Long Term Results of Rotating Hinge Total Knee Arthroplasty in Complex Primary and Revision Cases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Scientific Program 2021APAS Virtual Saturday 10, 17, 24 July 2021 Apas2021.Com Platinum Sponsors Stryker
Scientific Program 2021APAS Virtual Saturday 10, 17, 24 July 2021 apas2021.com Platinum Sponsors stryker Titanium Sponsor Corin Connected Orthopaedic Insight SATURDAY 10 JULY 2021 All Times are AEST - Sydney, Australia Session 1K&H 12.00pm - 1.00pm Opening Ceremony & Plenary Knee & Hip Auditorium Moderator - Nicolaas Budhiparama Co-Moderators - Li Cao, Parag Sancheti 12.00pm Welcome message - President of APAS/ASIA/APKS Nicolaas Budhiparama Virtual Handover of APAS Presidential Medal Li Cao, Yan Wang, Parag Sancheti 12.15pm Presidential Guest Speaker - How to get more out of what you read in Orthopaedic Journals Seth Leopold 12.30pm APAS Guest Speaker - VTE: money, politics or patient outcomes Javad Parvizi 12.45pm Q&A KNEE AUDITORIUM HIP AUDITORIUM Session 2K 1.00pm - 2.15pm Session 2H 1.00pm - 2.30pm Live Surgery Hip Session - Dual Mobility and Approaches Moderator 1 - Jim Sullivan Moderator 2 - Muhammad Amin Chinoy Moderator and Panel: Sebastien Parratte / Parag Sancheti / Nicolaas Budhiparama 1.00pm Robot assist cementless Persona TKA - ROSA 1.00pm Direct anterior THA: here to stay - Jim Sullivan Surgeon - Rami Sorial 1.07pm Minimally invasive hip philosophy and results on posterior approach variants Nepean private hospital, Sydney, Australia Sol Qurashi 2.00pm Q&A 1.14pm Dysplastic Acetabulum : acetabuloplasty, PISA technique or combined? - Ismail H. D. 2.15pm Session Ends 1.21pm Management of Fracture Upper end of Femur in Elderly, A dilemma - Osteosynthesi or Bipolar or THA or Dual Mobility hip, A rational approach - Chandra Yadav 1.28pm Anterior Hip Replacement in a Community Setting Off the Table. - Umar Burney 1.35pm Q&A 1.50pm Reconstructing posterior capsule- a new technique for increasing stability with THA Guoqiang Zhang 1.57pm Dual mobility articulations in THR .When and why? - Andrew Shimmin 2.04pm Primary difficult Total Hip Arthroplasty for Acetabular fracture - Ismail H. -
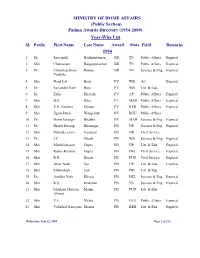
(Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl. Prefix First Name Last Name Award State Field Remarks 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs Expired 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs Expired 3 Dr. Chandrasekhara Raman BR TN Science & Eng. Expired Venkata 4 Shri Nand Lal Bose PV WB Art Expired 5 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 6 Dr. Zakir Hussain PV AP Public Affairs Expired 7 Shri B.G. Kher PV MAH Public Affairs Expired 8 Shri V.K. Krishna Menon PV KER Public Affairs Expired 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & Eng. Expired 11 Dr. Shanti Swarup Bhatnagar PB UP Science & Eng. Expired 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. J.C. Ghosh PB WB Science & Eng. Expired 14 Shri Maithilisharan Gupta PB UP Litt. & Edu. Expired 15 Shri Radha Krishan Gupta PB DEL Civil Service Expired 16 Shri R.R. Handa PB PUN Civil Service Expired 17 Shri Amar Nath Jha PB UP Litt. & Edu. Expired 18 Shri Malihabadi Josh PB DEL Litt. & Edu. 19 Dr. Ajudhia Nath Khosla PB DEL Science & Eng. Expired 20 Shri K.S. Krishnan PB TN Science & Eng. Expired 21 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmed 22 Shri V.L. Mehta PB GUJ Public Affairs Expired 23 Shri Vallathol Narayana Menon PB KER Litt. & Edu. Expired Wednesday, July 22, 2009 Page 1 of 133 Sl. Prefix First Name Last Name Award State Field Remarks 24 Dr. -

Symposium – Polytrauma
Welcome Messages ............................................................................................ 8 Organising Committees .................................................................................... 10 About SICOT ....................................................................................................... 11 SICOT General Assembly ................................................................................... 12 Awards ................................................................................................................ 13 SICOT Diploma Examination ............................................................................. 17 Scientific Programme ....................................................................................... 19 General Information ........................................................................................... 19 Peer Reviewers ................................................................................................... 22 Invited Speakers ................................................................................................. 24 Moderators ......................................................................................................... 27 Programme Colour Scheme .............................................................................. 28 Plenary Sessions ................................................................................................. 29 Partner Societies ............................................................................................... -

ISHKS-2021-Scientifi
PROGRAM OVERVIEW INDIAN SOCIETY OF VIRTUAL HIP & KNEE SURGEONS ISHKS 2021 ESTB. : 2004 Regd. No. : E - 23526 (Mumbai) 16 - 18 APRIL ORGANIZING TEAM Dr. Hemant Wakankar Dr. A.V. Gurava Reddy President Organizing Chairman REGISTER NOW CLICK HERE Dr. A.B. Suhas Dr. Adarsh Dr. Kushal Dr. Praharsha www.ishks2021.com Masilamani Annapareddy Hippalgaonkar Mulpur INTERNATIONAL FACULTY USA USA USA USA Dr. Amar S. Ranawat Dr. Alejandro Gonzalez Dr. Jonathan Vigdorchik Dr. Seth A. Jerabek Hospital for Della Valle Hospital for Hospital for Special Surgery (HSS) Hospital for Special Surgery (HSS) Special Surgery (HSS) Special Surgery (HSS) USA USA USA USA Dr. Matt Austin Dr. Neil P. Sheth Dr. Sean D. Toomey Dr. Raymond Robinson Swedish Orthopedic Institute University of Miami Rothman Institute University of Pennsylvania CANADA USA USA UK Dr. Victor Hernandez Dr. Ram Yakkanti Dr. Mohit Bhandari Dr. Chris A Dodd Nuffield Orthopaedic McMaster University University of Miami University of Miami Centre and Oxford University Hospital UK UK Dr. Nikhil Shah Dr. Vikas Khanduja Wrightington Cambridge University NATIONAL FACULTY Ashok Rajgopal Arun Mullaji Anoop Jhurani Aman Dua Jaipur Delhi Gurgaon Mumbai Ashish Singh Ashok Kumar Avtar Singh Adarsh Annapareddy Hyderabad Bihar Chennai Amristar Bharat Modi B D Chatterjee Deepak Thakur H P Bhalodia Vadodara Kolkata Delhi Ahmedabad Dhanasekara Raja Dimple Parekh Gurava Reddy A V Harish Ghoota Coimbatore Ahmedabad Hyderabad Faridabad Harshad Joshi Hemant Wakankar Indrajit Sardar Javahir A Pachore Pune Surat Kolkata -

ISHKS BROCHURE 2019.Pdf
President’s note Dear Friends The most eagerly awaited, exciting and educational annual event is only a few days away ! Prepare for an academic extravaganza with outstanding faculty, current topics, raging controversies, developing trends and future perspectives in Hip and Knee Arthroplasty. Interaction and adequate time for debate and discussion will ensure you return enriched with ideas and techniques to help you perform even better Arthroplasty. Hope you have registered and we are looking forward to welcoming you in Bengaluru ! President - ISHKS Organizing Chairman Co Organizing Chairman Arun Mullaji H P C Khincha Sharan Patil ISHKS EXECUTIVE BOARD 2018 - 2019 President Committee Chairs Members of Committee Arun Mullaji Research Vikram Shah 1st Vice President S. V. Vaidya Rajesh Maniar Hemant Wakankar Nominating Ashok Rajgopal 2nd Vice President B.D. Chatterjee Surya Bhan Gurava Reddy Fellowship S. V. Vaidya Somesh Singh 3rd Vice President Sharan Patil Education S. S. Mohanty Secretary Membership Leo Joseph N. RajKumar Treasurer Legal H. P. C. Khincha Ronen Roy Past Presidents FOUNDER MEMBERS Rajesh Maniar (2017 - 2018) J.A. Pachore (Mumbai) Shekhar Agarwal (2016 - 2017) Ashok Rajgopal (Delhi) Sanjay Agarwala (2015 - 2016) Vikram Shah (Ahmedabad) H.P. Bhalodia (2014 - 2015) Suryanarayan P. (Chennai) C.J. Thakkar (2013 - 2014) Arun Mullaji (Mumbai) S.V. Vaidya (2012 - 2013) S.K.S. Marya (Delhi) S. K. S. Marya (2011 - 2012) P. Suryanarayan (2010 - 2011) Rajesh Maniar (Mumbai) Vikram I. Shah (2009 - 2010) Sanjay Agarwala (Mumbai) Ashok Rajgopal (2008 - 2009) S.V.Vaidya (Mumbai) Javahir A. Pachore (2006 - 2008) Surya Bhan (Delhi) Harish Bhende (Mumbai) A.V.Gurava Reddy (Hyderabad) P. -

Nominations for Padma Awards 2011
c Nominations fof'P AWARDs 2011 ADMA ~ . - - , ' ",::i Sl. Name';' Field State No ShriIshwarappa,GurapJla Angadi Art Karnataka " Art-'Cinema-Costume Smt. Bhanu Rajopadhye Atharya Maharashtra 2. Designing " Art - Hindustani 3. Dr; (Smt.).Prabha Atre Maharashtra , " Classical Vocal Music 4. Shri Bhikari.Charan Bal Art - Vocal Music 0, nssa·' 5. Shri SamikBandyopadhyay Art - Theatre West Bengal " 6: Ms. Uttara Baokar ',' Art - Theatre , Maharashtra , 7. Smt. UshaBarle Art Chhattisgarh 8. Smt. Dipali Barthakur Art " Assam Shri Jahnu Barua Art - Cinema Assam 9. , ' , 10. Shri Neel PawanBaruah Art Assam Art- Cinema Ii. Ms. Mubarak Begum Rajasthan i", Playback Singing , , , 12. ShriBenoy Krishen Behl Art- Photography Delhi " ,'C 13. Ms. Ritu Beri , Art FashionDesigner Delhi 14. Shri.Madhur Bhandarkar Art - Cinema Maharashtra Art - Classical Dancer IS. Smt. Mangala Bhatt Andhra Pradesh Kathak Art - Classical Dancer 16. ShriRaghav Raj Bhatt Andhra Pradesh Kathak : Art - Indian Folk I 17., Smt. Basanti Bisht Uttarakhand Music Art - Painting and 18. Shri Sobha Brahma Assam Sculpture , Art - Instrumental 19. ShriV.S..K. Chakrapani Delhi, , Music- Violin , PanditDevabrata Chaudhuri alias Debu ' Art - Instrumental 20. , Delhi Chaudhri ,Music - Sitar 21. Ms. Priyanka Chopra Art _Cinema' Maharashtra 22. Ms. Neelam Mansingh Chowdhry Art_ Theatre Chandigarh , ' ,I 23. Shri Jogen Chowdhury Art- Painting \VesfBengal 24.' Smt. Prafulla Dahanukar Art ~ Painting Maharashtra ' . 25. Ms. Yashodhara Dalmia Art - Art History Delhi Art - ChhauDance 26. Shri Makar Dhwaj Darogha Jharkhand Seraikella style 27. Shri Jatin Das Art - Painting Delhi, 28. Shri ManoharDas " Art Chhattisgarh ' 29. , ShriRamesh Deo Art -'Cinema ,Maharashtra Art 'C Hindustani 30. Dr. Ashwini Raja Bhide Deshpande Maharashtra " classical vocalist " , 31. ShriDeva Art - Music Tamil Nadu Art- Manipuri Dance 32. -

Fortis Announces Increased EBIDTA for Q3FY08 by 103% V/S Q2FY08
Fortis Healthcare reports healthy Q3 and 9M FY17 results Group Consolidated revenues for Q3 up 10.4%, Operating EBITDA up 159.3% Group Consolidated revenues for 9MFY17 up 9.9%, Operating EBITDA up 74% Completes the acquisition of 51% economic interest in Fortis Hospotel Limited (FHTL) from RHT; witnesses a significant reduction in net BT costs – down 37% versus Q3FY16 and down 40% versus Q2FY17 Files Composite Scheme of Arrangement and Amalgamation (demerger of diagnostics business) with the National Company Law Tribunal, Chandigarh for approval Hospital Business revenues up 8.5% to Rs 917 Cr despite impact of demonetization; operating EBITDA rises 7.3x to Rs 60.1 Cr Hospital Business EBITDAC* for Q3FY17 at Rs 131.3 Cr, 14.3% margin and for 9MFY17 Rs 434.9 Cr, 15.5% margin Diagnostics business net revenues up 10.9% to Rs 188 Cr despite impact of demonetization; EBITDA margins at 19.9% for the quarter and 22.7% for 9MFY17 Gurugram, February 14, 2017: Fortis Healthcare Ltd. (Fortis), India’s leading healthcare delivery Company, today, announced its consolidated results for the quarter and nine-month period ended December 31, 2016 (Q3FY17 and 9MFY17). Group Consolidated Business (Q3FY17) o Revenues at Rs 1133.4 Cr for the quarter, up 10.4% versus Rs 1026.5 Cr in Q3FY16 o Consolidated EBITDAC at Rs 186.6 Cr, 16.5% margin versus 15.4% margin in Q3FY16 o Consolidated operating EBITDA at Rs 115.4 Cr, an increase of 159% over Q3FY16 o Consolidated PBT before forex and exceptional items at Rs 16 Cr versus a loss of Rs 26.7 Cr o Consolidated PATMI at Rs 442 Cr versus a loss of Rs 30.6 Cr; PATMI includes a one- time gain in Share in Associates. -

4. Dr Ashok Rajgopal.Cdr
Review Journal of Clinical Orthopaedics 2017 Jan-June;2(1):10-13 What is New in Total Knee Replacement Ashok Rajgopal1, Vivek Dahiya1 Abstract Total knee replacement is a Gold standard for treatment of arthritis of knees. It has stood the test of time and has delivered excellent results. With time the number of knee replacement are increasing and the age of patients are decreasing. Technological advances have kept pace with the newer designs which have helped deliver better results to the patients Keywords: Total knee replacement, new updates, technology Background adhere to the age old nuances of “Let it cellophane, and many other materials The knee is the largest joint of the be , you are getting old”. In the past two have been used, but results were human body and it is involved in almost decades the average age of the patients disappointing. The use of metallic all the activities of daily living. It is undergoing knee replacement surgery interposition arthroplasty began in the prone to repetitive micro trauma leading has come down resulting in an increased late 1930s. Today implants are made of a to wear and tear of the cartilage which in demand on the knee joint [3]. The highly polished cobalt chrome alloy turn leads to osteoarthritis of the knee challenges for the Orthopaedics surgeon which is a very strong alloy well joint. Osteoarthritis makes a knee stiff, are manifold. Not only does he need to tolerated and accepted by the human painful to walk on and inhibits an correct the deformity, and enable the body. -

Annexure 1B 18416
Annexure 1 B List of taxpayers allotted to State having turnover of more than or equal to 1.5 Crore Sl.No Taxpayers Name GSTIN 1 BROTHERS OF ST.GABRIEL EDUCATION SOCIETY 36AAAAB0175C1ZE 2 BALAJI BEEDI PRODUCERS PRODUCTIVE INDUSTRIAL COOPERATIVE SOCIETY LIMITED 36AAAAB7475M1ZC 3 CENTRAL POWER RESEARCH INSTITUTE 36AAAAC0268P1ZK 4 CO OPERATIVE ELECTRIC SUPPLY SOCIETY LTD 36AAAAC0346G1Z8 5 CENTRE FOR MATERIALS FOR ELECTRONIC TECHNOLOGY 36AAAAC0801E1ZK 6 CYBER SPAZIO OWNERS WELFARE ASSOCIATION 36AAAAC5706G1Z2 7 DHANALAXMI DHANYA VITHANA RAITHU PARASPARA SAHAKARA PARIMITHA SANGHAM 36AAAAD2220N1ZZ 8 DSRB ASSOCIATES 36AAAAD7272Q1Z7 9 D S R EDUCATIONAL SOCIETY 36AAAAD7497D1ZN 10 DIRECTOR SAINIK WELFARE 36AAAAD9115E1Z2 11 GIRIJAN PRIMARY COOPE MARKETING SOCIETY LIMITED ADILABAD 36AAAAG4299E1ZO 12 GIRIJAN PRIMARY CO OP MARKETING SOCIETY LTD UTNOOR 36AAAAG4426D1Z5 13 GIRIJANA PRIMARY CO-OPERATIVE MARKETING SOCIETY LIMITED VENKATAPURAM 36AAAAG5461E1ZY 14 GANGA HITECH CITY 2 SOCIETY 36AAAAG6290R1Z2 15 GSK - VISHWA (JV) 36AAAAG8669E1ZI 16 HASSAN CO OPERATIVE MILK PRODUCERS SOCIETIES UNION LTD 36AAAAH0229B1ZF 17 HCC SEW MEIL JOINT VENTURE 36AAAAH3286Q1Z5 18 INDIAN FARMERS FERTILISER COOPERATIVE LIMITED 36AAAAI0050M1ZW 19 INDU FORTUNE FIELDS GARDENIA APARTMENT OWNERS ASSOCIATION 36AAAAI4338L1ZJ 20 INDUR INTIDEEPAM MUTUAL AIDED CO-OP THRIFT/CREDIT SOC FEDERATION LIMITED 36AAAAI5080P1ZA 21 INSURANCE INFORMATION BUREAU OF INDIA 36AAAAI6771M1Z8 22 INSTITUTE OF DEFENCE SCIENTISTS AND TECHNOLOGISTS 36AAAAI7233A1Z6 23 KARNATAKA CO-OPERATIVE MILK PRODUCER\S FEDERATION -

Alphabetical List of Recommendations Received for Padma Awards - 2014
Alphabetical List of recommendations received for Padma Awards - 2014 Sl. No. Name Recommending Authority 1. Shri Manoj Tibrewal Aakash Shri Sriprakash Jaiswal, Minister of Coal, Govt. of India. 2. Dr. (Smt.) Durga Pathak Aarti 1.Dr. Raman Singh, Chief Minister, Govt. of Chhattisgarh. 2.Shri Madhusudan Yadav, MP, Lok Sabha. 3.Shri Motilal Vora, MP, Rajya Sabha. 4.Shri Nand Kumar Saay, MP, Rajya Sabha. 5.Shri Nirmal Kumar Richhariya, Raipur, Chhattisgarh. 6.Shri N.K. Richarya, Chhattisgarh. 3. Dr. Naheed Abidi Dr. Karan Singh, MP, Rajya Sabha & Padma Vibhushan awardee. 4. Dr. Thomas Abraham Shri Inder Singh, Chairman, Global Organization of People Indian Origin, USA. 5. Dr. Yash Pal Abrol Prof. M.S. Swaminathan, Padma Vibhushan awardee. 6. Shri S.K. Acharigi Self 7. Dr. Subrat Kumar Acharya Padma Award Committee. 8. Shri Achintya Kumar Acharya Self 9. Dr. Hariram Acharya Government of Rajasthan. 10. Guru Shashadhar Acharya Ministry of Culture, Govt. of India. 11. Shri Somnath Adhikary Self 12. Dr. Sunkara Venkata Adinarayana Rao Shri Ganta Srinivasa Rao, Minister for Infrastructure & Investments, Ports, Airporst & Natural Gas, Govt. of Andhra Pradesh. 13. Prof. S.H. Advani Dr. S.K. Rana, Consultant Cardiologist & Physician, Kolkata. 14. Shri Vikas Agarwal Self 15. Prof. Amar Agarwal Shri M. Anandan, MP, Lok Sabha. 16. Shri Apoorv Agarwal 1.Shri Praveen Singh Aron, MP, Lok Sabha. 2.Dr. Arun Kumar Saxena, MLA, Uttar Pradesh. 17. Shri Uttam Prakash Agarwal Dr. Deepak K. Tempe, Dean, Maulana Azad Medical College. 18. Dr. Shekhar Agarwal 1.Dr. Ashok Kumar Walia, Minister of Health & Family Welfare, Higher Education & TTE, Skill Mission/Labour, Irrigation & Floods Control, Govt. -

ORTHOPAEDIC SURGERY Ganga Hospital, Coimbatore, India
Department of ORTHOPAEDIC SURGERY Ganga Hospital, Coimbatore, India. Activity Report 2013 - 2014 The traditional symbol of orthopaedic Surgery, described by Nicolas Andry in 1741, is the bent tree that has been braced to make it grow upward and straight. Ganga Hospital 313 Mettupalayam Road, Coimbatore - 641 043, Tamilnadu, INDIA. Hospital : +91 422 2485000, 4250000, Appointment : +91 422 2485025, 2485026, Fax No +91 422 2451444 Email : [email protected], [email protected], Web : www.gangahospital.com Founders Mrs. Kanakavalli Shanmuganathan & Dr. J. G. Shanmuganathan Vision To showcase to the world the best in patient care, surgical expertise, academics, medical ethics and state-of-the art technology. Dr Ravindra Bhat To be a center which will be a pride of our country. 1993-2012 Mission To provide quality treatment at affordable cost so that the expertise Dr Ravindra Bhat headed the Department of Anaesthesia of Ganga Hospital from 1993-2012 and will be available to every citizen of our country. laid the foundation for trauma care in the hospital. His dedication and involvement in the care of severely injured left an everlasting impression to all those who have met him. He did pioneering work in the initial management of polytrauma victims, regional anaesthesia and nerve block and was a source of inspiration for the numerous fellows and trainees from all over the world. To perpetuate his memory, ' Ganga Hospital – Dr Ravindra Bhat Memorial Oration' has been initiated and will be delivered annually by an eminent medical personnel. To live in the hearts of those who love you is never to die... Dr. -
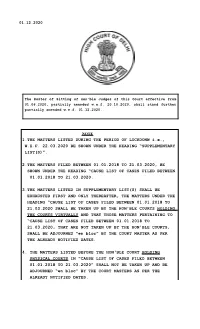
1.THE MATTERS LISTED DURING the PERIOD of LOCKDONW I.E., W.E.F
01.12.2020 The Roster of Sitting of Hon’ble Judges of this Court effective from 01.06.2020, partially amended w.e.f. 20.10.2020, shall stand further partially amended w.e.f. 01.12.2020. NOTE 1.THE MATTERS LISTED DURING THE PERIOD OF LOCKDONW i.e., W.E.F. 22.03.2020 BE SHOWN UNDER THE HEADING “SUPPLEMENTARY LIST(S)”. 2.THE MATTERS FILED BETWEEN 01.01.2018 TO 21.03.2020, BE SHOWN UNDER THE HEADING “CAUSE LIST OF CASES FILED BETWEEN 01.01.2018 TO 21.03.2020. 3.THE MATTERS LISTED IN SUPPLEMENTARY LIST(S) SHALL BE EXHAUSTED FIRST AND ONLY THEREAFTER, THE MATTERS UNDER THE HEADING “CAUSE LIST OF CASES FILED BETWEEN 01.01.2018 TO 21.03.2020 SHALL BE TAKEN UP BY THE HON'BLE COURTS HOLDING THE COURTS VIRTUALLY AND THAT THOSE MATTERS PERTAINING TO “CAUSE LIST OF CASES FILED BETWEEN 01.01.2018 TO 21.03.2020, THAT ARE NOT TAKEN UP BY THE HON'BLE COURTS, SHALL BE ADJOURNED “en bloc” BY THE COURT MASTER AS PER THE ALREADY NOTIFIED DATES. 4. THE MATTERS LISTED BEFORE THE HON'BLE COURT HOLDING PHYSICAL COURTS IN “CAUSE LIST OF CASES FILED BETWEEN 01.01.2018 TO 21.03.2020” SHALL NOT BE TAKEN UP AND BE ADJOURNED “en bloc” BY THE COURT MASTERS AS PER THE ALREADY NOTIFIED DATES. DELETION NOTE 1. CM(M) 603/2020 LISTED BEFORE HON'BLE MR. JUSTICE NAJMI WAZIRI AT ITEM NO 1 IS DELETED AS THE SAME IS LISTED BEFORE HON'BLE MR.