Department of Nutrition and Dietetics a Guide on Lowering Your Salt Intake
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

$25 Per Person Plus Tax & Service
24 Hour Notice Required on All Orders American Artisan Charcuterie Local Salami, Pepperoni, Speck, Bresaola, Green Olives, Artichokes, Cherry Peppers, Tomatoes, and Roasted Red Peppers Served with Ale Mustard & Sliced Breads *Fresh Fruit Display Seasonal Fresh Fruits artistically arranged *Garden Vegetable Display Assorted Seasonal Vegetables Served with Basil Pesto Aioli and Buttermilk-Parsley Dressing Domestic Cheese Display Sonoma Goat Cheese, Pepper Jack, White Cheddar, Gorgonzola and Brie Served with House Spiced Nuts, Dried Fruits, and Sliced Breads $25 per person Plus Tax & Service Fee Garden Vegetable Display Assorted Seasonal Vegetables Served with Basil Pesto Aioli and Buttermilk-Parsley Dressing Gourmet Cheese Spreads Your Choice of the Following Flavors: Herb & Roasted Garlic Boursin with Italian Parsley Pimento Cheese Goat Cheese, Basil Pesto and Sun-Dried Tomatoes Served with Sliced Breads Grilled & Chilled Beef Tenderloins with Sweet Pepper Piccalilli Chicken and Sun Dried Tomato Sausage in Puff Pastry Cured Salmon in Cucumber Cubes with Saffron Aioli Tarpy’s Mini Meatloaves Caramelized Onion, Thyme and Gruyere Flatbread $40 per person Plus Tax & Service Fee American Artisan Charcuterie Local Salami, Pepperoni, Speck, Bresaola, Green Olives, Artichokes, Cherry Peppers, Tomatoes, and Roasted Red Peppers Served with Ale Mustard & Sliced Breads Antipasto Display Display of Grilled Marinated Vegetables, Vegetable Giardiniera, Olives, Roasted Peppers, Wood Fired Portabella Mushrooms, Marinated Mozzarella and Genoa Salami Served -

Hot Sandwiches Cold Sandwiches
Scrumptious Sandwiches ~All sandwiches served with coleslaw and house salad~ Hot Sandwiches Cold Sandwiches Served on a choice of White or Brown Toasted Bloomer Served on a choice of White or Brown Bloomer Proper Fish Finger Butty - £8.75 Glazed Ham & Piccalilli - £7.75 Prosecco Battered Cod Goujons & Tartare Sauce Roast Sirloin of Beef & Horseradish - £7.75 “Yorky” Cheese Steak Sandwich - £10.75 Grilled Yorkshire Sirloin with melting Yorkshire Blue Cheese Black Bomber Cheddar & Chutney - £7.25 (V) Smokey Bacon BLT - £9.50 Bacon, Lettuce, Tomato & Dijon Mayonnaise Smoked Salmon & Cream Cheese - £8.25 Halloumi Grill - £9.50 Black Truffle Egg Mayonnaise - £7.75 (V) Grilled Halloumi, Pesto, Baby Gem Hand-Cut Chunky Chips £3.75 Black Truffle Mash £3.75 Onion Rings £3.75 Nibble Bowls Marinated Olives £3.75 Black Truffle Mayonnaise £2.00 Farrier Salad £3.75 Large Plates Small Plates ~Served with Vegetables & Potatoes where appropriate~ The ‘Stable’ Soup of the Day - £6.50 (GO) (V) Cider Braised Pork Collar - £16.50 Served with a Crispy Bread Roll Apple Puree, Apple Crumble, Crackling, Braised Gravy Hickory Smoked Chicken Breast - £9.50 (GF) Spinach & Ricotta Tortellini - £16.25 (V) Farrier Style Greek Salad, Foraged Herb Dressing Piquant Tomato Sauce, Wild Garlic Dressing, Parmesan Whitby Smokehouse Fishcake - £8.50 Prosecco Battered Whitby Cod - £15.50 Hand Cut Tartare Sauce, Charred Citrus, Herb Salad Hand Cut Chips, Buttered Garden Peas, Tartar Sauce & Charred Lemon Smooth Liver & Cognac Pate - £8.50 Toasted Brioche & Apple Chutney Grilled -

British Food
BRITISH FOOD GROCERY ITEM PRODUCT DESCRIPTION CTN SIZE BATCHELORS PEAS CANS 0740 MUSHY PEAS ORIGINAL 24x300g 0741 MUSHY PEAS CHIP SHOP 24x300g 0743 BIGGA PEAS 24x300g 0745 FARROWS MARROWFAT 24x300g 0744 SMALL PEAS 24x300g FORESIGHT 0843 PEASE PUDDING 6x410g HOMEPRIDE COOK-IN-SAUCE CANS 0823 WHITE WINE 12x500g 0824 RED WINE 12x500g 0825 CURRY 12x500g 0829 CHASSEUR 12x500g 0830 SWEET & SOUR 12x500g 0831 CHILLI 12x500g HEINZ - JARS 0925 PLOUGHMANS PICKLE 8x280g 0926 MILD MUSTARD PICKLE 8x280g 0927 TANGY SANDWICH PICKLE 8x280g 0928 TANGY TOMATO PICKLE 8x280g 0929 PICCALILLI PICKLE 8x280g 0930 PICKLED ONIONS 6x440g 0931 SILVERSKIN ONIONS 6x440g 0933 BABY BEETROOT 6x440g 0934 CRINKLE CUT BEETROOT 6x440g 0935 RED CABBAGE 6x440g 0939 SALAD CREAM 12x285g ITEM PRODUCT DESCRIPTION CTN SIZE 0940 SANDWICH SPREAD 12x270g 0937 TOMATO SOUP 24x400g 0942 BAKED BEANS 4 PACK 6x4PK 6x4x415g 0920 MINI JAR MAYONNAISE 80x30g 0921 MINI JAR COARSE GRAIN MUSTARD 80x39g 0922 MINI JAR TOMATO KETCHUP 80x39g GOLDENFRY 0961 GRAVY GRANULES SMALL 6x170g 0958 YORKSHIRE PUDDING MIX 12x142g PKT 0959 DUMPLING MIX 12x142g PKT 0960 GRAVY GRANULES LARGE 6x300g PAXO 0994 SAGE & ONION STUFFING 16x170g PKT WEETABIX UK 0790 WHOLEWHEAT BISCUITS 14x430g 0791 ALPEN ORIGINAL MUESLI 10x625g 0792 ALPEN NO ADDED SUGAR 10x560g Page 1 of 10 PRINCES 0452 HERRING IN TOMATO SAUCE 10x200g 0454 PILCHARDS IN TOMATO SAUCE SMALL 12x155g 0455 PILCHARDS IN TOMATO SAUCE LARGE 12x425g 0456 PRESSED CODS ROE SMALL 12x200g 0457 PRESSED CODS ROE LARGE 6x600g 0458 SOFT CODS ROE 10x100g SHIPPAMS 0465 CRAB -

Pickles and Pickling
No 106 BULLETIN 1930-31 OF THE AGRICULTURAL EXTENSION SERVICE, THE OHIO STATE UNIVERSITY H. C RAMSOWER, Director Pickles and Pickling By Lelia C. Ogle Extension Specialist in Nutrition The Ohio State University THE OHIO STATE UNIVER$I'l'Y, COLUMBUS, OHIO, ANP THE UNITEP STATES DEPART~ OF Alll\ICULTURE 000P!llll4.TING AGRICtTUl'UltAL EXTENSION SERVICE-H. c. RAMSOWER, D1:ree:tm: FREE-Cooperative Agricultural Extensfon Work-Acts of 111sY 8 and June 30, 1914 PICKLES AND PICKLING By LELIA C. OGLE Specia!Jst in Nutrition The Ohio State University Fruits and vegetables preserved with salt, vinegar, or both, and with or without the addition of sugar and spices, constitute what is commonly called pickles. The discussion in this bulletin will be confined to the principles of pickling as they apply especially to cucumber pickles, in an effort to answer some of the many questions on the process and its difficulties. Cucumbers may be preserved by means of (1) fermentation as the result of the action of the bacteria on the sugar of the veg etables; (2) the addition of acid, usually vinegar; or (3) addition of a very strong brine. Any of these methods prevent bacterial growth if all other conditions are right. The secret of making pickles by the fermentation process lies in bringing about acid fermentation quickly, and after this is done, in preserving the acidity of the brine by covering tightly or sealing to exclude air. It is the acid formed by the action of bacteria on the sugar of the vegetables that cures and keeps the vegetables, if all air is excluded and scum yeast has not been allowed to develop. -

Table of Contents Breakfast
TABLE OF CONTENTS BREAKFAST................................................................................................................................................................. 2 HOT AND COLD ...................................................................................................................................................... 2 PACKAGES .............................................................................................................................................................. 3 MORNING/AFTERNOON TEA OPTIONS ..................................................................................................................... 4 SWEET AND SAVOURY OPTIONS ........................................................................................................................... 4 GLUTEN FREE ......................................................................................................................................................... 5 WHOLE CAKES ........................................................................................................................................................ 6 HIGH TEA................................................................................................................................................................ 6 LUNCH OPTIONS ........................................................................................................................................................ 7 BREAD AND RICE PAPER ....................................................................................................................................... -

Autumn Piccalilli with Pear
Autumn piccalilli with pear Eaten immediately, this pickle will have a punchy tang, perfect with strong cheeses, but by winter the flavours will mellow, ideal for sliced ham. • 2 small cauliflower , cut into small florets • 400g silverskin or pearl onions • 600g courgettes , cut into small chunks (about 2cm pieces) • 6 firm pears , cored, and cut as the courgettes • 100g salt • 1.7l cider vinegar • finger-length piece fresh root ginger , grated • 2 tbsp coriander seeds • 3 tbsp brown or black mustard seeds • 300g golden caster sugar • 8 tbsp cornflour • 5 tbsp English mustard powder • 3 tsp turmeric 1. In a bowl, mix together the vegetables, pears and salt with 2 litres of cold water, then cover and leave overnight. 2. The next day, drain the brine from the vegetables, rinse briefly, then tip into a large saucepan with the vinegar, ginger, coriander seeds, mustard seeds and sugar. Bring to the boil and simmer for 8-10 mins until the veg is just tender but still with a little bite. Drain the vegetables, reserving the liquid, and set aside while you make the sweet mustard sauce. 3. In a large bowl, stir together the cornflour, mustard powder and turmeric, then gradually pour in the hot vinegar while whisking, until you have a lump-free, thin yellow sauce. Return it to the saucepan and bubble over a low heat, stirring constantly, for 4 mins until smooth and thickened. Stir in the veg and spoon into five sterilised 500ml jars while hot, then seal. Once cool, enjoy straight away, or store in a cool, dark cupboard for 2-3 months. -

Pickles & Relishes
Food Preservation… Pickles & Relishes, Lesson 6 UNIVERSITYUNIVERSITY OF OF ALASKA ALASKA FAIRBANKSFAIRBANKS FNH-00562F Pickles & Relishes Pickles are one of the favorites of home can- ners, and pickling is among the oldest known methods of preserving food, dating back to Biblical times. Today, pickles are great for snacks and are the perfect companion for sandwiches. When we speak of pickles, many of us think only of cucumbers. But in canning terms, pickles include any fruit, meat or vegetable prepared by a pickling process, as well as a wide variety of relishes. Pickle products are either fermented in brine (salt) or packed in vinegar to aid preservation. Many older recipes called for pickles to be weeks. Dilled cucumbers and sauerkraut be- packed into jars and sealed without processing. long to this group. Herbs and spices are often This method is no longer recommended. There added to the solution for flavoring. is always a danger of harmful microorganisms entering the food when it is transferred from Fresh-pack pickles—Quick-process pickles pickling container to jar. canned in a spicy vinegar solution without brining, but usually soaked for several hours Processing destroys organisms that can cause or overnight. spoilage and inactivates enzymes that may af- fect flavor, color and texture. Relishes—Prepared from fruits and/or veg- etables that are chopped and cooked to desired Pickle products are generally grouped into consistency in a spicy vinegar solution. If a four classes: sweet relish is desired, sugar can be added. Hot peppers or other spices make a hot relish. Brined pickles—Also called fermented pick- les. -

Making Traditional and Modern Chutneys, Pickles and Relishes: a Comprehensive Guide Pdf
FREE MAKING TRADITIONAL AND MODERN CHUTNEYS, PICKLES AND RELISHES: A COMPREHENSIVE GUIDE PDF Jeremy Hobson,Philip Watts | 128 pages | 26 Jul 2010 | The Crowood Press Ltd | 9781847971920 | English | Ramsbury, United Kingdom Chutney recipes - BBC Good Food Please sign in to Making Traditional and Modern Chutneys a review. If you have changed your email address then contact us and we will update your details. Would you like to proceed to the App store to download the Waterstones App? We have recently updated our Privacy Policy. The site uses cookies to offer you a better experience. By continuing to browse the site you accept our Cookie Policy, you can change your settings at any time. Temporarily unavailable Currently unavailable to order. Email me when available Stay one step ahead and let us notify you when this item is next available Making Traditional and Modern Chutneys order. Notify me. Thank you We Making Traditional and Modern Chutneys contact you when this item is next available to order. Chutneys, pickles and relishes are important forms of preserved food that can bring life and richness to any meal, be it a simple lunch or an exotic dinner. Commercially, they form a multi-million pound industry and ever-imaginative Pickles and Relishes: A Comprehensive Guide examples appear on the supermarket shelves with great regularity. Moreover, pickles, chutneys and relishes are often a favourite with shoppers at farmer's markets and country fairs. Notwithstanding this, there is absolutely no reason why, with very little effort, and often the most basic of locally sourced ingredients, you should not make your own. -

Sides Large Small Terrine Board Snacks
LUNCH SMALL PUFFER’S PETITE OYSTERS 6 for 20 DILL PICKLE JUICE CHICKPEA PUREE 13 SNACKS KAMUT CRISPBREAD, WILTED SPRING ONION & LIGURIAN OLIVE OIL HERBED CAESAR SALAD 15 CARAMEL POPCORN ANCHOVY CROUTONS 5 MARKET CHOP SALAD 15 SEA SALT RADISHES, SQUASH, WAX BEANS, FETA & SUNFLOWER SEEDS & PEPPER CRISPS 5 HEIRLOOM TOMATO & BOILED FARM EGG 16 TONNATO SAUCE & GRILLED BREAD SPICED ALMONDS BROCCOLI RABE QUICHE 15 5 FONTINA, MARJORAM & FIELD GREENS SEAFOOD SAUSAGE 19 SCOTCH EGG BEURRE BLANC & CHIVES 9 BLOOD SAUSAGE 16 SCRUMPETS FRIED DUCK EGG & CREAMY TARRAGON VINAIGRETTE MINT VINEGAR 9 COTECHINO 15 SPICED BAKED BEANS & PARSLEY SHALLOT SALAD BOILED PEANUTS FRIED IN PORK FAT LARGE 7 CHICKEN LIVER PARFAIT CHARGRILLED LAMB BURGER 23 9 FETA, CUMIN MAYO & THRICE COOKED CHIPS OVEN BAKED 3 CHEESE SANDWICH 16 ONION MARMALADE & MUSTARD ROASTED MUSHROOM SANDWICH 16 ON MICHE BREAD WITH TALLEGGIO, RADICCHIO & GIARDINIERA SLOW COOKED SQUASH FRITTATA 17 BASIL, SAVORY, & MITICREMA BEER BATTERED LONG ISLAND FLUKE 23 TERRINE BOARD THRICE COOKED CHIPS & TARTAR SAUCE 34 CHARGRILLED SKIRT STEAK 24 SERVED WITH PICKLES, FRIED EGGS & TOMATILLO SALSA PICCALILLI AND MUSTARD GUINEA HEN SIDES WITH MORELS CHIOGGIA BEETS 9 RUSTIC PORK HORSERADISH & NEPITELLA VINEGAR WITH PISTACHIO CAULIFLOWER 9 ROASTED GARLIC & CHERMOULA RABBIT & PRUNE FINGERLING POTATOES 9 PICKLED MUSTARD SEED, ROSEMARY & CREME FRAICHE HEAD CHEESE ROMANO BEANS 9 BRAISED WITH TOMATO, NIGELLA SEED & SHEEP’S MILK RICOTTA LIVERWURST BROCCOLI 9 CALABRIAN CHILI & ANCHOVIES CONSUMING RAW OR UNDERCOOKED MEATS, POULTRY, SEAFOOD, SHELLFISH OR EGGS MAY INCREASE YOUR RISK OF FOODBORNE ILLNESS. -

Peppy Pickles & Relishes
Home Economics Circular September 1958 reppy pickles I p.ettsh,, By KATHRYN J. ORR Specialist in Foods and Nutrition KINDS OF PICKLES Pickled pineapple, tart and sweet .. dills with a tang . .. old-fashioned cu cumber slices . piquant piccalilli .. these typify the four kinds of homemade pickles. Easiest to make are the fruit pickles which are simmered in a sweet-sour sirup. Pineapples and mangos may be preserved in this way. Then there are the quick-processed pickles made from vegetables salted down overnight and combined the next day with boiling-hot vinegar and spice. Next are the brined pickles, also called fermented pickles because they go · through a curing process lasting several weeks. Green tomato and cucumber dills belong in this group, along with brined beans. Last are the relishes, such as tomato catsup, chili sauce, and chutneys made of vegetables or fruits, chopped and sea soned, : or cooked down to a spicy sauce. Best pickled vegetables are firm, clear, even in color throughout with no Cooperative extension work in cloudy or white spots, and have a tart, Agriculture and Home Economics pungent flavor. College of Agriculture Univ,nity of Hawaii United Stoles Pickled fruits are plump, firm but nepartment of Agriculture cooperating tender, and have a spicy, sweet-sour taste. FOR SUCCESS IH PICKLING with other ingredients and then lifted out before pickles are packed. Spices Use only fresh, good-quality fruits packed in the jars with pickles will turn and vegetables . Cucumbers and dark. When using a spice bag, be sure green tomatoes are best pickled with to have a clean, thin, white cloth large in 24 hours of picking. -

Burgers Sides + Desserts
BURGERS BURGER SHOP CLASSIC 8.5 GRASS FED BEEF PATTY, MATURE CHEDDAR, DILL PICKLES, SMOKED MUSTARD MAYO, KETCHUP, BABY GEM, CHALLAH BUN / ADD BACON FOR £1.5 HEREFORD HOP 10 GRASS FED BEEF PATTY, SLOW COOKED BEEF, HOP CHEESE, DILL PICKLES, SMOKED MUSTARD MAYO, KETCHUP, BABY GEM, CHALLAH BUN THE WORCESTER BLUE 10 GRASS FED BEEF PATTY, WORCESTER BLUE CHEESE, BEER ONIONS, BLACK GARLIC MAYO, KETCHUP, BABY GEM, CHALLAH BUN BUTTERMILK CHICKEN 9 HEREFORD FREE RANGE BUTTERMILK FRIED CHICKEN, APPLE SLAW, BLACK GARLIC MAYO, PICKLED RED ONIONS, KETCHUP, BABY GEM, CHALLAH BUN KIMCHI CHICKEN BURGER 9.5 HEREFORD FREE RANGE BUTTERMILK FRIED CHICKEN, HOUSE KIMCHI, PERI PERI MAYO, BABY GEM, CHALLAH BUN BBQ PULLED PORK 8 BBQ PULLED PORK, APPLE SLAW, BBQ SAUCE, MUSTARD MAYO, PICKLED RED CABBAGE, BABY GEM, CHALLAH BUN FALAFEL (VEGAN) 7.5 FALAFEL, APPLE SLAW, PICKLED RED CABBAGE, TAHINI SAUCE, KETCHUP, LEAVES, CHALLAH BUN MAKE ANY BUGRER INTO A SALAD WITH PICKLES AND SLAW ADD BACON OR CHEESE TO ANY BURGER: £1.5 ADD PULLED PORK TO ANY BURGER: £3.5 SWAP YOUR BUN FOR A GLUTEN FREE BUN: £1 SIDES + DESSERTS ROSEMARY CHIPS 3 SWEET POTATO FRIES 4 BBQ CHICKEN WINGS 6 WESTCOMBE CHEESE CURDS + PICCALILLI KETCHUP 5.5 KIMCHI 3.5 HOUSE SLAW (VEGAN) 3.5 PORK LOADED FRIES 9 BBQ PULLED PORK, APPLE SLAW, BBQ SAUCE, MUSTARD MAYO, PICKLED RED CABBAGE, ROSEMARY FRIES VEGAN JACKFRUIT LOADED FRIES 7.5 BBQ JACKFRUIT, ROSEMARY FRIES, VEGAN MAYO HOUSE SAUCES 1 BLACK GARLIC MAYO, PERI PERI MAYO, MUSTARD MAYO, GARLIC+SMOKED PAPRIKA MAYO, BBQ, PICCALILLI KETCHUP SALTED CARAMEL BROWNIE -
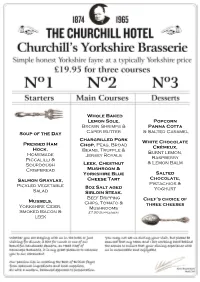
Soup of the Day Pressed Ham Hock, Homemade Piccalilli
Whole Baked Lemon Sole, Popcorn Brown Shrimps & Panna Cotta Soup of the Day Caper Butter & Salted Caramel Chargrilled Pork Pressed Ham White Chocolate Chop, Peas, Broad Crèmeux, Hock, Beans, Truffle & Homemade Burnt lemon, Jersey Royals Raspberry Piccalilli & Sourdough Leek, Chestnut & Lemon Balm Crispbread Mushroom & Yorkshire Blue Salted Salmon Gravlax, Cheese Tart Chocolate, Pistachios & Pickled Vegetable 8oz Salt aged Salad Yoghurt Sirloin Steak, Beef Dripping Mussels, Chef’s choice of Chips, Tomato & three cheeses Yorkshire Cider, Mushrooms Smoked Bacon & £7.50 Supplement leek GrazingGrazing MenuMenu Introducing our menu of small plates showcasing modern British cooking of predominantly humble Yorkshire ingredients. Our chefs suggest selecting three to four dishes per person to graze from and you can always order more if you require. The Head Chef and his team will either send your dishes to your table in the order they feel most appropriate or you can choose this for yourself. Bread & Our Own Butter 3 Confit Duck Egg Yolk, Jacket Potato, Salt & Vinegar 4 Mushroom Macaroons, Chocolate & White Truffle 5 Crispy Ham, Chicken Skin, Cauliflower, Thyme & Truffle 5 Cheese In Cracker, Foraged Salad & Black Truffle 6 Tomato Short Bread, Buffalo Mozzarella, Heritage Tomato & Smoked Potato 7 Pork Belly, Onion Variations & Mushroom Ketchup 7 ‘Fish & Chips’, Sherry Vinegar Jelly & Scraps 7 Hand Dived Scallop, XO Sauce, Puffed Rice & Coriander Shoots 8 24 Hour Braised Lamb Belly, Baby Gem, Peas & Parmesan 9 Hay Smoked Mackerel, BBQ Carrots, Orange & Sea Aster 9 Yorkshire Stout Braised Beef Cheek, Bone Marrow Fudge & Salsify 12 Charred Octopus, Red Pepper, Preserved Lemon, Basil & Mint 12 Yorkshire Foraged Salad 3 Salt Baked Jersey Royals 3 Beef Dripping Chips 3 Popcorn Panna Cotta & Salted Caramel 6 White Chocolate Crèmeux, Burnt lemon, Raspberry & Lemon Balm 6 Salted Chocolate, Pistachios & Yoghurt 6 Lemon Meringue Lolly Pops 4 Churros, Rhubarb & Lemon Thyme Sugar 4 Your Selection of Four Cheeses 10 Chutney & Biscuits.