Inborn Errors of Metabolism
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Incidence of Inborn Errors of Metabolism by Expanded Newborn
Original Article Journal of Inborn Errors of Metabolism & Screening 2016, Volume 4: 1–8 Incidence of Inborn Errors of Metabolism ª The Author(s) 2016 DOI: 10.1177/2326409816669027 by Expanded Newborn Screening iem.sagepub.com in a Mexican Hospital Consuelo Cantu´-Reyna, MD1,2, Luis Manuel Zepeda, MD1,2, Rene´ Montemayor, MD3, Santiago Benavides, MD3, Hector´ Javier Gonza´lez, MD3, Mercedes Va´zquez-Cantu´,BS1,4, and Hector´ Cruz-Camino, BS1,5 Abstract Newborn screening for the detection of inborn errors of metabolism (IEM), endocrinopathies, hemoglobinopathies, and other disorders is a public health initiative aimed at identifying specific diseases in a timely manner. Mexico initiated newborn screening in 1973, but the national incidence of this group of diseases is unknown or uncertain due to the lack of large sample sizes of expanded newborn screening (ENS) programs and lack of related publications. The incidence of a specific group of IEM, endocrinopathies, hemoglobinopathies, and other disorders in newborns was obtained from a Mexican hospital. These newborns were part of a comprehensive ENS program at Ginequito (a private hospital in Mexico), from January 2012 to August 2014. The retrospective study included the examination of 10 000 newborns’ results obtained from the ENS program (comprising the possible detection of more than 50 screened disorders). The findings were the following: 34 newborns were confirmed with an IEM, endocrinopathies, hemoglobinopathies, or other disorders and 68 were identified as carriers. Consequently, the estimated global incidence for those disorders was 3.4 in 1000 newborns; and the carrier prevalence was 6.8 in 1000. Moreover, a 0.04% false-positive rate was unveiled as soon as diagnostic testing revealed negative results. -

EXTENDED CARRIER SCREENING Peace of Mind for Planned Pregnancies
Focusing on Personalised Medicine EXTENDED CARRIER SCREENING Peace of Mind for Planned Pregnancies Extended carrier screening is an important tool for prospective parents to help them determine their risk of having a child affected with a heritable disease. In many cases, parents aren’t aware they are carriers and have no family history due to the rarity of some diseases in the general population. What is covered by the screening? Genomics For Life offers a comprehensive Extended Carrier Screening test, providing prospective parents with the information they require when planning their pregnancy. Extended Carrier Screening has been shown to detect carriers who would not have been considered candidates for traditional risk- based screening. With a simple mouth swab collection, we are able to test for over 419 genes associated with inherited diseases, including Fragile X Syndrome, Cystic Fibrosis and Spinal Muscular Atrophy. The assay has been developed in conjunction with clinical molecular geneticists, and includes genes listed in the NIH Genetic Test Registry. For a list of genes and disorders covered, please see the reverse of this brochure. If your gene of interest is not covered on our Extended Carrier Screening panel, please contact our friendly team to assist you in finding a gene test panel that suits your needs. Why have Extended Carrier Screening? Extended Carrier Screening prior to pregnancy enables couples to learn about their reproductive risk and consider a complete range of reproductive options, including whether or not to become pregnant, whether to use advanced reproductive technologies, such as preimplantation genetic diagnosis, or to use donor gametes. -

Amino Acid Disorders 105
AMINO ACID DISORDERS 105 Massaro, A. S. (1995). Trypanosomiasis. In Guide to Clinical tions in biological fluids relatively easy. These Neurology (J. P. Mohrand and J. C. Gautier, Eds.), pp. 663– analyzers separate amino acids either by ion-ex- 667. Churchill Livingstone, New York. Nussenzweig, V., Sonntag, R., Biancalana, A., et al. (1953). Ac¸a˜o change chromatography or by high-pressure liquid de corantes tri-fenil-metaˆnicos sobre o Trypanosoma cruzi in chromatography. The results are plotted as a graph vitro: Emprego da violeta de genciana na profilaxia da (Fig. 1). The concentration of each amino acid can transmissa˜o da mole´stia de chagas por transfusa˜o de sangue. then be calculated from the size of the corresponding O Hospital (Rio de Janeiro) 44, 731–744. peak on the graph. Pagano, M. A., Segura, M. J., DiLorenzo, G. A., et al. (1999). Cerebral tumor-like American trypanosomiasis in Most amino acid disorders can be diagnosed by acquired immunodeficiency syndrome. Ann. Neurol. 45, measuring the concentrations of amino acids in 403–406. blood plasma; however, some disorders of amino Rassi, A., Trancesi, J., and Tranchesi, B. (1982). Doenc¸ade acid transport are more easily recognized through the Chagas. In Doenc¸as Infecciosas e Parasita´rias (R. Veroesi, Ed.), analysis of urine amino acids. Therefore, screening 7th ed., pp. 674–712. Guanabara Koogan, Sa˜o Paulo, Brazil. Spina-Franc¸a, A., and Mattosinho-Franc¸a, L. C. (1988). for amino acid disorders is best done using both South American trypanosomiasis (Chagas’ disease). In blood and urine specimens. Occasionally, analysis of Handbook of Clinical Neurology (P. -

Disease Reference Book
The Counsyl Foresight™ Carrier Screen 180 Kimball Way | South San Francisco, CA 94080 www.counsyl.com | [email protected] | (888) COUNSYL The Counsyl Foresight Carrier Screen - Disease Reference Book 11-beta-hydroxylase-deficient Congenital Adrenal Hyperplasia .................................................................................................................................................................................... 8 21-hydroxylase-deficient Congenital Adrenal Hyperplasia ...........................................................................................................................................................................................10 6-pyruvoyl-tetrahydropterin Synthase Deficiency ..........................................................................................................................................................................................................12 ABCC8-related Hyperinsulinism........................................................................................................................................................................................................................................ 14 Adenosine Deaminase Deficiency .................................................................................................................................................................................................................................... 16 Alpha Thalassemia............................................................................................................................................................................................................................................................. -

Amino Acid Disorders
471 Review Article on Inborn Errors of Metabolism Page 1 of 10 Amino acid disorders Ermal Aliu1, Shibani Kanungo2, Georgianne L. Arnold1 1Children’s Hospital of Pittsburgh, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA; 2Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo, MI, USA Contributions: (I) Conception and design: S Kanungo, GL Arnold; (II) Administrative support: S Kanungo; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: E Aliu, GL Arnold; (V) Data analysis and interpretation: None; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Georgianne L. Arnold, MD. UPMC Children’s Hospital of Pittsburgh, 4401 Penn Avenue, Suite 1200, Pittsburgh, PA 15224, USA. Email: [email protected]. Abstract: Amino acids serve as key building blocks and as an energy source for cell repair, survival, regeneration and growth. Each amino acid has an amino group, a carboxylic acid, and a unique carbon structure. Human utilize 21 different amino acids; most of these can be synthesized endogenously, but 9 are “essential” in that they must be ingested in the diet. In addition to their role as building blocks of protein, amino acids are key energy source (ketogenic, glucogenic or both), are building blocks of Kreb’s (aka TCA) cycle intermediates and other metabolites, and recycled as needed. A metabolic defect in the metabolism of tyrosine (homogentisic acid oxidase deficiency) historically defined Archibald Garrod as key architect in linking biochemistry, genetics and medicine and creation of the term ‘Inborn Error of Metabolism’ (IEM). The key concept of a single gene defect leading to a single enzyme dysfunction, leading to “intoxication” with a precursor in the metabolic pathway was vital to linking genetics and metabolic disorders and developing screening and treatment approaches as described in other chapters in this issue. -

Living with Classical Homocystinuria
Living with Classical Homocystinuria This brochure will help you understand what classical homocystinuria is, how it affects your body, and how you can manage your condition A few words about this brochure What is homocystinuria? Has your doctor diagnosed you or your child You may have heard the word “homocystinuria” with homocystinuria (HO-mo-SIS-tin-YUR- for the first time when your doctor talked to ee-uh)? There are three types of genetic you about possibly having this condition. disorders that cause homocystinuria. Each Homocystinuria is a rare disorder involving type has a different cause and different the amino acid homocysteine (HO-mo-SIS- health issues. This brochure will talk about teen). Amino acids are building blocks that your classical homocystinuria. The information body uses to make proteins. Homocystinuria will help you understand classical occurs when there is a buildup of the amino acid homocystinuria and how you can manage homocysteine in your blood and urine. your condition. High levels of homocysteine can be harmful to your body. You may be reading this brochure because you have classical homocystinuria or Why is there homocysteine because your child or a sibling or a friend in your body? has it. Or perhaps you’re a healthcare professional. Please note the brochure It starts with the foods you eat. Your body addresses “you,” but it’s understood that makes homocysteine from another amino acid “you,” the reader, may not have classical called methionine (meh-THIGH-uh-neen). Most homocystinuria yourself. foods contain some methionine. But high-protein foods such as meat, fish, eggs, or cheese tend to have the most methionine. -

Blueprint Genetics Hyperammonemia and Urea Cycle Disorder Panel
Hyperammonemia and Urea Cycle Disorder Panel Test code: ME1601 Is a 49 gene panel that includes assessment of non-coding variants. Is ideal for patients with hyperammonemia or a clinical suspicion of a disorder of urea cycle metabolism. The genes on this panel are included in the Comprehensive Metabolism Panel. About Hyperammonemia and Urea Cycle Disorder Congenital urea cycle disorders are the result of defects in the metabolism of nitrogen waste. Deficiency of any of the enzymes in the urea cycle results in an excess of ammonia or other precursor metabolites in the blood. Normally, urea production lowers the ammonia levels in the blood but in the case of defective enzymes, the urea cycle is disturbed. Infants with urea cycle disorders (UCDs) develop cerebral edema, lethargy, hypothermia, neurologic signs and coma, often shortly after birth. Partial, or milder, UCDs are possible if the affected enzyme is positioned in a later phase of the urea cycle. Patients with UCDs may present with hyperammonemia often triggered by stress or illness. The most common primary hyperammonemia is X-linked recessive ornithine transcarbamylase deficiency caused by mutations in the OTC gene. The estimated prevalence is 1:56,000. Prevalence estimates for the other specific urea cycle disorders are 1:200,000 for ASL- and ASS1-related deficiencies and <1:1,000,000 for ARG1, CPS1 and NAGS-related deficiencies. The diagnostic yield ranges from 50% to 80% for different primary urea cycle disorders. In addition to congenital UCDs, this panel has the ability to diagnose other diseases of early phase hyperammonemia and other inborn errors of metabolism showing similar and overlapping symptoms. -

Tyrosinemia, Type 11 Or 111 (TYR II/TYR 111) CAUSE Tyrosinemia Type II and III Affect an Enzyme Needed to Break Down Proteins from the Food We Eat
KENTUCKY NEWBORN SCREENING PROGRAM PARENT TEACHING SHEET Kentucky Newborn Screening Program, 275 East Main Street, Frankfort, KY 40621, Phone (502) 564-3756, Fax (502) 564-1510 Tyrosinemia, type 11 or 111 (TYR II/TYR 111) CAUSE Tyrosinemia type II and III affect an enzyme needed to break down proteins from the food we eat. In tyrosinemia type II and II, the enzyme used to break down proteins is missing or not working properly. A person who has tyrosinemia type II or III doesn’t have enough enzyme to break down protein containing tyrosine. When the body can’t break down tyrosine, it builds up in the body and causes health problems. Tyrosinemia type II and III are genetic disorders that are passed on (inherited) from parents to a child. The mother and father of an affected child carry a gene change that can cause tyrosinemia type I. Parents usually do not have signs or symptoms, or even know they carry the gene change. IF NOT TREATED Tyrosinemia type II or III are different for each child. Some children with tyrosinemia type II or III have only a few health problems, while other children may have serious complications. If tyrosinemia II or III is not treated, a child might develop: • Poor coordination and balance • Intellectual disability • Eye problems (Type II) • Behavior changes (Type II) • Skin lesion (Type II) • Seizures (Type III) It is very important to follow the doctor’s instructions for testing and treatment. TREATMENT OPTIONS Tyrosinemia type II and III can be treated. Treatment is life-long and can include: • Low protein diet- a dietician will help you with the best diet for your child • Medications to lower amino acid levels. -
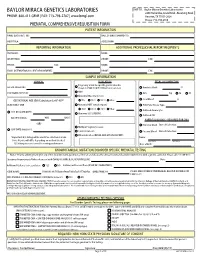
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -

Richner-Hanhart Syndrome (Tyrosinemia Type II)
CASE LETTER Richner-Hanhart Syndrome (Tyrosinemia Type II) Fanny Locatelli, MD; Eve Puzenat, MD; Jean Bernard Arnoux, MD; Dominique Blanc, MD; François Aubin, MD, PhD of Richner-Hanhart syndrome. Diagnosis was confirmed PRACTICE POINTS by an elevated plasma level of tyrosine (1580 µmol/L; • Richner-Hanhart syndrome (tyrosinemia type II) reference range, 40–80 µmol/L). should be suspected in patients demonstrating A low tyrosine and low phenylalanine diet (no ani- cutaneous lesions, especially palmoplantar kerato- mal proteins) was immediately introduced, with supple- sis associated with bilateral pseudodendritic corneal mentation of amino acids, vitamins, and trace elements. lesions unresponsive to antiviral therapy. After 8 days, the plasma level of tyrosinemia decreased • Early diagnosis and initiation of a tyrosine- by a factor of 4 (392 µmol/L). After 1 month, the cutane- phenylalanine–restricted diet in infancy is the most ous and ocular copylesions completely resolved (Figure, B). effective therapy to prevent mental retardation. Discrete psychomotor slowing still persisted for 1 year and then reached complete normalization. Genetic analy- sis showed a composite heterozygous mutation of the tyrosine aminotransferase gene, TAT, on chromosome 16. To the Editor: Thenot mutation detected in the patient’s mother was an Richner-Hanhart syndrome, also known as tyrosinemia A to V substitution at codon 147 (A147V). The second type II or oculocutaneous tyrosinemia, is a rare autosomal- mutation was detected in the father; it was an 8 nucleo- recessive, childhood-onset, metabolic hereditary disease.1 tides duplication and then a substitution leading to a A deficiency of tyrosine aminotransferase leads toDo an premature stop codon at codon 37 (R37X). -

Disorders Alphabetical by Disease Updated 1/2020
Disorders Alphabetical by Disease updated 1/2020 Disorders Abbreviation Classification Recommended Uniform Screening Panel (RUSP) Classification 2,4 Dienoyl CoA Reductase Deficiency DE RED Fatty Acid Oxidation Disorder Secondary Condition 2-Methyl 3 Hydroxy Butyric Aciduria 2M3HBA Organic Acid Disorder Secondary Condition 2-Methyl Butyryl-CoA Dehydrogenase Deficiency 2MBG Organic Acid Disorder Secondary Condition (called 2-Methylbutyrylglycinuria on RUSP) 3-Hydroxy-3-Methylglutaryl CoA Lyase Deficiency HMG Organic Acid Disorder Core Condition 3-Methylcrotonyl CoA Carboxylase Deficiency 3MCC Organic Acid Disorder Core Condition 3-Methylglutaconic Aciduria 3MGA Organic Acid Disorder Secondary Condition Alpha-Thalassemia (Bart's Hb) Hemoglobin Bart's Hemoglobin Disorder Secondary Conditoin Argininemia, Arginase Deficiency ARG Amino Acid Disorder Secondary Condition Arginosuccinic Aciduria ASA Amino Acid Disorder Core Condition Benign Hyperphenylalaninemia PHE Amino Acid Disorder Secondary Condition Beta-Ketothiolase Deficiency BKT Organic Acid Disorder Core Condition Biopterin Defect in Cofactor Biosynthesis BIOPT (BS) Amino Acid Disorder Secondary Condition Biopterin Defect in Cofactor Regeneration BIOPT (Reg) Amino Acid Disorder Secondary Condition Biotinidase Deficiency BIO Metabolic Disorder of Biotin Recycling Core Condition Carbamoyltransferase Deficiency, Carbamoyl Phosphate Synthetase I Deficiency CPS Amino Acid Disorder Not on RUSP Carnitine Palmitoyl Transferase Deficiency Type 1 CPT I Fatty Acid Oxidation Disorder Secondary Condition -

Diseases Catalogue
Diseases catalogue AA Disorders of amino acid metabolism OMIM Group of disorders affecting genes that codify proteins involved in the catabolism of amino acids or in the functional maintenance of the different coenzymes. AA Alkaptonuria: homogentisate dioxygenase deficiency 203500 AA Phenylketonuria: phenylalanine hydroxylase (PAH) 261600 AA Defects of tetrahydrobiopterine (BH 4) metabolism: AA 6-Piruvoyl-tetrahydropterin synthase deficiency (PTS) 261640 AA Dihydropteridine reductase deficiency (DHPR) 261630 AA Pterin-carbinolamine dehydratase 126090 AA GTP cyclohydrolase I deficiency (GCH1) (autosomal recessive) 233910 AA GTP cyclohydrolase I deficiency (GCH1) (autosomal dominant): Segawa syndrome 600225 AA Sepiapterin reductase deficiency (SPR) 182125 AA Defects of sulfur amino acid metabolism: AA N(5,10)-methylene-tetrahydrofolate reductase deficiency (MTHFR) 236250 AA Homocystinuria due to cystathionine beta-synthase deficiency (CBS) 236200 AA Methionine adenosyltransferase deficiency 250850 AA Methionine synthase deficiency (MTR, cblG) 250940 AA Methionine synthase reductase deficiency; (MTRR, CblE) 236270 AA Sulfite oxidase deficiency 272300 AA Molybdenum cofactor deficiency: combined deficiency of sulfite oxidase and xanthine oxidase 252150 AA S-adenosylhomocysteine hydrolase deficiency 180960 AA Cystathioninuria 219500 AA Hyperhomocysteinemia 603174 AA Defects of gamma-glutathione cycle: glutathione synthetase deficiency (5-oxo-prolinuria) 266130 AA Defects of histidine metabolism: Histidinemia 235800 AA Defects of lysine and