________ ________________________________________________________ 2. Now add 10 mL of grain alcohol to 10 mL of water. a) Please record any observations: ___________________________________________________ ___________________________________________________ b) Based upon your observations, indicate if the liquids are miscible or immiscible. Support your answer. ________________________________________________________ ________________________________________________________ Support for Cornell Center for Materials Research is provided through NSF Grant DMR-0079992 Copyright 2004 CCMR Educational Programs. All rights reserved. II. Observation Of Perthite A. Perthite Observation: With the hand specimens and hand lenses provided, list as many observations possible in the space below. _________________________________________________________ _________________________________________________________ -
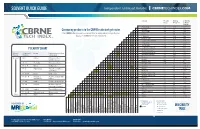
Miscibility Table
Solvent Polarity Boiling Solubility Index Point (°C) in Water (%w/w) Acetic Acid 6.2 118 100 Comparing products in the CBRNE realm just got easier. Acetone 5.1 56 100 Acetonitrile 5.8 82 100 Visit CBRNEtechindex.com to view and lter an independent, comprehensive Benzene 2.7 80 0.18 database of CBRNE detection equipment. n-Butanol 4.0 125 0.43 Butyl Acetate 3.9 118 7.81 Carbon Tetrachloride 1.6 77 0.08 Chloroform 4.1 61 0.815 Cyclohexane 0.2 81 0.01 1,2-Dichloroethane1 3.5 84 0.81 POLARITY CHART Dichloromethane2 3.1 41 1.6 Dimethylformamide 6.4 155 100 Relative Compound Group Representative Solvent Polarity Formula Compounds Dimethyl Sulfoxide3 7.2 189 100 Dioxane 4.8 101 100 Nonpolar R - H Alkanes Petroleum ethers, ligroin, hexanes Ethanol 5.2 78 100 Ethyl Acetate 4.4 77 8.7 Ar - H Aromatics Toluene, benzene Di-Ethyl Ether 2.8 35 6.89 R - O - R Ethers Diethyl ether Heptane 0.0 98 0.0003 R - X Alkyl halides Tetrachloromethane, Hexane 0.0 69 0.001 chloroform Methanol 5.1 65 100 4 R - COOR Esters Ethyl acetate Methyl-t-Butyl Ether 2.5 55 4.8 Methyl Ethyl Ketone5 4.7 80 24 R - CO - R Aldehydes Acetone, methyl ethyl and ketones ketone Pentane 0.0 36 0.004 n-Propanol 4.0 97 100 R - NH Amines Pyridine, triethylamine 2 Iso-Propanol6 3.9 82 100 R - OH Alcohols Methanol, ethanol, Di-Iso-Propyl Ether 2.2 68 isopropanol, butanol Tetrahydrofuran 4.0 65 100 R - COHN2 Amides Dimethylformamide Toluene 2.4 111 0.051 R - COOH Carboxylic acids Ethanoic acid Tichloroethylene 1.0 87 0.11 Water 9.0 100 100 Polar H - OH Water Water Xylene 2.5 139 0.018 4 5 -

In Chemistry, What Is Miscibility? Why Don't They Dissolve? Like Dissolves
In Chemistry, What is Miscibility? Article from Frostburg University Miscibility is the ability of two liquids to mix with each to form a homogeneous solution. Water and ethanol, for example, are miscible. They can be mixed in any proportion, and the resulting solution will be clear and show only one phase. Oil and water, on the other hand, are immiscible. A mixture of vegetable oil and water will always separate into two layers, and won't dissolve in each other. Other solvents are only partially miscible, meaning that only some portion will dissolve in water. Most of the liquids encountered in everyday life are either water-based, called aqueous, or organic, which in the chemical sense means they contain carbon atoms. These can generally be divided into two broad classes. They're either polar or nonpolar. Polar molecules are molecules that have a positive end and a negative end. Nonpolar molecules do not have positive and negative ends. They have the same charge or no charge throughout the molecule. Why don’t they dissolve? Like dissolves Like! Polar solvents are miscible with polar solutes. Nonpolar solvents are miscible with nonpolar solutes. Polar solutes like salt, NaCl, is easily dissolved by polar solvents like water. The figure to the left shows how water molecules dissolve a salt crystal because of the polarity. The positive end of water molecules are attracted to the negative chlorine ions and the negative end of the water molecules are attracted to positive sodium ions. Immiscible solvents are those that do not mix. Water and oil are immiscible because water is polar and oil is nonpolar. -

Liquid–Liquid Extraction of Actinides, Lanthanides, and Fission Products by Use of Ionic Liquids: from Discovery to Understanding
Anal Bioanal Chem (2011) 400:1555–1566 DOI 10.1007/s00216-010-4478-x REVIEW Liquid–liquid extraction of actinides, lanthanides, and fission products by use of ionic liquids: from discovery to understanding Isabelle Billard & Ali Ouadi & Clotilde Gaillard Received: 13 October 2010 /Revised: 19 November 2010 /Accepted: 25 November 2010 /Published online: 4 January 2011 # Springer-Verlag 2010 Abstract Liquid–liquid extraction of actinides and lantha- policies favor direct disposal in deep geological reposito- nides by use of ionic liquids is reviewed, considering, first, ries. Whatever the choice made nowadays, the future of phenomenological aspects, then looking more deeply at the nuclear energy, stimulated by the world demand for energy, various mechanisms. Future trends in this developing field are will require new waste-management policies, guided by presented. new regulations and economic obligations, centered on future nuclear reactors, most probably emerging from the Keywords Actinides . Lanthanides . Liquid–liquid generation IV program. In this context, ionic liquids, extraction . Ionic liquids already used in various industrial fields [1], may prove useful. Thus, this paper reviews the emerging field of Abbreviations liquid–liquid extraction of actinides (An), lanthanides (Ln), CMPO Carbamoyl-methyl phosphine oxide and fission products (mainly Sr and Cs but in a few cases TBP Tributyl phosphate we will refer to works devoted to other metallic species) by TODGA N,N,N′,N′-Tetra(n-octyl)diglycolamide use of ionic liquids (ILs). Owing to limited space, the TTA Thenoyltrifluoroacetone reader is referred to some recent excellent reviews on ILs or on An and Ln in ILs [2–5]. We simply define ionic liquids as salts with melting points below 100°C. -

Extraction.Pdf
Extraction A useful technique for purification of mixture Dr. Zerong Wang at UHCL Separation processes Liquid-liquid extraction Adsorption Filtration Solid-liquid extraction (leaching) Elution chromatography Membrane separation processes Distillation Affinity separation processes Drying and evaporation Freeze-drying (lypholyzation) Precipitation Crystallization Electrophoresis Centrifugation Mechanical sieving Dialysis Dr. Zerong Wang at UHCL 1 Extraction Extraction is a purification technique in which compounds with different solubilities are separated using solvents of different polarities. This basic chemical process is often performed in conjunction with reversible acid/base reactions. Dr. Zerong Wang at UHCL Type of Extraction Liquid-Solid Extraction Liquid-Liquid Extraction Dr. Zerong Wang at UHCL 2 Liquid-Solid Extraction Brewing tea Percolating coffee Spices and herbs Dr. Zerong Wang at UHCL Leaching (Liquid-Solid Extraction) Diffusion of the solute out of the solid and into the liquid solvent is mostly the controlling step. Principle of separation: preferential solubility Created or added phase: liquid Separating agent: liquid solvent Dr. Zerong Wang at UHCL 3 Liquid-Liquid Extraction Dr. Zerong Wang at UHCL Liquid-Liquid Extraction Used when distillation is impractical The mixture to be separated is heat sensitive. Volatility differences are much too small. The mixture forms a azeotropic mixture Solute concentration is low Dr. Zerong Wang at UHCL 4 Liquid-Liquid Extraction Principle Different species with different solubilities in the two immiscible liquid phases, i.e., these species have different partition behavior in different phases. Dr. Zerong Wang at UHCL Applications of Liquid-liquid extraction Separation of aromatics from aliphatic hydrocarbons Purification of antibiotics Purification of aromatics such as benzene, xylene and toluene Protein purification using aqueous two-phase systems Purification of natural products Purification of dyes and pigments Metallurgical purifications Dr. -

Experiment 3: Studying Density, Miscibility and Solubility of Liquids
04Lab | Experiment 3: Studying Density, Miscibility and Solubility of liquids Objective The goal of this experiment is to determine the densities of three unknown liquid, test the miscibility of each liquid to each other and the solubility of iodine in each liquid. Materials o Three 13 x 100 mm Test tubes o One 18 x 150 mm Test tubes o 10 mL plastic graduated cylinder o Stirring Rod o Berel Pipets o Liquid- A o Liquid - B o Liquid - C o Iodine Crystals o Distilled water Introduction Reading: Ch 2.4 & Ch 9.3, Chemistry in our Lives Timberlake . “Matter & Energy.” Pay special attention to the sections on solubility found in chapter 9.3. Density, Miscibility and Solubility How do water and oil mix at the molecular level? Does oil sink or float in water? Are the two liquids miscible in each other? The answer to these questions will be investigated in this experiment. Physical properties such as densities and miscibility of various liquids in water may help provide answers to these questions. An observable (or measurable) property of matter i.e., color, bpt, mpt, conductivity, texture, miscibility specific heat and density are important in helping identify different substances and how they interact with each other. Consider what occurs when vinegar and oil are mixed in Italian salad dressing. The oil floats on top and the vinegar and the herbs sinks to the bottom. We say that the oil is less dense than the vinegar. We can also state that oil and vinegar are immiscible. Density (d or �) is defined as the mass per unit volume. -

Molecular Driving Forces Behind the Tetrahydrofuran−Water Miscibility
Article pubs.acs.org/JPCB Molecular Driving Forces behind the Tetrahydrofuran−Water Miscibility Gap † ‡ † § † † † ‡ Micholas Dean Smith, , Barmak Mostofian, , Loukas Petridis, Xiaolin Cheng, and Jeremy C. Smith*, , † Center for Molecular Biophysics, University of Tennessee and Oak Ridge National Laboratory, Oak Ridge, Tennessee 37830, United States ‡ Department of Biochemistry and Cellular Molecular Biology, University of Tennessee, M407 Walters Life Sciences, 1414 Cumberland Avenue, Knoxville, Tennessee 37996, United States § Joint Institute for Biological Sciences, University of Tennessee and Oak Ridge National Laboratory, Oak Ridge, Tennessee 37830, United States *S Supporting Information ABSTRACT: The tetrahydrofuran−water binary system exhibits an unusual closed-loop miscibility gap (transitions from a miscible regime to an immiscible regime back to another miscible regime as the temperature increases). Here, using all-atom molecular dynamics simulations, we probe the structural and dynamical behavior of the binary system in the temperature regime of this gap at four different mass ratios, and we compare the behavior of bulk water and tetrahydrofuran. The changes in structure and dynamics observed in the simulations indicate that the temperature region associated with the miscibility gap is distinctive. Within the miscibility-gap temperature region, the self- diffusion of water is significantly altered and the second virial coefficients (pair- interaction strengths) show parabolic-like behavior. Overall, the results suggest that the gap is the result of differing trends with temperature of minor structural changes, which produces interaction virials with parabolic temperature dependence near the miscibility gap. ■ INTRODUCTION presence of voids,9,10,13 a preferred T-like orientation for 9,10 Tetrahydrofuran (THF) is a ubiquitous organic solvent. -

Miscibility Gaps in Fused Salts. Note XI. Systems Formed with Silver
Miscibility Gaps in Fused Salts. Note XI. Systems Formed with Silver Halides and Lithium or Sodium Halides Giorgio Flor, Chiara Margheritis, Giuseppina Campari Vigano', and Cesare Sinistri Centro di studio per la termodinamica ed elettrochimica dei sistemi salini fusi e solidi del C.N.R. Institute of Physical Chemistry, University of Pavia, Italy Z. Naturforsch. 37 a, 1068-1072 (1982); received June 3, 1982 The salt families formed with silver halides and lithium or sodium halides were studied in order to investigate demixing in the liquid state. In particular, measurements were carried out on the stable diagonals of the 12 pertinent reciprocal ternaries. Liquid-liquid equilibria were found to occur in the 10 mixtures containing LiF, NaF, LiCl, LiBr and NaCl (the last one only in the presence of Agl). The miscibility gap, however, could be fully measured only on the four mixtures AgBr-(-LiCl, Agl + LiCl, Agl + LiBr and Agl + NaCl: for these and for the mixture Agl + NaBr an "a priori" prediction of the gap was possible on the basis of current thermodynamic theories. The systematic analysis of demixing in mixtures Apparatus and Materials of fused salts is continued with the present paper The apparatus and the experimental technique which reports on the families formed with silver (based on the direct visual observation of the sample, halides and lithium or sodium halides. possibly supported by DTA measurements) were In each of the two groups of reciprocal ternaries described in previous papers of this series [3]. AgX + LiY and AgX + NaY (X, Y = F, CI, Br, I), The salts used were Merck Suprapur lithium and 4 binaries with a common ion, 6 unstable diagonals sodium halides and Fluka puriss. -

Physical Pharmacy
Physical pharmacy Lec 1 dr basam al zayady Solubility and Distribution Phenomena Solubility is defined in quantitative terms as the concentration of solute in a saturated solution at a certain temperature, and in a qualitative way, it can be defined as the spontaneous interaction of two or more substances to form a homogeneous molecular dispersion. Solubility is an intrinsic material property that can be altered only by chemical modification of the molecule, in contrast to this, dissolution is an extrinsic material property that can be influenced by various chemical, physical, or crystallographic means such as complexation, particle size, surface properties, solid-state modification, or solubilization enhancing formulation strategies. The solubility of a compound depends on the physical and chemical properties of the solute and the solvent as well as on such factors as temperature, pressure, the pH of the solution The thermodynamic solubility of a drug in a solvent is the maximum amount of the most stable crystalline form that remains in solution in a given volume of the solvent at a given temperature and pressure under equilibrium conditions. Thermodynamic equilibrium is achieved when the overall lowest energy state of the system is achieved. This means that only the equilibrium solubility reflects the 1 balance of forces between the solution and the most stable, lowest energy crystalline form of the solid. Solubility Expressions The solubility of a drug may be expressed in a number of ways. The United States Pharmacopeia (USP) describes the solubility of drugs as parts of solvent required for one part solute. Solubility is also quantitatively expressed in terms of molality, molarity, and percentage.