S41598-021-83654-7.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Landscape Analysis of Geographical Names in Hubei Province, China
Entropy 2014, 16, 6313-6337; doi:10.3390/e16126313 OPEN ACCESS entropy ISSN 1099-4300 www.mdpi.com/journal/entropy Article Landscape Analysis of Geographical Names in Hubei Province, China Xixi Chen 1, Tao Hu 1, Fu Ren 1,2,*, Deng Chen 1, Lan Li 1 and Nan Gao 1 1 School of Resource and Environment Science, Wuhan University, Luoyu Road 129, Wuhan 430079, China; E-Mails: [email protected] (X.C.); [email protected] (T.H.); [email protected] (D.C.); [email protected] (L.L.); [email protected] (N.G.) 2 Key Laboratory of Geographical Information System, Ministry of Education, Wuhan University, Luoyu Road 129, Wuhan 430079, China * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel: +86-27-87664557; Fax: +86-27-68778893. External Editor: Hwa-Lung Yu Received: 20 July 2014; in revised form: 31 October 2014 / Accepted: 26 November 2014 / Published: 1 December 2014 Abstract: Hubei Province is the hub of communications in central China, which directly determines its strategic position in the country’s development. Additionally, Hubei Province is well-known for its diverse landforms, including mountains, hills, mounds and plains. This area is called “The Province of Thousand Lakes” due to the abundance of water resources. Geographical names are exclusive names given to physical or anthropogenic geographic entities at specific spatial locations and are important signs by which humans understand natural and human activities. In this study, geographic information systems (GIS) technology is adopted to establish a geodatabase of geographical names with particular characteristics in Hubei Province and extract certain geomorphologic and environmental factors. -

Download Article
Advances in Economics, Business and Management Research, volume 70 International Conference on Economy, Management and Entrepreneurship(ICOEME 2018) Research on the Path of Deep Fusion and Integration Development of Wuhan and Ezhou Lijiang Zhao Chengxiu Teng School of Public Administration School of Public Administration Zhongnan University of Economics and Law Zhongnan University of Economics and Law Wuhan, China 430073 Wuhan, China 430073 Abstract—The integration development of Wuhan and urban integration of Wuhan and Hubei, rely on and Ezhou is a strategic task in Hubei Province. It is of great undertake Wuhan. Ezhou City takes the initiative to revise significance to enhance the primacy of provincial capital, form the overall urban and rural plan. Ezhou’s transportation a new pattern of productivity allocation, drive the development infrastructure is connected to the traffic artery of Wuhan in of provincial economy and upgrade the competitiveness of an all-around and three-dimensional way. At present, there provincial-level administrative regions. This paper discusses are 3 interconnected expressways including Shanghai- the path of deep integration development of Wuhan and Ezhou Chengdu expressway, Wuhan-Ezhou expressway and from the aspects of history, geography, politics and economy, Wugang expressway. In terms of market access, Wuhan East and puts forward some suggestions on relevant management Lake Development Zone and Ezhou Gedian Development principles and policies. Zone try out market access cooperation, and enterprises Keywords—urban regional cooperation; integration registered in Ezhou can be named with “Wuhan”. development; path III. THE SPACE FOR IMPROVEMENT IN THE INTEGRATION I. INTRODUCTION DEVELOPMENT OF WUHAN AND EZHOU Exploring the path of leapfrog development in inland The degree of integration development of Wuhan and areas is a common issue for the vast areas (that is to say, 500 Ezhou is lower than that of central urban area of Wuhan, and kilometers from the coastline) of China’s hinterland. -
Present Status, Driving Forces and Pattern Optimization of Territory in Hubei Province, China Tingke Wu, Man Yuan
World Academy of Science, Engineering and Technology International Journal of Environmental and Ecological Engineering Vol:13, No:5, 2019 Present Status, Driving Forces and Pattern Optimization of Territory in Hubei Province, China Tingke Wu, Man Yuan market failure [4]. In fact, spatial planning system of China is Abstract—“National Territorial Planning (2016-2030)” was not perfect. It is a crucial problem that land resources have been issued by the State Council of China in 2017. As an important unordered and decentralized developed and overexploited so initiative of putting it into effect, territorial planning at provincial level that ecological space and agricultural space are seriously makes overall arrangement of territorial development, resources and squeezed. In this regard, territorial planning makes crucial environment protection, comprehensive renovation and security system construction. Hubei province, as the pivot of the “Rise of attempt to realize the "Multi-Plan Integration" mode and Central China” national strategy, is now confronted with great contributes to spatial planning system reform. It is also opportunities and challenges in territorial development, protection, conducive to improving land use regulation and enhancing and renovation. Territorial spatial pattern experiences long time territorial spatial governance ability. evolution, influenced by multiple internal and external driving forces. Territorial spatial pattern is the result of land use conversion It is not clear what are the main causes of its formation and what are for a long period. Land use change, as the significant effective ways of optimizing it. By analyzing land use data in 2016, this paper reveals present status of territory in Hubei. Combined with manifestation of human activities’ impact on natural economic and social data and construction information, driving forces ecosystems, has always been a specific field of global climate of territorial spatial pattern are then analyzed. -
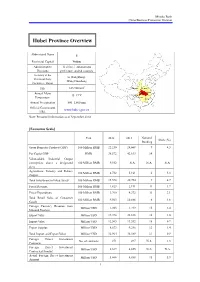
Hubei Province Overview
Mizuho Bank China Business Promotion Division Hubei Province Overview Abbreviated Name E Provincial Capital Wuhan Administrative 12 cities, 1 autonomous Divisions prefecture, and 64 counties Secretary of the Li Hongzhong; Provincial Party Wang Guosheng Committee; Mayor 2 Size 185,900 km Shaanxi Henan Annual Mean Hubei Anhui 15–17°C Chongqing Temperature Hunan Jiangxi Annual Precipitation 800–1,600 mm Official Government www.hubei.gov.cn URL Note: Personnel information as of September 2014 [Economic Scale] Unit 2012 2013 National Share (%) Ranking Gross Domestic Product (GDP) 100 Million RMB 22,250 24,668 9 4.3 Per Capita GDP RMB 38,572 42,613 14 - Value-added Industrial Output (enterprises above a designated 100 Million RMB 9,552 N.A. N.A. N.A. size) Agriculture, Forestry and Fishery 100 Million RMB 4,732 5,161 6 5.3 Output Total Investment in Fixed Assets 100 Million RMB 15,578 20,754 9 4.7 Fiscal Revenue 100 Million RMB 1,823 2,191 11 1.7 Fiscal Expenditure 100 Million RMB 3,760 4,372 11 3.1 Total Retail Sales of Consumer 100 Million RMB 9,563 10,886 6 4.6 Goods Foreign Currency Revenue from Million USD 1,203 1,219 15 2.4 Inbound Tourism Export Value Million USD 19,398 22,838 16 1.0 Import Value Million USD 12,565 13,552 18 0.7 Export Surplus Million USD 6,833 9,286 12 1.4 Total Import and Export Value Million USD 31,964 36,389 17 0.9 Foreign Direct Investment No. -

Retrospect: the Outbreak Evaluation of COVID-19 in Wuhan District of China
healthcare Article Retrospect: The Outbreak Evaluation of COVID-19 in Wuhan District of China Yimin Zhou 1,2,*,† , Zuguo Chen 1,3,† , Xiangdong Wu 1,2 , Zengwu Tian 1,2, Lingjian Ye 1,2 and Leyi Zheng 1,2 1 Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, 1068 Xueyuan Avenue, Xili University Town, Shenzhen 518055, China; [email protected] (Z.C.); [email protected] (X.W.); [email protected] (Z.T.); [email protected] (L.Y.); [email protected] (L.Z.) 2 School of Computer Science and Technology, The University of Chinese Academy of Sciences, Beijing 100049, China 3 School of Information and Electrical Engineering, Hunan University of Science and Technology, Xiangtan 411201, China * Correspondence: [email protected] † The first two authors contributed equally. Abstract: There were 27 novel coronavirus pneumonia cases found in Wuhan, China in December 2019, named as 2019-nCoV temporarily and COVID-19 formally by the World Health Organization (WHO) on the 11 February 2020. In December 2019 and January 2020, COVID-19 has spread on a large scale among the population, which brought terrible disaster to the life and property of the Chinese people. In this paper, we analyze the features and pattern of the virus transmission. Considering the influence of indirect transmission, a conscious-based Susceptible-Exposed-Infective-Recovered (SEIR) (C-SEIR) model is proposed, and the difference equation is used to establish the model. We simulated the C-SEIR model and key important parameters. The results show that (1) increasing people’s awareness of the virus can effectively reduce the spread of the virus; (2) as the capability and possibility of indirect infection increases, the proportion of people being infected will also increase; (3) the increased cure rate can effectively reduce the number of infected people. -

Hubei Xiangyang Integrated Sustainable Transportation and Logistics Planning and Strategic Study
Technical Assistance Consultant’s Report Project Number: 51029-001 June 2020 People’s Republic of China: Hubei Xiangyang Integrated Sustainable Transportation and Logistics Planning and Strategic Study Prepared by: David Lupton & Associates Ltd. For the Asian Development Bank and Xiangyang Municipal Transport Bureau This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. TA-9547 PRC: Hubei Xiangyang Comprehensive Transportation and Logistics Planning and Strategic Study- 01 (51029-001) Supplementary Report June 2020 Prepared for: the Asian Development Bank and Xiangyang Municipal Transport Bureau David Lupton & Associates Ltd. TA-9547 PRC: Hubei Xiangyang Comprehensive Transportation and Logistics Planning and Strategic Study- 01 (51029-001) CURRENCY EQUIVALENT (as of 10 January 2019) Currency unit: USD USD1=7.08 CNY 1 CNY=USD 0.14 WEIGHTS AND MEASURES km2 – square kilometre m3 cubic meter mu: 15 mu=1 hectare NOTES (i) In this Report, “$” refers to US Dollars (ii) The fiscal year (FY) of the Government and its agencies ends on 31 December. FY before a calendar year denotes the year in which the fiscal year ends, e.g., FY2018 ends on 31 December 2018. (iii) At the 17 January 2019 meeting between the client the XMTB, ADB and the consultant, the client requested that the title for the Project be changed to “Hubei Xiangyang Comprehensive Transportation and Logistics Planning and Strategic Study” in order to reflect the new Han River Economic Development Plan Consultants Quality Assurance Protocol Prepared By Robert L. Wallack, David J. -

Effect of Public Health Interventions on COVID-19 Cases
Respiratory epidemiology Original research Thorax: first published as 10.1136/thoraxjnl-2020-215086 on 16 February 2021. Downloaded from Effect of public health interventions on COVID-19 cases: an observational study Weihong Qiu,1,2 Heng He,3 Peng Zhang,4 Wenwen Yang,4 Tingming Shi,5 Xing Wang,1,2 Ailian Chen,1,2 Li Xie,1,2 Meng Yang,1,2 Dongming Wang,1,2 Mingyan Li,4 Weihong Chen 1,2 ► Additional material is ABSTRACT published online only. To view Background As the epidemic of COVID-19 is gradually Key messages please visit the journal online (http:// dx. doi. org/ 10. 1136/ controlled in China, a summary of epidemiological thoraxjnl-2020- 215086). characteristics and interventions may help control its global What is the key question? spread. ► Since the outbreak, the full spectrum of the For numbered affiliations see Methods Data for COVID-19 cases in Hubei Province outbreak and the impact of non- pharmaceutical end of article. (capital, Wuhan) was extracted until 7 March 2020. interventions on COVID-19 in Hubei Province The spatiotemporal distribution of the epidemic in are still unclear. Correspondence to four periods (before 10 January, 10–22 January, 23 Professor Weihong Chen, What is the bottom line? January–6 February and 7 February–7 March) was Department of Occupational ► We analysed the effects of non- pharmaceutical and Environmental Health, evaluated, and the impacts of interventions were intervention measures, including district traffic School of Public Health, Tongji observed. interruption, wearing masks in public places Medical College, Huazhong Results Among 67 706 COVID-19 cases, 52 111 University of Science and and isolating infected patients and close (76.97%) were aged 30–69 years old, and 34 680 Technology, Wuhan, Hubei, contacts, on stopping the epidemic in Wuhan (51.22%) were women. -

Short-Term Outcomes of COVID-19 and Risk Factors for Progression
AGORA | | RESEARCH LETTER Short-term outcomes of COVID-19 and risk factors for progression To the Editor: Coronavirus disease 2019 (COVID-19) has now become a worldwide health concern. The severity of COVID-19 has been classified as mild, moderate, severe and critical [1]. To date, there have been a few studies focused on the clinical course and outcome of critical cases [2–4]. However, information regarding outcomes of mild-to-moderate cases is lacking, despite the fact that mild-to-moderate cases have accounted for approximately 80% of laboratory-confirmed patients [1, 5]. This study aimed to investigate short-term outcomes of patients rated with different severities on admission, and to identify risk factors for progression, thereby helping the management of COVID-19 in clinical practice. All consecutive patients with laboratory-confirmed COVID-19 admitted to The First People’s Hospital of Jingzhou and to Xiangyang Central Hospital (tertiary hospitals located in Jingzhou City and Xiangyang City, Hubei Province, China) between 16 January and 24 February 2020 were unselectively enrolled. Diagnosis of COVID-19 was made according to the Diagnosis and Treatment Program for COVID-19 (Trial Version 5), released by China’s National Health Commission [6], and complied with World Health Organization interim guidance [7]. Mild cases were defined when patients only presented with mild symptoms and did not have a radiographic appearance of pneumonia. Moderate cases were defined when patients presented with fever and/or respiratory symptoms and had a radiographic appearance of pneumonia. Severe cases were defined when patients presented with one of the following: 1) respiratory − distress with respiratory rate ⩾30 breaths·min 1; 2) finger oxygen saturation ⩽93% at resting state; 3) arterial oxygen tension/inspiratory oxygen fraction ⩽300 mmHg. -

A Brief Evolutionary History of TCM Culture in Hubei— from the Pre
2017 3rd Annual International Conference on Modern Education and Social Science (MESS 2017) ISBN: 978-1-60595-450-9 A Brief Evolutionary History of TCM Culture in Hubei— From the Pre-Qin Period to the Qing Dynasty Ming-An HUANG1,a, He-Rong MAO2,b*, Hui WEN3,c and Chong WEN4,d 1Center for TCM Development and Research, Hubei University of TCM, No. 1, West Huang Jiahu Road, Hongshan District, Wuhan City, Hubei Province, 430065, PRC. 2*Center for Compilation and Translation of TCM Literature, School of Foreign Languages, Hubei University of TCM, No. 1, West Huang Jiahu Road, Hongshan District, Wuhan City, Hubei Province, 430065, PRC. 3Department of Finance/Center for Military Medicine, Academy of Military Economics, No.122, Luo Jiadun, Qiaokou District, Wuhan City, Hubei Province, 430035, PRC. 4Department of TCM Rehabilitation, the Central Hospital of Wuhan, No. 26, Shengli Street, Jiang’an District, Wuhan City, Hubei Province, 430014, PRC. [email protected],[email protected]* [email protected],[email protected] *He-Rong MAO, Center for Compilation and Translation of TCM Literature, School of Foreign Languages, Hubei University of TCM, No. 1, West Huang Jiahu Road, Hongshan District, Wuhan City, Hubei Province, 430065, PRC. Telephone: +86-13986187098, E-mail: [email protected] Keywords: Evolutionary History, TCM Culture, Hubei Abstract: This paper tries to analyze the rules of evolution and development of TCM culture in Hubei in history. By exploring the rich materials from the authentic history books and local annals and interpreting the great medical thoughts of representative TCM masters lived in Hubei, we find that TCM culture has been well inherited and carried forward in Hubei and Hubei enjoys a respected position in the holistic development of TCM culture in China. -

Store Name:Microsoft Authorized Store Store ID: AR57 Contact Name
Store Name:Microsoft Authorized Store Store ID: AR57 Contact Name: Li Zuochao Phone: 18971682221 Address: Shop No# SJ2, first floor, gongmao hanggang road, wuhan city, Hu Bei Province Postal Code: 430022 Store Name:Kiosk - Wuhan New Netcom Wuhan Yifangcheng Store Store ID: AR61 Contact Name: Liao Qin Phone: 15997493703 Address: Microsoft store, 4th floor, shopping center, 1 square, 1515 zhongshan avenue, jiang an district, Wuhan, Hu Bei Province Postal Code: 430014 Store Name:Microsoft Authorized Store Store ID: AR78 Contact Name: Xiao Mangling Phone: 13636150166 Address: Microsoft store, 1st floor, huayuecheng plaza, 29 chaoyang middle road, MaoJian District, shiyan city, Hubei province Postal Code: 442000 Store Name: Microsoft Authorized Store Store ID: AR79 Contact Name: Qiu Wenjie Phone: 18071124426 Address: 5th floor, Wuhan New Netcom International Plaza, Hanjiang District, Wuhan, Hubei Province. Postal Code: 430022 Store Name:Microsoft Authorized Store Store ID: AR80 Contact Name: Lu Dudu Phone: 18971503732 Address: 5th floor, Wushang square, No#. 688 Jiefang avenue, Hankou, Wuhan Province Postal Code: 430022 Store Name:Microsoft Authorized Store Store ID: AR96 Contact Name: Yang Ming Phone: 18627871210 Address: B1 Guanggu industrial and trade appliances (carrefour downstairs) of Guanggu Walking Street, Hongshan District, Wuhan, Hubei province. Postal Code: 430070 Store Name:Microsoft Experience Center Store ID: SIS25 Contact Name: Wen Ranhao Phone: 18607154911 Address: Suning e-buy Microsoft, Zhongshan Plaza, 557 Jiefang Avenue, -

Wudang Mountain (Famous for Martial Arts) Shennongjia (A Place of Primitive Forest), Etc
Welcome to China! Welcome to Hubei! Welcome to Wuhan! Part I. About Hubei Province Part II.About Wuhan City I.Brief Introduction II.Hubei Food III.Hubei Celebrities IV.Hubei Attractions V.Hubei Customs I. Brief Introduction Basic Facts E (鄂)for short the Province of a Thousand Lakes---千湖之省 provincial capital---Wuhan Hometown of the first ancestor of the Chinese nation,the emperor Yan( Shennong) Rich in agriculture, fishery ,forestry and hydropower resources. Main industries : iron and steel, machinery, power and automobile. Historic interest and scenic beauty the Three Gorges of the Yangtze River the East Lake and the Yellow Crane Tower in Wuhan the Temple of Emperor Yan in Suizhou the Hometown of Quyuan in Zigui Wudang Mountain (famous for martial arts) Shennongjia (a place of primitive forest), etc. Geography 186,000 square kilometers. Population : 60,700,000 HUBEI---the north of the Dongting Lake. High in the west and low in the east and wide open to the south, the Jianghan Plain. North--- Henan South---Jiangxi &Hunan East --- Anhui West ---Sichuan Northwest ---Shaanxi Climate Hubei has a sub-tropical monsoonal climate, with a mean annual temperature of 15oC- 17oC -- the hottest month, July, averaging 27- 30oC and the coldest month, January, 1-5oC -- and a mean annual precipitation of 800-1600 mm. Administrative Division and Population 1 autonomous prefecture: Enshi Tujiazu 12 prefecture-level cities: Wuhan, Huangshi, Shiyan, Jingzhou, Yichang, Xiangfan, Ezhou, Jingmen, Xiaogan, Huanggang, Xianning, Suizhou 24 county-level cities 39 counties 2 autonomous counties 1 forest district: Shennongjia ethnic groups :Han, Tu, Miao, Hui, Dong, Manchu, Zhuang, and Mongolian. -

Huaxin Cement Co., Ltd. Announcement on Providing Guarantee for Bank Loans of Some Subsidiaries
Stock Codes: 600801, 900933 Stock Abbreviations: Huaxin Cement, Huaxin B Share Ref: 2020-014 Huaxin Cement Co., Ltd. Announcement on Providing Guarantee for Bank Loans of Some Subsidiaries To the best of our knowledge, the Board of Directors of the Company and its members confirm that there is no material false or misleading statement or material omission in this announcement and shall be severally and jointly liable for the truthfulness, accuracy and completeness of its content. Important Content: Guaranteed companies: Huaxin Cement (Yangxin) Ltd. and other 55 wholly owned subsidiaries and controlling subsidiaries. Guarantee amount provided by the Company for Huaxin Cement (Yangxin) Ltd. and other 55 wholly owned subsidiaries and controlling subsidiaries is 5.419 billion RMB. By the end of 2019, the Company’s actual guarantee balance for the 56 wholly owned subsidiaries and controlling subsidiaries was 1.79 billion RMB. Counter guarantee: nil Overdue guarantee: nil I. General Information of the Guarantees On April 27, 2020, the Sixteenth Meeting of the Ninth Board of Directors of Huaxin Cement Co., Ltd. (hereinafter referred to as “the Company”) reviewed and adopted the Proposal in Respect of Providing Guarantee for Bank Loans of Some Subsidiaries. By December 31, 2019, guarantee reviewed by the Board of Directors for wholly owned subsidiaries, controlling subsidiaries and related party companies totalled at 7.065 billion RMB within the valid duration. Affected by periodical financing environment and subjective reasons of some subsidiaries, the actual utilized guarantee amount is 1,442.8234 million RMB and 49.74 million USD, accounting for 10.7% of the latest audited net assets and 25% of the approved total guarantee amount.