Table 7-1 Glaucoma Medications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
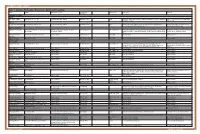
Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg
OPTOMETRIC STUDY CENTER Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg. % Product Sizes Side Effects Warnings Reduction CHOLINERGIC AGENTS Direct Pilocarpine (generic) Pilocarpine 1%, 2%, 4% Increases trabecular outflow BID-QID/15-25% 15ml Headache, blurred vision, myopia, retinal detachment, bronchiole constriction, Angle closure, shortness of breath, retinal narrowing of angle detachment Indirect Phospholine Iodide (Pfizer) Echothiophate iodide 0.125% Increases trabecular outflow QD-BID/15-25% 5ml Same as above plus cataractogenic iris cysts in children, pupillary block, Same as above, plus avoid prior to any increased paralysis with succinylcholine general anesthetic procedure ALPHA-2 AGONISTS Alphagan P (Allergan) Brimonidine tartrate 0.1%, 0.15% with Purite Decreases aqueous production, increases BID-TID/up to 26% 5ml, 10ml, 15ml Dry mouth, hypotension, bradycardia, follicular conjunctivitis, ocular irritation, Monitor for shortness of breath, dizziness, preservative uveoscleral outflow pruritus, dermatitis, conjunctival blanching, eyelid retraction, mydriasis, drug ocular redness and itching, fatigue allergy Brimonidine tartrate Brimonidine tartrate 0.15%, 0.2% Same as above Same as above 5ml, 10ml Same as above Same as above (generic) Iopidine (Novartis) Apraclonidine 0.5% Decreases aqueous production BID-TID/up to 25% 5ml, 10ml Same as above but higher drug allergy (40%) Same as above BETA-BLOCKERS Non-selective Betagan (Allergan) Levobunolol 0.25%, 0.5% Decreases -

NEW ZEALAND DATA SHEET 1. PRODUCT NAME IOPIDINE® (Apraclonidine Hydrochloride) Eye Drops 0.5%
NEW ZEALAND DATA SHEET 1. PRODUCT NAME IOPIDINE® (apraclonidine hydrochloride) Eye Drops 0.5%. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each mL of Iopidine Eye Drops 0.5% contains apraclonidine hydrochloride 5.75 mg, equivalent to apraclonidine base 5 mg. Excipient with known effect Benzalkonium chloride 0.1 mg per 1 mL as a preservative. For the full list of excipients, see section 6.1. 2. PHARMACEUTICAL FORM Eye drops, solution, sterile, isotonic. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Iopidine Eye Drops 0.5% are indicated for short-term adjunctive therapy in patients on maximally tolerated medical therapy who require additional IOP reduction. Patients on maximally tolerated medical therapy who are treated with Iopidine Eye Drops 0.5% to delay surgery should have frequent follow up examinations and treatment should be discontinued if the intraocular pressure rises significantly. The addition of Iopidine Eye Drops 0.5% to patients already using two aqueous suppressing drugs (i.e. beta-blocker plus carbonic anhydrase inhibitor) as part of their maximally tolerated medical therapy may not provide additional benefit. This is because apraclonidine is an aqueous-suppressing drug and the addition of a third aqueous suppressant may not significantly reduce IOP. The IOP-lowering efficacy of Iopidine Eye Drops 0.5% diminishes over time in some patients. This loss of effect, or tachyphylaxis, appears to be an individual occurrence with a variable time of onset and should be closely monitored. The benefit for most patients is less than one month. 4.2. Dose and method of administration Dose One drop of Iopidine Eye Drops 0.5% should be instilled into the affected eye(s) three times per day. -

Pharmacology of Ophthalmologically Important Drugs James L
Henry Ford Hospital Medical Journal Volume 13 | Number 2 Article 8 6-1965 Pharmacology Of Ophthalmologically Important Drugs James L. Tucker Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Chemicals and Drugs Commons, Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Tucker, James L. (1965) "Pharmacology Of Ophthalmologically Important Drugs," Henry Ford Hospital Medical Bulletin : Vol. 13 : No. 2 , 191-222. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol13/iss2/8 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. For more information, please contact [email protected]. Henry Ford Hosp. Med. Bull. Vol. 13, June, 1965 PHARMACOLOGY OF OPHTHALMOLOGICALLY IMPORTANT DRUGS JAMES L. TUCKER, JR., M.D. DRUG THERAPY IN ophthalmology, like many specialties in medicine, encompasses the entire spectrum of pharmacology. This is true for any specialty that routinely involves the care of young and old patients, surgical and non-surgical problems, local eye disease (topical or subconjunctival drug administration), and systemic disease which must be treated in order to "cure" the "local" manifestations which frequently present in the eyes (uveitis, optic neurhis, etc.). Few authors (see bibliography) have attempted an introduction to drug therapy oriented specifically for the ophthalmologist. The new resident in ophthalmology often has a vague concept of the importance of this subject, and with that in mind this paper was prepared. -

Glaucoma Pharmacology A-Z Selecting Therapy Prostaglandin
1/6/2014 PGAs • QHS dosing • Long duration of action Glaucoma Pharmacology A-Z • Flatten diurnal curve • Effective on trough and peak IOP Eric E. Schmidt, O.D. • No systemic side effects Omni Eye Specialists Wilmington, NC • Little tachyphylaxis [email protected] Selecting Therapy PGAs 2008 • Goals of primary therapy • Bimatoprost (Lumigan) – Achieve lowest IOP on monotherapy – High response rate—few to no nonresponders • Latanoprost (Xalatan) – Maintain consistent IOP lowering – Obtain patient compliance and adherence by meeting their goals and expectations • Travaprost, Travaprost Z (Travatan, Travatan Z) • Building-block approach to medical therapy – Establish the strongest foundation prior to resorting to adjunctive therapy Prostaglandin analogs Prostaglandin Side Effects • Lower IOP by enhancing uveoscleral • Conjunctival hyperemia: Severe outflow hyperemia • They also reduce episcleral venous – Lumigan 3.5% – Travatan 1.5% pressure – Xalatan <1% – Rescula 1% • PGAs work by causing up to a 26% • Is this a transient phenomenon? reduction in resistance to outflow • Is it an allergic conjunctivitis? • Breaks down collagen in the uveoscleral • Is it worth stopping the drop? meshwork • Create new channels for outflow 1 1/6/2014 Conjunctival hyperemia Prostaglandins • PGAs have an effect on EP receptors • Oh sure, we know they are good, but just which are vasodilators how good are they? – Average IOP drop of 34% • The stronger the drug binds to that – Improved compliance receptor the more pronounced the – Excellent safety profiles -

Understanding and Living with Glaucoma
Understanding and Living with Glaucoma Betty hopes future generations won’t have to live with glaucoma. Dr. Goldberg’s breakthrough research could mean they won’t have to. Understanding and Living with Glaucoma C SUPPORTED BY AN EDUCATIONAL GRANT FROM AERIE PHARMACEUTICALS, INC. Glaucoma is an eye disease that gradually steals your vision. Usually, glaucoma has no symptoms in its early stages. But without proper treatment glaucoma can lead to blindness. The good news is that with regular eye exams, early detection, and treatment, you can preserve your sight. This guide will give you a complete introduction to the facts about glaucoma. D Glaucoma Research Foundation 2 INTRODUCTION 3 UNDERSTANDING GLAUCOMA 3 Understand the Eye to Understand Glaucoma 4 How Glaucoma Affects the Eye 6 Who Gets Glaucoma? 7 Are There Symptoms? 7 When Should You Get Your Eyes Checked for Glaucoma? 8 DIFFERENT TYPES OF GLAUCOMA 8 Primary Open-Angle or Open-Angle Glaucoma 9 Primary Angle-Closure or Angle-Closure Glaucoma or Narrow-Angle Glaucoma 10 Other Types of Glaucoma 10 • Normal-Tension Glaucoma 10 • Secondary Glaucoma 12 DETECTING GLAUCOMA 12 How Is Glaucoma Diagnosed? 12 What To Expect During Glaucoma Examinations 12 • Tonometry 12 • Ophthalmoscopy 15 • Perimetry 16 • Gonioscopy 16 • Pachymetry 17 TREATING GLAUCOMA 17 Treatment of Primary Open-Angle Glaucoma 17 • Selective Laser Trabeculoplasty 18 • Glaucoma Medications 21 • Incisional Surgeries 25 • Unapproved Treatments 25 Treatment of Primary Angle-Closure Glaucoma 26 Treatment of Other Types of Glaucoma 28 FREQUENTLY ASKED QUESTIONS 30 LIVING WITH GLAUCOMA 30 Working with Your Doctor 32 Responding to Vision Changes Due to Glaucoma 32 Questions For Your Doctor 34 Your Lifestyle Counts 35 Looking Ahead 36 APPENDIX 36 A Guide To Glaucoma Medications 38 Glossary Understanding and Living with Glaucoma 1 Introduction If you have been diagnosed with glaucoma, or are a glaucoma suspect, you probably have a lot of questions and some concerns. -

Prostaglandin Analogs Prostaglandin Analogs
9/26/2017 Disclosure Statement “I have no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or Joseph Bergmann, MD provider(s) of commercial services discussed in this CME activity.” Medical Treatment Medical Treatment Is it effective / How does it work? Oral Is it safe / What are the side effects? Methazolamide Acetazolamide Is it expensive? Topical How do I take my drops Prostaglandins Do I need to do this my whole life? Beta-blockers Alpha-adrenergic Carbonic Anhydrase Inhibitors Cholinergic Agonists Rho Kinase Inhibitors Oral Carbonic Anhydrase Oral Carbonic Anhydrase Inhibitors Inhibitors Preparations/ Dosing Anatomy/ Physiology/ Pharmacokinetics Side Effects Cost 1 9/26/2017 Oral CAIs Oral CAI’s: Side Effects How is it available? Allergy Methazolamide ○ 25-50mg 2-3 times daily Rare Acetazolamide ○ 250-500 mg standard release dosed 4-6 hours Aplastic anemia, Thrombocytopenia, ○ 500 mg Sequels (standard release) dosed 12 hours Agranulocytosis How it works Decrease aqueous humor formation by direct antagonist activity on Hypokalemia ciliary epithelial carbonic anhydrase Create systemic acidosis Common 90% of enzyme must be inhibited for it to be effective Methazolamide is liver metabolized, acetazolamide is kidney GI: nausea, diarrhea, weight loss, metallic taste metabolized Nervous: Lethargy, depression, parathesias, Action Onset within 1 hour decreased libido Peak 2-4 hours (sustained release Renal: Kidney stones duration “Hangover” Oral CAI’s: Cost Prostaglandin Acetazolamide Regular and Sustained Release (Diamox Analogs Sequels) ○ $$$ Methazolamide $$$ Prostaglandin Analogs Prostaglandin Analogs How is it available? How it works Prostamides Improves aqueous outflow Bimatoprost, Latanoprost, Travaprost Pressure dependent and independent ○ Xalatan introduced in 1996 Elevated presence of metalloproteinases--- ○ Once daily dosing breaking down the collagen matrix within the uveoscleral region that surround the ciliary Decosanoid muscle bundles. -

Cvs Caremark ® Maintenance Drug List
CVS CAREMARK® MAINTENANCE DRUG LIST EFFECTIVE AS OF 03/03/2021 Maintenance drugs are prescriptions commonly used to treat conditions that are considered chronic or long-term. These conditions usually require regular, daily use of medicines. Examples of maintenance drugs are those used to treat high blood pressure, heart disease, asthma and diabetes. Due to the large number of available medicines, this list is not all inclusive. Please note that this list does not guarantee coverage and is subject to change. Your prescription benefit plan may not cover certain products or categories, regardless of their appearance on this list. Where a generic is available, it is listed by the generic name. If no generic is available, then the brand name appears. This list represents brand products in CAPS and generic products in lower case italics. If you have questions about your prescription benefits, please log on to your account at Caremark.com or call Customer Care at the number on your ID card. Allergies pentoxifylline Depression desloratidine prasugrel bupropion levocetirizine ticlopidine citalopram ZONTIVITY desvenlafaxine Alzheimer’s Disease duloxetine donepezil Cancer escitalopram galantamine anastrozole fluoxetine memantine exemestane fluvoxamine rivastigmine letrozole mirtazapine NAMZARIC tamoxifen nefazodone toremifene paroxetine Antipsychotics sertraline trazodone Aripiprazole Contraceptives venlafaxine brexipiprazole ethinyl estradiol-desogestrel APLENZIN loxapine ethinyl estradiol-drospirenone FETZIMA olanzapine ethinyl estradiol-ethynodiol -

206185Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 206185Orig1s000 SUMMARY REVIEW Deputy Division Director and Cross-Discipline Team Leader Review NDA 206185 Date August 24, 2018 From Wiley A. Chambers, M.D., William M. Boyd, M.D. Subject Deputy Division Director and Cross-Discipline Team Leader Review NDA # 206185 Applicant Sun Pharma Global FZE U.S Representative: Sun Pharmaceuticals Industries, Inc. Date of Submission 5/7/2018 PDUFA Goal Date 11/7/2018 Type of Application 505(b)(2) Name Xelpros (latanoprost ophthalmic emulsion) 0.005% Dosage forms / Strength Topical ophthalmic emulsion Proposed Indication(s) Reduction of intraocular pressure in patients with open-angle glaucoma or ocular hypertension Regulatory Action: Approval 1. Introduction NDA 206185, Xelpros (latanoprost ophthalmic emulsion) 0.005% was submitted as a 505(b)(2) application referencing the Agency’s summary findings for NDA 20-597, Xalatan (latanoprost ophthalmic solution). The proposed indication is the same as that approved for Xalatan, the reduction of intraocular pressure in patients with open-angle glaucoma or ocular hypertension. Previous action letters for this application cited facilities which were not incompliance with cGMPs. A May 7, 2018, submission to the new drug application served as a complete, class 2 response to the December 19, 2016, action letter. The manufacturing and testing facilities for this NDA are now deemed acceptable and an overall “Approval” recommendation was entered in Panorama by the Office of Process and Facilities (OPF) on 6-26-2018. Although numerically inferior to Xalatan (latanoprost ophthalmic solution) 0.005%, the IOP reduction is a clinically significant reduction in IOP and represents a benefit over the potential risks of using the product. -

Drugs That May Be Used Based on Licensure Designation Page 1 of 7 Updated February 2021 by the Pennsylvania State Board of Optometry
Drugs Which May Be Used Based on Licensure Designation Approved Drugs a.) Administration and prescription of pharmaceutical agents for therapeutic purposes. Optometrists who are certified to prescribe and administer pharmaceutical agents for therapeutic purposes under section 4.1 of the Optometric Practice and Licensure Act (63 P. S. § 244.4a), may prescribe and administer the drugs listed in subsections (c)(1) – (11) below in their practice of optometry. See also 49 Pa. Code § 23.202 for the application procedure for optometrists to administer and prescribe pharmaceutical agents for therapeutic purposes. b.) Administration and prescription of pharmaceutical agents to treat glaucoma. Optometrists who are certified to prescribe and administer pharmaceutical agents to treat glaucoma under section 4.2 of the Optometric Practice and Licensure Act (63 P.S. § 244.4b), may prescribe and administer the drugs listed in subsection (c)(12) below in their practice of optometry. See also 49 Pa. Code § 23.205 for the application procedure for optometrists to administer and prescribe pharmaceutical agents to treat glaucoma. c.) DEA registration reminder. Licensees who hold, or plan to obtain, a DEA registration are reminded to review and comply with PDMP standards. d.) Allowable pharmaceutical products. Optometrists may prescribe and administer the following pharmaceutical products or the A-rated generic therapeutically equivalent drug: (1) Topical Anesthetics (i) benoxinate (ii) lidocaine (iii) proparacaine (iv) tetracaine (2) Topical Ocular Lubricants -

Clinical Considerations with Glaucoma
Clinical Considerations With Glaucoma Ralph E. Hamor DVM, MS, DACVO Glaucoma is a leading cause of blindness in the middle-aged dog. Glaucoma should be considered as one of the "rule outs" in any case of "red eye" or "watery eye," especially in predisposed breeds (see lists below). Glaucoma is characterized by an elevation of intraocular pressure (IOP) that results in progressive loss of retinal ganglion cells and their axons. Aqueous, produced by the ciliary body, flows from the posterior chamber through the pupil into the anterior chamber and drains out of the eye via the trabecular meshwork in the iridocorneal angle and into the intrascleral venous plexus (conventional outflow). Uveoscleral (unconventional) outflow also occurs in most species: aqueous flows into the vitreous, across the uveal tract, along the supraciliary-suprachoroidal space into the adjacent sclera. Uveoscleral outflow accounts for 3% of aqueous outflow in the cat, 13% in rabbits, 15% in dogs and may be up to 50% in the horse. Increased IOP results from obstruction to outflow, not an increase in aqueous production. Whatever the cause, the most important consideration is whether the glaucoma is primary or secondary. PRIMARY GLAUCOMA occurs when there is no recognizable cause of the glaucoma. These patients are born with either an abnormal drainage angle, a drainage angle that becomes abnormal, or a drainage angle that appears normal but ceases to function normally. In some cases, gonioscopy (evaluation of the external drainage angle) demonstrates that a patient has an abnormal appearing drainage angle. This finding is only a risk factor that the patient will develop clinical signs of glaucoma. -
Delivery Device for a Controlled Drug Release of an Active Agent Into The
(19) & (11) EP 1 671 624 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 9/00 (2006.01) A61K 31/58 (2006.01) 11.08.2010 Bulletin 2010/32 (21) Application number: 05025475.4 (22) Date of filing: 29.04.2004 (54) Delivery device for a controlled drug release of an active agent into the posterior section of the eye System zur kontrollierten Freisetzung eines bioaktiven Wirkstoffs im hinteren Bereich des Auges Un système bioactive pour la libération controlée d’un agent bioactif dans la section postérieure oculaire (84) Designated Contracting States: • Lawin, Laurie R. AT BE BG CH CY CZ DE DK EE ES FI FR GB GR New Brighton, Minnesota 55112 (US) HU IE IT LI LU MC NL PL PT RO SE SI SK TR • Shen, Byron C. Eden Prairie, Minnesota 55347 (US) (30) Priority: 02.05.2003 US 467419 P • De Juan, Eugene La Canada, California 91011 (US) (43) Date of publication of application: • Varner, Signe E. 21.06.2006 Bulletin 2006/25 Los Angeles, California 90065 (US) • Chappa, Ralph A. (62) Document number(s) of the earlier application(s) in Prior Lake, Minnesota 55372 (US) accordance with Art. 76 EPC: 04750957.5 / 1 633 320 (74) Representative: Vossius & Partner Siebertstrasse 4 (73) Proprietor: SurModics, Inc. 81675 München (DE) Eden Prairie, MN 55344-3523 (US) (56) References cited: (72) Inventors: WO-A-02/074196 US-A1- 2002 188 037 • Anderson, Aron B. Minnetonka, Minnesota 55343 (US) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Ocular Toxicology and Pharmacology
Ocular Toxicology and Pharmacology Susan Schneider, MD Vice President, Retina Acucela Inc [email protected] Ocular Toxicology “The remedy often times proves worse than the disease” - William Penn Ocular Toxicology Site Affected Ocular Toxicology: Corneal and Lenticular • Chloroquine & hydroxychloroquine • Indomethacin • Amiodarone • Tamoxifen • Suramin • Chlorpromazine (corneal endothelium) • Gold salts (chrysiasis) Causes of Corneal “Swirl” Keratopathy • Chloroquine • Suramin (used in AIDS patients) • Tamoxifen • Amiodarone Ocular Toxicology: Transient Myopia • Sulfonamides • Tetracycline • Perchlorperazine (Compazine) • Steroids • Carbonic anhydrase inhibitors Ocular Toxicology: Conjunctival, Eyelid, Scleral • Isoretinoin: DES, blepharoconjunctivitis • Chlorpromazine: Slate-blue discoloration • Niacin: Lid edema • Gold salts: Conjunctiva • Tetracycline: Conjunctival inclusion cysts • Minocycline: Bluish discoloration of sclera Ocular Toxicology: Uveal Rifabutin: • Anterior uveitis +/- vitritis, associated with hypopyon • Resolves after discontinuation of medication Ocular Toxicology: Lacrimal system Decreased tearing: Increased tearing: • Anticholinergics • Adrenergic agonists • Antihistamines • Antihypertensives • Vitamin A analogs • Cholinergic agonists • Phenothiazines • Antianxiety agents • Tricyclic antidepressants Ocular Toxicology: Retinal • Chloroquine (Aralen) & Hydroxychloroquine (Plaquenil): Bull’s eye maculopathy • Thioridazine (Mellaril): +/-decreased central vision, pigment stippling, circumscribed RPE dropout • Quinine: