Triglyceride: One Molecule at the Center of Health and Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Blood Fats Explained
Blood Fats Explained HEART UK – The Cholesterol Charity providing expert support, education and influence 2 | Fats in the blood At risk of cardiovascular disease? | 3 Fats in the blood At risk of cardiovascular disease? Fats that circulate in the blood are called lipids. Very low density lipoproteins (VLDL) transport Cardiovascular disease (CVD) is the medical Blood pressure is a measure of the resistance Cholesterol and triglycerides are both lipids. mainly triglycerides made by the liver to where name for circulatory diseases such as coronary to the flow of blood around your body. It is They have essential roles in the body. In excess they are either used to fuel our muscles or stored heart disease (CHD), stroke, mini stroke (transient measured in millimetres of mercury (mmHg). Your they are harmful. for later use. ischaemic attack or TIA), angina and peripheral doctor or nurse will measure both your systolic vascular disease (PVD). You are more likely to (upper figure) and diastolic (lower figure) blood Cholesterol is needed to build cell walls and Low density lipoproteins (LDL) carry most of the develop CVD the more risk factors you have. pressure. About a third of adults have high blood to make hormones and vitamin D. Some of our cholesterol in our body from the liver to the cells pressure. If untreated it increases the risk of cholesterol comes from the food we eat; but most that need it. The cholesterol that is carried on LDLs There are two types of risk factors: heart attack and stroke. High blood pressure is is made in the liver. -

II. Phosphoglyceride Fatty Acids
Pediat. Res. 8: 93-102 (1974) Arachidonic acid ethanolamine phosphoglycerides brain lipids choline phosphoglycerides Some Chemical Aspects of Human Brain Development. II. Phosphoglyceride Fatty Acids MANUELAMARTINEZ, CARMEN CONDE, AND ANGELBALLABRIGA[~~~ Autonomous University, School of Medicine, Children's Hospital of the "Seguridad Social," Barcelona, Spain Extract The fatty acids of total phosphoglycerides (TPG), ethanolamine phosphoglycerides (EPG), and choline phosphoglycerides (CPG) were obtained by mild alkaline trans- methylation from lipid extracts of whole cerebrum and then analyzed by gas chroma- tography. A complete brain hemisphere from each of the 34 newborn infants reported previously was homogenized and its lipids extracted according to the procedure speci- fied in that report. As the gestational age of the children went up, a statistically significant increase of the n-3/n-6 ratio and, especially, of the 22:4(n-6)/22:5(n-6) index was observed. Other ratios, such as the n-6/n-9 and the 18:0/18: 1(n-9), were also studied in the fatty acid patterns of EPG and CPG. Both of them showed sig- nificant increases with the gestational age of the infants. The [22 :4(n-6) + 22 :5(n-6)]/ 20:4(n-6) index, an indicator of the elongation process of arachidonic acid, on the other hand, did not show appreciable changes with maturation in TPG during this period of life. When ethanolamine and choline phosphoglycerides were analyzed separately, however, the elongation of arachidonic acid did rise with the gestational age in the former whereas it decreased in the latter. As intrauterine maturation of the human brain progresses, changes in the polyun- saturated fatty acid patterns, contrary to those observed in undernourished animals, take place. -

Fats and Fatty Acid in Human Nutrition
ISSN 0254-4725 91 FAO Fats and fatty acids FOOD AND NUTRITION PAPER in human nutrition Report of an expert consultation 91 Fats and fatty acids in human nutrition − Report of an expert consultation Knowledge of the role of fatty acids in determining health and nutritional well-being has expanded dramatically in the past 15 years. In November 2008, an international consultation of experts was convened to consider recent scientific developments, particularly with respect to the role of fatty acids in neonatal and infant growth and development, health maintenance, the prevention of cardiovascular disease, diabetes, cancers and age-related functional decline. This report will be a useful reference for nutrition scientists, medical researchers, designers of public health interventions and food producers. ISBN 978-92-5-106733-8 ISSN 0254-4725 9 7 8 9 2 5 1 0 6 7 3 3 8 Food and Agriculture I1953E/1/11.10 Organization of FAO the United Nations FAO Fats and fatty acids FOOD AND NUTRITION in human nutrition PAPER Report of an expert consultation 91 10 − 14 November 2008 Geneva FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2010 The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. -
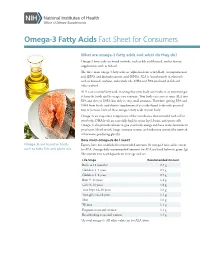
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Omega-6:Omega-3 Fatty Acid Ratio and Total Fat Content of the Maternal Diet Alter Offspring Growth and Fat Deposition in the Rat
nutrients Article Omega-6:Omega-3 Fatty Acid Ratio and Total Fat Content of the Maternal Diet Alter Offspring Growth and Fat Deposition in the Rat Sally A. V. Draycott 1,2,*, Matthew J. Elmes 1, Beverly S. Muhlhausler 2,3 and Simon Langley-Evans 1 1 Sutton Bonington Campus, School of Biosciences, University of Nottingham, Loughborough LE12 5RD, UK; [email protected] (M.J.E.); [email protected] (S.L.-E.) 2 Food and Nutrition Research Group, Department of Food and Wine Science, School of Agriculture, Food and Wine, University of Adelaide, Adelaide, SA 5064, Australia; [email protected] 3 Commonwealth Scientific and Industrial Research Organisation, Adelaide, SA 5000, Australia * Correspondence: [email protected] Received: 1 July 2020; Accepted: 13 August 2020; Published: 19 August 2020 Abstract: Omega-3 long-chain polyunsaturated fatty acids (LCPUFA) have been shown to inhibit lipogenesis and adipogenesis in adult rats. Their possible early life effects on offspring fat deposition, however, remain to be established. To investigate this, female Wistar rats (n = 6–9 per group) were fed either a 9:1 ratio of linoleic acid (LA) to alpha-linolenic acid (ALA) or a lower 1:1.5 ratio during pregnancy and lactation. Each ratio was fed at two total fat levels (18% vs. 36% fat w/w) and offspring were weaned onto standard laboratory chow. Offspring exposed to a 36% fat diet, irrespective of maternal dietary LA:ALA ratio, were lighter (male, 27 g lighter; female 19 g lighter; p < 0.0001) than those exposed to an 18% fat diet between 3 and 8 weeks of age. -

Omega-3, Omega-6 and Omega-9 Fatty Acids
Johnson and Bradford, J Glycomics Lipidomics 2014, 4:4 DOI: 0.4172/2153-0637.1000123 Journal of Glycomics & Lipidomics Review Article Open Access Omega-3, Omega-6 and Omega-9 Fatty Acids: Implications for Cardiovascular and Other Diseases Melissa Johnson1* and Chastity Bradford2 1College of Agriculture, Environment and Nutrition Sciences, Tuskegee University, Tuskegee, Alabama, USA 2Department of Biology, Tuskegee University, Tuskegee, Alabama, USA Abstract The relationship between diet and disease has long been established, with epidemiological and clinical evidence affirming the role of certain dietary fatty acid classes in disease pathogenesis. Within the same class, different fatty acids may exhibit beneficial or deleterious effects, with implications on disease progression or prevention. In conjunction with other fatty acids and lipids, the omega-3, -6 and -9 fatty acids make up the lipidome, and with the conversion and storage of excess carbohydrates into fats, transcendence of the glycome into the lipidome occurs. The essential omega-3 fatty acids are typically associated with initiating anti-inflammatory responses, while omega-6 fatty acids are associated with pro-inflammatory responses. Non-essential, omega-9 fatty acids serve as necessary components for other metabolic pathways, which may affect disease risk. These fatty acids which act as independent, yet synergistic lipid moieties that interact with other biomolecules within the cellular ecosystem epitomize the critical role of these fatty acids in homeostasis and overall health. This review focuses on the functional roles and potential mechanisms of omega-3, omega-6 and omega-9 fatty acids in regard to inflammation and disease pathogenesis. A particular emphasis is placed on cardiovascular disease, the leading cause of morbidity and mortality in the United States. -

2015 National Lipid Association
Journal of Clinical Lipidology (2015) -, -–- Original Contribution National Lipid Association Recommendations for Patient-Centered Management of Dyslipidemia: Part 1—Full Report Terry A. Jacobson, MD*, Matthew K. Ito, PharmD, Kevin C. Maki, PhD, Carl E. Orringer, MD, Harold E. Bays, MD, Peter H. Jones, MD, James M. McKenney, PharmD, Scott M. Grundy, MD, PhD, Edward A. Gill, MD, Robert A. Wild, MD, PhD, Don P. Wilson, MD, W. Virgil Brown, MD Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA (Dr Jacobson); Oregon State University/Oregon Health & Science University, College of Pharmacy, Portland, OR, USA (Dr Ito); Midwest Center for Metabolic & Cardiovascular Research and DePaul University, Chicago, IL, USA (Dr Maki); University of Miami Health System, Miami, FL, USA (Dr Orringer); Louisville Metabolic and Atherosclerosis Research Center, Louisville, KY, USA (Dr Bays); Baylor College of Medicine, Houston, TX, USA (Dr Jones); Virginia Commonwealth University and National Clinical Research, Richmond, VA, USA (Dr McKenney); The University of Texas Southwestern Medical Center, Dallas, TX, USA (Dr Grundy); University of Washington/Harborview Medical Center, Seattle, WA, USA (Dr Gill); Oklahoma University Health Sciences Center, Oklahoma City, OK, USA (Dr Wild); Cook Children’s Medical Center, Fort Worth, TX, USA (Dr Wilson); and Emory University School of Medicine, Atlanta, GA, USA (Dr Brown) KEYWORDS: Abstract: The leadership of the National Lipid Association convened an Expert Panel to develop a Clinical consensus set of recommendations for patient-centered management of dyslipidemia in clinical med- recommendations; icine. An Executive Summary of those recommendations was previously published. This document Dyslipidemia; provides support for the recommendations outlined in the Executive Summary. -

Utilization of Glycerol-C'4 for Intestinal Glyceride Esterifi- Cation: Studies in a Patient with Chyluria * PETER R
Journal of Clinical Investigation Vol. 43, No. 3, 1964 Utilization of Glycerol-C'4 for Intestinal Glyceride Esterifi- cation: Studies in a Patient with Chyluria * PETER R. HOLT (Fromz the Gastroinitestinial Research Laboratory anid Medical Service, St. Luike's Hospital, New York, N. Y.) Ingested long chain triglycerides are hydrolyzed quantitative estimation of the incorporation of the to partial glycerides and free fatty acids in the in- exogenous labeled glycerol into intestinal lymiplh testinal lumen, but the extent of intraluminal hy- lipids. drolysis is still in dispute (2). After digestion Materials and Methods and absorption into the intestinal mucosa, re-esteri- fication of the fatty acids is necessary before in- Cliniical features. The subject, a 63-year-old Puerto corporation into chylomicra, which pass into the Rican male, was admitted to St. Luke's Hospital with a 30-year history of chyluria. Complete clinical data on intestinal lymphatics. Favarger and Gerlach this patient have been published (10). Lymphography originally considered that mucosal esterification of revealed tortuous dilated intra-abdominal lymphatics fatty acids occurred by a mechanism that was a with communications from the cisterna chyli and para- reversal of lipolysis (3). Subsequent studies in- aortic lymph glands to the left kidney and bladder (10). dicated that a more complex system of synthesis Cystoscopy showed a fistula in the region of the bladder neck. was involved (4). In addition, glycerol, liberated Before these studies the patient had been maintained onl within the intestinal lumen by hydrolysis, was not formula feedings, and while ingesting only long chain believed to be a substrate for glyceride-glycerol fats (C16 to C18 triglycerides), excreted in the urine fat synthesis, for when C14-labeled glycerol and free amounting to 3.5 to 14% (mean, 8.5%) of the daily fat fatty acids or triglycerides were fed to rats, little intake. -

Insulin Regulates Hepatic Triglyceride Secretion and Lipid Content Via Signaling in the Brain
Diabetes Page 2 of 37 Insulin regulates hepatic triglyceride secretion and lipid content via signaling in the brain Short Title: Brain insulin regulates hepatic VLDL secretion Thomas Scherer1,2,5, Claudia Lindtner1, James O’Hare1, Martina Hackl2, Elizabeth Zielinski1, Angelika Freudenthaler2, Sabina Baumgartner-Parzer2, Klaus Tödter3, Joerg Heeren3, Martin Krššák2,4, Ludger Scheja3, Clemens Fürnsinn2 & Christoph Buettner1,5 1Department of Medicine and Department of Neuroscience, Diabetes, Obesity and Metabolism Institute, Icahn School of Medicine at Mount Sinai, One Gustave L. Levy Place, New York, NY 10029, USA 2Department of Medicine III, Division of Endocrinology and Metabolism, Medical University of Vienna, Waehringer Guertel 18-20, 1090 Vienna, Austria 3Department of Biochemistry and Molecular Cell Biology, University Medical Center Hamburg-Eppendorf, 20246 Hamburg, Germany 4High Field MR Centre, Department of Biomedical Imaging and Image Guided Therapy, Medical University of Vienna, Waehringer Guertel 18-20, 1090 Vienna, Austria 5To whom correspondence should be addressed. E–mail: [email protected] or [email protected] T.S.: Phone: +43 1 40400 47850; Fax: +43 1 40400 77900 C.B.: Phone: +1 212 241 3425; Fax: +1 212 241 4218 Key words: brain; insulin; triglyceride secretion; hepatic lipid content Word count: 3998 Figures: 4 1 Diabetes Publish Ahead of Print, published online February 9, 2016 Page 3 of 37 Diabetes Non-standard abbreviations ARC: arcuate nucleus; CNS: central nervous system; CSF: cerebrospinal -

A Novel Omega‐3 Glyceride Mixture Enhances Enrichment Of
A novel omega‐3 glyceride mixture enhances enrichment of eicosapentaenoic acid and docosahexaenoic acid after single dosing in healthy older adults: results from a double‐ blind crossover trial Helena L. Fisk1,2,*, Grete Mørk Kindberg3, Svein Olaf Hustvedt3, and Philip C Calder1,2 1School of Human Development and Health, Faculty of Medicine, University of Southampton, Southampton SO16 6YD, United Kingdom; 2NIHR Southampton Biomedical Research Centre, University Hospital Southampton NHS Foundation Trust and University of Southampton, Southampton SO16 6YD, United Kingdom; 3BASF Norge AS, 0283 Oslo, Norway. *Author for correspondence: School of Human Development and Health, Faculty of Medicine, University of Southampton, IDS Building, MP887 Southampton General Hospital, Tremona Road, Southampton SO16 6YD, United Kingdom Running heading: Enrichment of EPA and DHA after single dosing List of abbreviations: ω‐3, omega‐3; ALA, alpha‐linoleic acid; BMI, body mass index; Cmax, maximal concentration; DHA, docosahexaenoic acid; DPA, docosapentaenoic acid; EE, ethyl‐ester(s); EPA, eicosapentaenoic acid; FA, fatty acid(s); FAME, fatty acid methyl esters; FFA, free fatty acid(s); Glyceride formulation, mix of mono, di and triglycerides; HDL, high density lipoprotein; HOMA2‐IR, homeostatic model assessment of insulin resistance; hsCRP, high sensitivity C‐reactive protein; iAUC, incremental area under the curve; ω‐3 LCPUFA, omega‐3 long chain polyunsaturated fatty acid(s); SMEDS, self‐micro‐emulsifying delivery system; TG, triglyceride(s); Tmax,, time at which maximal concentration occurs. 1 1 Abstract 2 A glyceride mix of mono, di, and triglycerides increases solubilisation and enhances emulsification of 3 omega‐3 (ω‐3) fatty acid (FA) containing lipids in the stomach. This allows for better access of 4 digestive enzymes, pivotal for the release of bioactive ω‐3 FA. -

Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases
International Journal of Molecular Sciences Review Omega-3 Versus Omega-6 Polyunsaturated Fatty Acids in the Prevention and Treatment of Inflammatory Skin Diseases Anamaria Bali´c 1 , Domagoj Vlaši´c 2, Kristina Žužul 3, Branka Marinovi´c 1 and Zrinka Bukvi´cMokos 1,* 1 Department of Dermatology and Venereology, University Hospital Centre Zagreb, School of Medicine University of Zagreb, Šalata 4, 10 000 Zagreb, Croatia; [email protected] (A.B.); [email protected] (B.M.) 2 Department of Ophtalmology and Optometry, General Hospital Dubrovnik, Ulica dr. Roka Mišeti´ca2, 20000 Dubrovnik, Croatia; [email protected] 3 School of Medicine, University of Zagreb, Šalata 3, 10000 Zagreb, Croatia; [email protected] * Correspondence: [email protected] Received: 31 December 2019; Accepted: 21 January 2020; Published: 23 January 2020 Abstract: Omega-3 (!-3) and omega-6 (!-6) polyunsaturated fatty acids (PUFAs) are nowadays desirable components of oils with special dietary and functional properties. Their therapeutic and health-promoting effects have already been established in various chronic inflammatory and autoimmune diseases through various mechanisms, including modifications in cell membrane lipid composition, gene expression, cellular metabolism, and signal transduction. The application of !-3 and !-6 PUFAs in most common skin diseases has been examined in numerous studies, but their results and conclusions were mostly opposing and inconclusive. It seems that combined !-6, gamma-linolenic acid (GLA), and -

Propane-1,2-Diyl Diacetate Using Immobilized Lipase B from Candida Antarctica and Pyridinium Chlorochromate As an Oxidizing Agent
International Journal of Molecular Sciences Article Chemoenzymatic Synthesis of the New 3-((2,3-Diacetoxypropanoyl)oxy)propane-1,2-diyl Diacetate Using Immobilized Lipase B from Candida antarctica and Pyridinium Chlorochromate as an Oxidizing Agent Esteban Plata 1,Mónica Ruiz 1, Jennifer Ruiz 1, Claudia Ortiz 2, John J. Castillo 1,* and Roberto Fernández-Lafuente 3,* 1 Escuela de Química, Grupo de investigación en Bioquímica y Microbiología (GIBIM), Edificio Camilo Torres 210, Universidad Industrial de Santander, CEP, 680001 Bucaramanga, Colombia; [email protected] (E.P.); [email protected] (M.R.); [email protected] (J.R.) 2 Escuela de Microbiología, Universidad Industrial de Santander, 680001 Bucaramanga, Colombia; [email protected] 3 ICP-CSIC, Campus UAM-CSIC, Cantoblanco, 28049 Madrid, Spain * Correspondence: [email protected] (J.J.C.); rfl@icp.csic.es (R.F.-L.); Tel.:+57-320-902-6464 (J.J.C.); +34915854804 (R.F.-L.) Received: 3 August 2020; Accepted: 4 September 2020; Published: 5 September 2020 Abstract: To exploit the hydrolytic activity and high selectivity of immobilized lipase B from Candida antarctica on octyl agarose (CALB-OC) in the hydrolysis of triacetin and also to produce new value-added compounds from glycerol, this work describes a chemoenzymatic methodology for the synthesis of the new dimeric glycerol ester 3-((2,3-diacetoxypropanoyl)oxy)propane-1,2-diyl diacetate. According to this approach, triacetin was regioselectively hydrolyzed to 1,2-diacetin with CALB-OC. The diglyceride product was subsequently oxidized with pyridinium chlorochromate (PCC) and a dimeric ester was isolated as the only product. It was found that the medium acidity during the PCC treatment and a high 1,2-diacetin concentration favored the formation of the ester.