Highlights from Year Two of the CCG's Strategic Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2017 City of York Biodiversity Action Plan
CITY OF YORK Local Biodiversity Action Plan 2017 City of York Local Biodiversity Action Plan - Executive Summary What is biodiversity and why is it important? Biodiversity is the variety of all species of plant and animal life on earth, and the places in which they live. Biodiversity has its own intrinsic value but is also provides us with a wide range of essential goods and services such as such as food, fresh water and clean air, natural flood and climate regulation and pollination of crops, but also less obvious services such as benefits to our health and wellbeing and providing a sense of place. We are experiencing global declines in biodiversity, and the goods and services which it provides are consistently undervalued. Efforts to protect and enhance biodiversity need to be significantly increased. The Biodiversity of the City of York The City of York area is a special place not only for its history, buildings and archaeology but also for its wildlife. York Minister is an 800 year old jewel in the historical crown of the city, but we also have our natural gems as well. York supports species and habitats which are of national, regional and local conservation importance including the endangered Tansy Beetle which until 2014 was known only to occur along stretches of the River Ouse around York and Selby; ancient flood meadows of which c.9-10% of the national resource occurs in York; populations of Otters and Water Voles on the River Ouse, River Foss and their tributaries; the country’s most northerly example of extensive lowland heath at Strensall Common; and internationally important populations of wetland birds in the Lower Derwent Valley. -

North Yorkshire Joint Strategic Needs Assessment 2019 Vale of York CCG Profile
January 2019 North Yorkshire Joint Strategic Needs Assessment 2019 Vale of York CCG Profile Introduction This profile provides an overview of population health needs in Vale of York CCG (VoY CCG). Greater detail on particular topics can be found in our Joint Strategic Needs Assessment (JSNA) resource at www.datanorthyorkshire.org. This document is structured into five parts: population, deprivation, disease prevalence, hospital admissions and mortality. It identifies the major themes which affect health in VoY CCG and presents the latest available data, so the dates vary between indicators. Summary Life expectancy is higher than England. For 2011-2015, female life expectancy in VoY CCG is 83.6 years (England: 83.1), and male life expectancy is more than three years lower than for females at 80 years (England: 79.4) [1]. There is a high proportion of older people. In 2017, 19.6% of the population was aged 65 and over (68,900), higher than national average (17.3%). Furthermore over 9,100 (2.6%) were age 85+, compared with 2.3% in England. [2] Some children grow up in relative poverty. In 2015, there were 11.2% of children aged 0-15 years living in low income families, compared with 19.9% in England [1]. There are areas of deprivation. Within the CCG area, 7 Lower Super Output Areas (LSOAs) out of a total of 206 are amongst the 20% most deprived in England, and one these LSOAs is amongst the 10% most deprived in England. This is in Selby West ward in Selby District. [3] Many people have longstanding health problems. -

Big Changes to Nhs Commissioning in North Yorkshire
FREE ANNUAL REPORTER Summary of our achievements during 2019-20 Don’t miss BIG CHANGES TO NHS out: stay in ‘The Loop’ COMMISSIONING IN THE Loop is a virtual engagement network of patients, carers and the wider public with interests in NORTH YORKSHIRE health services funded by NHS North Yorkshire CCG. If you live in North HREE North Yorkshire clinical Yorkshire or if you are a commissioning groups (CCGs) have patient registered at a been disestablished and a new GP practice in North entity created. NHS Hambleton, Yorkshire, you can T sign-up. It’s free to join Richmondshire and Whitby CCG, NHS Harrogate and Rural District CCG and NHS and you get first-hand Scarborough and Ryedale CCG were information about the replaced by NHS North Yorkshire CCG on 1 work of the CCG and April 2020. We welcome NHS England’s developments to health decision and the benefits it will bring to the services across North people of North Yorkshire. As a single Yorkshire. organisation we can: We currently have Eliminate unnecessary duplication and almost 300 Loop bureaucratic boundaries to work more members and we want to efficiently together and with our partners deliver for local people. A single leadership continue to expand our Ensure consistency of decision making team was appointed in 2018, following network so that we can for the people of North Yorkshire decisions by each CCG’s governing body. listen to the views of Develop a unified approach to Charles Parker, GP and Chair of NHS people from the different relationships with the new North North Yorkshire CCG said the new communities we cover. -
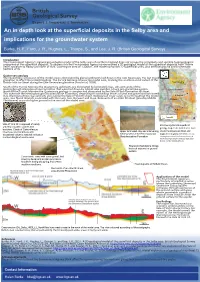
An in Depth Look at the Superficial Deposits in the Selby Area And
Expert | Impartial | Innovative An in depth look at the superficial deposits in the Selby area and implications for the groundwater system Burke, H. F., Ford, J. R., Hughes, L., Thorpe, S., and Lee, J. R. (British Geological Survey) Introducon The Environment Agency’s regional groundwater model of the Selby area of northern England does not convey the complexity and variable hydrogeological properes of the superficial deposits. To address this the Environment Agency commissioned a 3D geological model of the superficial deposits from Thorne near Doncaster to Haxby just north of York. Covering an area of 1,300km2, the model comprises 22 superficial units, plus arficial ground and 6 schemac bedrock units. Quaternary geology The Quaternary succession of the model area is dominated by glacial sediments laid down in the Late Devensian, the last major glaciaon to affect the United Kingdom. The Escrick Moraine crosses the model area, marking the southern-most extent of the Brish-Irish Ice Sheet during the Late Devensian glaciaon (Ford et al, 2008). York Moraine South of the Escrick Moraine the Quaternary sediments are dominated by laminated clays, silts and sands of the Hemingbrough Glaciolacustrine Formaon that were laid down by Glacial Lake Humber, a huge pro-glacial lake system. Escrick Moraine North of the Escrick Moraine the Quaternary geology is complex and dominated by the Vale of York Formaon ll sheet. This overrode the Hemingbrough Glaciolacustrine Formaon, deposing ll containing lenses of sand and gravel and laminated clay. Glaciolacustrine clays and silts also overlie the Vale of York ll sheet. Widespread cover sands occur throughout the model R Derwent area, plus fluvial deposits associated with the rivers Aire, Derwent and Ouse. -

Bring Me Sunshine’ Living Well with Dementia in North Yorkshire
Living Well With Dementia in North Yorkshire ‘Bring Me Sunshine’ Living Well With Dementia in North Yorkshire Signatories to the Living Well Contents with Dementia Strategy: Foreword . 4 Who are ‘we’? . 4 Purpose and scope of the North Yorkshire vision for dementia support . .5 What’s the Picture? . 6 Young Onset Dementia . 6 People with Learning disabilities . 7 Living with dementia and other health conditions . .8 Prevention . 8 Financial Impact - the national picture . 9 What else do we know? . 10 National Strategies . 10 Local Strategies . 12 Primary Care . 13 Secondary (hospital) Care . 14 York Teaching Hospitals - Craven District Council - Representing Mental Health Trusts representing acute hospital providers representing District Council members Overview of activity by area . 16 Mental Health Services . 18 How services are currently set up . 18 Care and Support . 20 Residential and Nursing Quality . 20 Achievements . 21 Accommodation . 23 Pathway . 24 End of Life Care and Support . 25 What matters most to people living with dementia - Consultation and engagement across North Yorkshire . 25 Key themes . 25 Delivering the strategy - action plan . 32 Moving Ahead . 34 Age UK - representing Selby District Council - the voluntary sector representing District Council officers 2 Published: 2017 3 ‘Bring Me Sunshine’ Living Well With Dementia in North Yorkshire Foreword Purpose and scope of the North Welcome to the North Yorkshire Dementia Strategy - ‘Bring Me Sunshine’ . Yorkshire vision for dementia support This strategy brings together organisations awareness of dementia will make a huge This strategy brings together the experiences well known information about people living from across Health and Social Care and the difference to the lives of many people across of those of us living with dementia and our with young onset dementia and people living Voluntary Sector to speak with one voice on North Yorkshire . -

Humber, Coast and Vale Integrated Care System (ICS) Information Pack June 2021
Humber, Coast and Vale Integrated Care System (ICS) Information Pack June 2021 NHS England and NHS Improvement Overview and Contents This information pack: - Gives a basic overview of the Integrated Care System (ICS); - Lists the Clinical Commissioning Groups (CCGs), Local Authorities (LAs) and NHS Trusts that operate in the ICS; - Provides basic maps of the ICS’s CCG and LA areas and boundaries; - Gives an overview of the wider North East and Yorkshire region and its 4 ICSs. CONTENTS PAGE CCG Area Information 3 Maps 4 CCG and Local Authority Information 5 NHS Trust Information 6 North East and Yorkshire Regional Information 7-13 ABBREVIATIONS NORTH EAST AND YORKSHIRE ICSs ICS Integrated Care System HCV Humber, Coast and Vale CCG Clinical Commissioning Group WY West Yorkshire LA Local Authority SYB South Yorkshire and Bassetlaw PCN Primary Care Network NENC North East and North Cumbria Please Note: All best efforts have been made to ensure the accuracy of the information contained within this pack at the time of its creation. Humber, Coast and Vale ICS CCG Area Information PRIMARY CARE CLINICAL COMMISSIONING GROUP POPULATION NETWORKS LOCAL AUTHORITIES * NHS TRUSTS AMBULANCE SERVICE (PCNs) Hull University Teaching Hospitals NHS Trust Humber Teaching NHS Foundation Trust East Riding of Yorkshire CCG 341,173 7 East Riding of Yorkshire Council Northern Lincolnshire and Goole NHS Foundation Trust York and Scarborough Teaching Hospitals NHS Foundation Trust Hull University Teaching Hospitals NHS Trust Hull CCG 259,778 5 Hull City Council Humber -

Windsor Chairs from the Vale of York. Adam Bowett
WINDSOR CHAIRS FROM THE VALE OF YORK Adam Bowett i. Outline map of the Vale of York. The Windsor chairs discussed in this essay are found predominantly within the area enclosed by the line York-Harrogate- Bedale-Northallerton - York. The published literature on Windsor chairs made in Yorkshire portrays them as a nineteenth-century phenomenon, developing out of the northward migration of High Wycombe chairmaking after 1800.1 The typology of Yorkshire Windsors constructed by Ivan Sparkes, Bernard Cotton and others has established clear stylistic and technical links between Windsor chairs made in the workshops of the South and West Ridings and the East Midlands manufactory based around Worksop and Retford, which itself was founded by Wycombe-trained chair-makers settling in Nottinghamshire at the beginning of the nineteenth century. Within a few decades chairmakers in the industrial areas of south and west Yorkshire had achieved a formidable output, and had established an identifiable Yorkshire style. The ‘standard’ Yorkshire Windsor is typified by the work of the Low Cringles workshop, near Keighley, which was published by Christopher Gilbert in 1995.2 But while these chairs have characteristics peculiar to Yorkshire, there is no disputing their debt to Nottinghamshire and, by extension, to High Wycombe. They are undoubtedly a manifestation of ‘regional’ chair-making, but they cannot be said to be ‘vernacular’ in the true sense of the word. Regional Furniture Volume XVIII 2004 2 WINDSOR CHAIRS FROM THE VALE OF YORK 2. Chair, late eighteenth century. Ash and oak spindles with sycamore seat. Original dark green paint beneath several subsequent finishes. -

Anglo-Saxon Settlements and Archaeological Visibility in the Yorkshire Wolds
This is a repository copy of Anglo-Saxon settlements and archaeological visibility in the Yorkshire Wolds. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/1172/ Book Section: Richards, J.D. orcid.org/0000-0003-3938-899X (2000) Anglo-Saxon settlements and archaeological visibility in the Yorkshire Wolds. In: Geake, H. and Kenny, J., (eds.) Early Deira: Archaeological studies of the East Riding in the fourth to ninth centuries AD. Oxbow Books , Oxford, UK , pp. 27-39. Reuse Items deposited in White Rose Research Online are protected by copyright, with all rights reserved unless indicated otherwise. They may be downloaded and/or printed for private study, or other acts as permitted by national copyright laws. The publisher or other rights holders may allow further reproduction and re-use of the full text version. This is indicated by the licence information on the White Rose Research Online record for the item. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ Anglo-Saxon Settlements and Archaeological Visibility -in the Yorkshre Wolds Julian D. Richards Summary in dispersed farms and villages. The thin chalk soils are largely given over to arable farming, although both cows Rural Anglo-Saxon settlements in the hinterland of York and sheep are also grazed on the uplands. There are are notoriously invisible. As a result of major urban rescue market towns at Malton and Driffield, lying off the chalk archaeology campaigns in the 1970s, more could be to the north-west and south-east respectively, but the inferred about Anglo-Saxon Yorkshire from finds in York nearest major urban centre is the city of York, which lies than from rural sites. -

NHS Vale of York CCG
CVD: Primary Care Intelligence Packs NHS Vale of York CCG June 2017 Version 1 Contents 1. Introduction 3 2. CVD prevention • The narrative 11 • The data 13 3. Hypertension • The narrative 16 • The data 17 4. Stroke • The narrative 27 • The data 28 5. Diabetes • The narrative 42 • The data 43 6. Kidney • The narrative 53 • The data 54 7. Heart • The narrative 65 • The data 66 8. Outcomes 82 9. Appendix 88 This document is valid only when viewed via the internet. If it is printed into hard copy or saved to another location, you must first check that the version number on your copy matches that of the one online. Printed copies are uncontrolled copies. 2 CVD: Primary Care Intelligence Packs Introduction 3 CVD: Primary Care Intelligence Packs This intelligence pack has been compiled by GPs and nurses and pharmacists in the Primary Care CVD Leadership Forum in collaboration with the National Cardiovascular Intelligence Network Matt Kearney Sarit Ghosh Kathryn Griffith George Kassianos Jo Whitmore Matthew Fay Chris Harris Jan Procter-King Yassir Javaid Ivan Benett Ruth Chambers Ahmet Fuat Mike Kirby Peter Green Kamlesh Khunti Helen Williams Quincy Chuhka Sheila McCorkindale Nigel Rowell Ali Morgan Stephen Kirk Sally Christie Clare Hawley Paul Wright Bruce Taylor Mike Knapton John Robson Richard Mendelsohn Chris Arden David Fitzmaurice 4 CVD: Primary Care Intelligence Packs Local intelligence as a tool for clinicians and commissioners to improve outcomes for our patients Why should we use this CVD Intelligence Pack The high risk conditions for cardiovascular disease (CVD) - such as hypertension, atrial fibrillation, high cholesterol, diabetes, non-diabetic hyperglycaemia and chronic kidney disease - are the low hanging fruit for prevention in the NHS because in each case late diagnosis and suboptimal treatment is common and there is substantial variation. -

NHS Vale of York Covid-19 and Vaccination Update
Involve – NHS Vale of York covid-19 and vaccination update Join the conversation - how you can help us Throughout the roll out of the vaccination we have a number of key messages that we need your helping in spreading through social media, networks, websites, newsletters and more. We have attached to this email a number of messages that you can use through your channels of communication - any help would be very much appreciated. Update on the roll out of the COVID vaccination The NHS is currently offering the COVID-19 vaccine to people most at risk from coronavirus. There is no need for patients to get in touch with their GP surgery – their surgery will contact individuals when it’s their turn. The vaccine is being offered in some hospitals and increasing numbers of local vaccination centres in North Yorkshire and York run by GP surgeries. The jab is currently being rolled out to all those aged 80 and over, along with frontline health and care workers and care home residents. People aged 75 and over and then all those who are 70 and over, together with clinically extremely vulnerable patients will follow. Read more. NHS Vale of York’s Clinical Chair and GP in Selby, Dr Nigel Wells, talks about why it’s important to wait to be contacted about your COVID vaccine in the short video below More people to get vaccinated in York as City site extended to become large-scale NHS Vaccination Centre The NHS COVID-19 vaccination programme is stepping up in York with Askham Bar Park and Ride now one of the first NHS Vaccination Centres, offering additional vaccinations to people from across the region. -

Strategic Flood Risk Assessment Revision 2 (March 2013)
YORK CITY OF YORK Strategic Flood Risk Assessment Revision 2 (March 2013) City of York Council Strategic Flood Risk Assessment Revision 2: March 2013 City of York Council Strategic Flood Risk Assessment Integrated Strategy Unit: Flood Risk Management Revision 2 : March 2013 Contents GLOSSARY ............................................................................................................................... 5 ABBREVIATIONS ...................................................................................................................... 7 EXECUTIVE SUMMARY ........................................................................................................... 8 1 INTRODUCTION .............................................................................................................. 13 1.1 Background ................................................................................................................... 13 1.2 Purpose of the Assessment .......................................................................................... 14 1.3 Contents ........................................................................................................................ 14 2 BACKGROUND ................................................................................................................ 16 2.1 River Network ............................................................................................................... 16 2.2 Broad Physical Characteristics .................................................................................... -
The Vertebrates of the River Foss: an Historical
The vertebrates of the River Foss: an historical review Burbot, from Rev William Houghton’s British Fresh-water Fishes, Volume 2 (1879) A report for the River Foss Society Martin Hammond [email protected] December 2017 1. INTRODUCTION This report was commissioned by the River Foss Society to review historic wildlife data associated with the river. It is one of three similar reports, the others covering flora and invertebrates. A wide range of literature has been searched, including the publications of the Yorkshire Naturalists’ Union (e.g. The Naturalist and Transactions of the Yorkshire Naturalists’ Union), synopses of the fauna of the York area (e.g. Grabham, 1906, 1907a & b) and papers relating to key species. The unpublished record books of the now-defunct York & District Field Naturalists’ Society (YDFNS) have also been consulted. Fisheries data was requested from the Environment Agency but only two sets of results from electro-fishing surveys were made available. Some general information was also provided by City of York Council. 2. MAMMALS The mammal species most closely associated with the River Foss are Water Vole and Otter. A number of other mammals will be more loosely associated with the river corridor, riparian habitats being important for foraging bats, for example. Water Vole Records from the archives suggest that Water Vole populations in the Vale of York increased greatly during the early 20th century but underwent phases of decline thereafter, with an accelerating reduction towards the end of the century. In 1911, it was noted in the YDFNS record book that, “Water Voles are rapidly becoming ubiquitous, most of the little becks with which the Vale of York is so plentifully supplied providing asylum for innumerable colonies of these interesting and prolific rodents”.