Digestive-System,-20-Times.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-Tailed Opossum (Monodelphis Domestica) and North American Opossum (Didelphis Virginiana)
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Doctoral Dissertations Graduate School 12-2001 Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana) Lee Anne Cope University of Tennessee - Knoxville Follow this and additional works at: https://trace.tennessee.edu/utk_graddiss Part of the Animal Sciences Commons Recommended Citation Cope, Lee Anne, "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana). " PhD diss., University of Tennessee, 2001. https://trace.tennessee.edu/utk_graddiss/2046 This Dissertation is brought to you for free and open access by the Graduate School at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Doctoral Dissertations by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. To the Graduate Council: I am submitting herewith a dissertation written by Lee Anne Cope entitled "Comparative Anatomy of the Lower Respiratory Tract of the Gray Short-tailed Opossum (Monodelphis domestica) and North American Opossum (Didelphis virginiana)." I have examined the final electronic copy of this dissertation for form and content and recommend that it be accepted in partial fulfillment of the equirr ements for the degree of Doctor of Philosophy, with a major in Animal Science. Robert W. Henry, Major Professor We have read this dissertation and recommend its acceptance: Dr. R.B. Reed, Dr. C. Mendis-Handagama, Dr. J. Schumacher, Dr. S.E. Orosz Accepted for the Council: Carolyn R. -

48 Anal Canal
Anal Canal The rectum is a relatively straight continuation of the colon about 12 cm in length. Three internal transverse rectal valves (of Houston) occur in the distal rectum. Infoldings of the submucosa and the inner circular layer of the muscularis externa form these permanent sickle- shaped structures. The valves function in the separation of flatus from the developing fecal mass. The mucosa of the first part of the rectum is similar to that of the colon except that the intestinal glands are slightly longer and the lining epithelium is composed primarily of goblet cells. The distal 2 to 3 cm of the rectum forms the anal canal, which ends at the anus. Immediately proximal to the pectinate line, the intestinal glands become shorter and then disappear. At the pectinate line, the simple columnar intestinal epithelium makes an abrupt transition to noncornified stratified squamous epithelium. After a short transition, the noncornified stratified squamous epithelium becomes continuous with the keratinized stratified squamous epithelium of the skin at the level of the external anal sphincter. Beneath the epithelium of this region are simple tubular apocrine sweat glands, the circumanal glands. Proximal to the pectinate line, the mucosa of the anal canal forms large longitudinal folds called rectal columns (of Morgagni). The distal ends of the rectal columns are united by transverse mucosal folds, the anal valves. The recess above each valve forms a small anal sinus. It is at the level of the anal valves that the muscularis mucosae becomes discontinuous and then disappears. The submucosa of the anal canal contains numerous veins that form a large hemorrhoidal plexus. -

Smoothelin Expression in the Gastrointestinal Tract: Implication in Colonic Inertia Owen T.M
RESEARCH ARTICLE Smoothelin Expression in the Gastrointestinal Tract: Implication in Colonic Inertia Owen T.M. Chan, MD, PhD,* Lauren Chiles, MD,* Mary Levy, DO,* Jing Zhai, MD, PhD,* Lisa M. Yerian, MD,w Haodong Xu, MD, PhD,z Shu-Yuan Xiao, MD,y Edy E. Soffer, MD,8 Jeffrey L. Conklin, MD,8 Deepti Dhall, MD,* Melissa E. Kahn, MD,* Bonnie L. Balzer, MD,* Mahul B. Amin, MD,* and Hanlin L. Wang, MD, PhD*z Key Words: smoothelin, colonic inertia, intestinal motility Abstract: Colonic inertia is a frustrating motility disorder to disorder, chronic intestinal pseudo-obstruction, slow transit patients, clinicians, and pathologists. The pathogenesis is largely constipation unknown. The aims of this study were to: (1) characterize the expression of smoothelin, a novel smooth muscle-specific con- (Appl Immunohistochem Mol Morphol 2013;21:452–459) tractile protein expressed only by terminally differentiated smooth muscle cells, in the normal gastrointestinal (GI) tract; and (2) determine whether smoothelin is aberrantly expressed in hronic constipation is a frequent complaint, being patients with colonic inertia. A total of 57 resections of the Creported in up to 16% of women and 12% of men.1 normal GI tract (distal esophagus to left colon) were obtained Clinically, constipation and colonic motility disorders are from patients without GI motor dysfunction. Sixty-one colon defined by not only infrequent bowel movements, but also resections were obtained from patients with a clinical diagnosis other manifestations such as excessive straining, hard of colonic inertia. Smoothelin immunostaining was conducted stools, incomplete evacuation, sensation of obstruction, on full-thickness tissue sections. In the nondysmotile controls, and manual maneuvers to facilitate defecation.2,3 General strong and diffuse cytoplasmic staining for smoothelin was ob- management of constipation includes conservative thera- served in both the inner circular and outer longitudinal layers of pies, such as behavioral modification, bulking agents, os- the muscularis propria (MP) throughout the entire GI tract. -

Normal Gross and Histologic Features of the Gastrointestinal Tract
NORMAL GROSS AND HISTOLOGIC 1 FEATURES OF THE GASTROINTESTINAL TRACT THE NORMAL ESOPHAGUS left gastric, left phrenic, and left hepatic accessory arteries. Veins in the proximal and mid esopha- Anatomy gus drain into the systemic circulation, whereas Gross Anatomy. The adult esophagus is a the short gastric and left gastric veins of the muscular tube measuring approximately 25 cm portal system drain the distal esophagus. Linear and extending from the lower border of the cri- arrays of large caliber veins are unique to the distal coid cartilage to the gastroesophageal junction. esophagus and can be a helpful clue to the site of It lies posterior to the trachea and left atrium a biopsy when extensive cardiac-type mucosa is in the mediastinum but deviates slightly to the present near the gastroesophageal junction (4). left before descending to the diaphragm, where Lymphatic vessels are present in all layers of the it traverses the hiatus and enters the abdomen. esophagus. They drain to paratracheal and deep The subdiaphragmatic esophagus lies against cervical lymph nodes in the cervical esophagus, the posterior surface of the left hepatic lobe (1). bronchial and posterior mediastinal lymph nodes The International Classification of Diseases in the thoracic esophagus, and left gastric lymph and the American Joint Commission on Cancer nodes in the abdominal esophagus. divide the esophagus into upper, middle, and lower thirds, whereas endoscopists measure distance to points in the esophagus relative to the incisors (2). The esophagus begins 15 cm from the incisors and extends 40 cm from the incisors in the average adult (3). The upper and lower esophageal sphincters represent areas of increased resting tone but lack anatomic landmarks; they are located 15 to 18 cm from the incisors and slightly proximal to the gastroesophageal junction, respectively. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria. -

Histopathology of Barrett's Esophagus and Early-Stage
Review Histopathology of Barrett’s Esophagus and Early-Stage Esophageal Adenocarcinoma: An Updated Review Feng Yin, David Hernandez Gonzalo, Jinping Lai and Xiuli Liu * Department of Pathology, Immunology, and Laboratory Medicine, College of Medicine, University of Florida, Gainesville, FL 32610, USA; fengyin@ufl.edu (F.Y.); hernand3@ufl.edu (D.H.G.); jinpinglai@ufl.edu (J.L.) * Correspondence: xiuliliu@ufl.edu; Tel.: +1-352-627-9257; Fax: +1-352-627-9142 Received: 24 October 2018; Accepted: 22 November 2018; Published: 27 November 2018 Abstract: Esophageal adenocarcinoma carries a very poor prognosis. For this reason, it is critical to have cost-effective surveillance and prevention strategies and early and accurate diagnosis, as well as evidence-based treatment guidelines. Barrett’s esophagus is the most important precursor lesion for esophageal adenocarcinoma, which follows a defined metaplasia–dysplasia–carcinoma sequence. Accurate recognition of dysplasia in Barrett’s esophagus is crucial due to its pivotal prognostic value. For early-stage esophageal adenocarcinoma, depth of submucosal invasion is a key prognostic factor. Our systematic review of all published data demonstrates a “rule of doubling” for the frequency of lymph node metastases: tumor invasion into each progressively deeper third of submucosal layer corresponds with a twofold increase in the risk of nodal metastases (9.9% in the superficial third of submucosa (sm1) group, 22.0% in the middle third of submucosa (sm2) group, and 40.7% in deep third of submucosa (sm3) group). Other important risk factors include lymphovascular invasion, tumor differentiation, and the recently reported tumor budding. In this review, we provide a concise update on the histopathological features, ancillary studies, molecular signatures, and surveillance/management guidelines along the natural history from Barrett’s esophagus to early stage invasive adenocarcinoma for practicing pathologists. -

Unit V – Problem 6 – Histology: Large Intestine and Appendix
Unit V – Problem 6 – Histology: Large Intestine and Appendix - Colon: The colon has no villi. The epithelium is simple columnar with numerous goblet cells. In the lamina propria are found deep intestinal glands, blood vessels and lymphatic nodules. The muscularis mucosae is present. In the submucosa are blood vessels, submucosal plexuses & some lymphatic nodules. The muscularis externa consists of inner circular smooth muscle fibers & outer longitudinal smooth muscle fibers which are arranged in three longitudinal bands called teniae coli (between the muscle layers are myenteric plexuses). The serosa is only found in the transverse and sigmoid parts of the colon. - Appendix: Simple columnar epithelium with goblet cells (no villi) and shorter less developed intestinal glands. The lamina propria contains diffuse lymphatic nodules with germinal centers. Muscularis mucosa is present. There are submucosa, muscularis externa (with inner circular and outer longitudinal smooth muscle fibers: between them are myenteric plexuses) & serosa. - Rectum: It has no villi. The epithelium is simple columnar with brush border and goblet cells. In the lamina propria are found deep intestinal glands and lymphatic nodules. There are submucosa, muscularis externa (arranged into inner circular & outer longitudinal smooth muscle fibers) & serosa. - Anorectal junction: Transition from the rectal epithelium (simple columnar) to the epithelium of the skin (non-keratinized stratified squamous epithelium). In the anal canal are found internal hemorrhoid plexus of veins, thickening of the circular smooth muscle to form the internal anal sphincter & the skeletal external anal sphincter. . -
Digestive System
Digestive system Dr. Anna L. Kiss Department of Anatomy, Histology and Embryology Semmelweis University Budapest 2019 The gastrointestinal tract (GI tract): digestion and excretion Upper gastrointestinal tract The upper GI tract consists of the mouth, pharynx, esophagus, and stomach. The lower GI tract. small intestine, which has three parts: -duodenum -jejunum -ileum large intestine, which has three parts: -cecum (the vermiform appendix is attached to the cecum). -colon (ascending colon, transverse colon, descending colon and sigmoid flexure) -rectum Primitive Gut Tube Coeliac trunk Superior mesenteric artery Inferior mesenteric artery Vitelline duct Umbilical loop Umbilical artery Final Position of Parts of Gut Tube Abdominal esophagus Thoracic esophagus Liver Stomach Gall bladder & bile duct Duodenum Pancreas 2.) Transverse colon Jejunum & ileum 1.) Ascending colon 3.) Descending colon Cecum Appendix 4.) Sigmoid colon Final Position of Parts of Gut Tube Stomach: left hypochondric region (intraperitoneal) Duodenum: right side (partly retroperitoneal) Jejunum, ileum: umbilical + iliac region (intraperitoneal) Appendix: right side (Mc Burney point) (intraperitoneal) Ascending colon: right iliac region Transverse colon: middle position (intraperitoneal) Descending colon: left iliac region Sigmoid colon: sacral and pelvic region (intraperitoneal) highly acidic environment due to gastric acid production The stomach lies between the esophagus and the duodenum It is on the left side of the abdominal cavity. Stomach fundus cardia rugae!! lesser curvature body pylorus greater curvature Diaphragm Fundus pyloric antrum Corpus superior part body (duodenum) Greater curvature descending part (duodenum) ascending part Jejunum horizontal part Histology of the gut Mucosa: • epithelium: simple columnar (goblet cells) • propria (lymphoreticular connective tissue): glands (Lieberkhün crypts) • muscularis mucosae (2 layered smooth muscle) Submucosa: loose connective tissue (submucosus plexus; glands, lymphatic follicles) External muscle layer (t. -
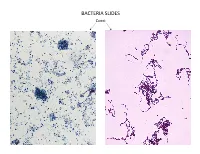
Bacteria Slides
BACTERIA SLIDES Cocci Bacillus BACTERIA SLIDES _______________ __ BACTERIA SLIDES Spirilla BACTERIA SLIDES ___________________ _____ BACTERIA SLIDES Bacillus BACTERIA SLIDES ________________ _ LUNG SLIDE Bronchiole Lumen Alveolar Sac Alveoli Alveolar Duct LUNG SLIDE SAGITTAL SECTION OF HUMAN HEAD MODEL Superior Concha Auditory Tube Middle Concha Opening Inferior Concha Nasal Cavity Internal Nare External Nare Hard Palate Pharyngeal Oral Cavity Tonsils Tongue Nasopharynx Soft Palate Oropharynx Uvula Laryngopharynx Palatine Tonsils Lingual Tonsils Epiglottis False Vocal Cords True Vocal Cords Esophagus Thyroid Cartilage Trachea Cricoid Cartilage SAGITTAL SECTION OF HUMAN HEAD MODEL LARYNX MODEL Side View Anterior View Hyoid Bone Superior Horn Thyroid Cartilage Inferior Horn Thyroid Gland Cricoid Cartilage Trachea Tracheal Rings LARYNX MODEL Posterior View Epiglottis Hyoid Bone Vocal Cords Epiglottis Corniculate Cartilage Arytenoid Cartilage Cricoid Cartilage Thyroid Gland Parathyroid Glands LARYNX MODEL Side View Anterior View ____________ _ ____________ _______ ______________ _____ _____________ ____________________ _____ ______________ _____ _________ _________ ____________ _______ LARYNX MODEL Posterior View HUMAN HEART & LUNGS MODEL Larynx Tracheal Rings Found on the Trachea Left Superior Lobe Left Inferior Lobe Heart Right Superior Lobe Right Middle Lobe Right Inferior Lobe Diaphragm HUMAN HEART & LUNGS MODEL Hilum (curvature where blood vessels enter lungs) Carina Pulmonary Arteries (Blue) Pulmonary Veins (Red) Bronchioles Apex (points -

Terminology: Nomenclature of Mucosa-Associated Lymphoid Tissue
nature publishing group ARTICLES See COMMENTARY page 8 See REVIEW page 11 Terminology: nomenclature of mucosa-associated lymphoid tissue P B r a n d t z a e g 1 , H K i y o n o 2 , R P a b s t 3 a n d M W R u s s e l l 4 Stimulation of mucosal immunity has great potential in vaccinology and immunotherapy. However, the mucosal immune system is more complex than the systemic counterpart, both in terms of anatomy (inductive and effector tissues) and effectors (cells and molecules). Therefore, immunologists entering this field need a precise terminology as a crucial means of communication. Abbreviations for mucosal immune-function molecules related to the secretory immunoglobulin A system were defined by the Society for Mucosal Immunolgy Nomenclature Committee in 1997, and are briefly recapitulated in this article. In addition, we recommend and justify standard nomenclature and abbreviations for discrete mucosal immune-cell compartments, belonging to, and beyond, mucosa-associated lymphoid tissue. INTRODUCTION for dimers (and larger polymers) of IgA and pentamers of It is instructive to categorize various tissue compartments IgM was proposed in 1974. 3,4 The epithelial glycoprotein involved in mucosal immunity according to their main function. designated secretory component (SC) by WHO in 1972 However, until recently, there was no consensus in the scientific (previously called “ transport piece ” or “ secretory piece ” ) turned community as to how these compartments should be named and out to be responsible for the receptor-mediated transcytosis classified. This lack of standardized terminology has been particu- of J-chain-containing Ig polymers (pIgs) through secretory larly confusing for newcomers to the mucosal immunology field. -

An Immunohistochemical Study of Gastric Mucosa and Critical Review Indicate That the Subepithelial Telocytes Are Prelymphatic Endothelial Cells
medicina Article An Immunohistochemical Study of Gastric Mucosa and Critical Review Indicate That the Subepithelial Telocytes Are Prelymphatic Endothelial Cells Oana D. Toader 1, Mugurel C. Rusu 2,* , Lauren¸tiuMogoantă 3, Sorin Hostiuc 4 , Adelina Maria Jianu 5 and Adrian Cosmin Ilie 5 1 Department XIII of Obstetrics, Gynecology and Neonatology, “Polizu” Clinical Hospital, “Carol Davila” University of Medicine and Pharmacy, 020021 Bucharest, Romania 2 Division of Anatomy, Faculty of Dental Medicine, “Carol Davila” University of Medicine and Pharmacy, 020021 Bucharest, Romania 3 Department of Histology, University of Medicine and Pharmacy Craiova, 2 Petru Rares Street, 200349 Craiova, Dolj, Romania 4 Department of Legal Medicine and Bioethics, Faculty of Dental Medicine, “Carol Davila” University of Medicine and Pharmacy, 020021 Bucharest, Romania 5 Division of Anatomy, “Victor Babe¸s”University of Medicine and Pharmacy, 300041 Timi¸soara,Romania * Correspondence: [email protected]; Tel.: +4-072-236-3705 Received: 28 March 2019; Accepted: 20 June 2019; Published: 27 June 2019 Abstract: Background and Objectives: There are only a few studies regarding gut subepithelial telocytes (TCs). The telopodes, namely peculiar TCs’ prolongations described on two-dimensional cuts, are not enough to differentiate this specific cell type. Subepithelial TCs were associated with the intestinal stem niche but a proper differential diagnosis with lymphatic endothelial cells (LECs) was not performed. In this study, we will also critically review studies suggesting that distinctive TCs could be positioned within the lamina propria. Materials and Methods: We performed an immunohistochemical study of human gastric mucosa to test the expression of D2-40, the lymphatic marker, as well as that of CD31, CD34, CD44, CD117/c-kit, α-smooth muscle actin (α-SMA) and vimentin in the gastric subepithelial niche. -

46 Small Intestine
Small Intestine The small intestine extends between the stomach and colon and is divided into the duodenum, jejunum, and ileum. Although there are minor microscopic differences among these subdivisions, all have the same basic organization as the rest of the digestive tube - mucosa, submucosa, muscularis externa, and serosa or adventitia. The transition from one segment to another is gradual. The proximal 12 inches of its length is generally considered duodenum, the remaining proximal two-fifths jejunum and the distal three-fifths ileum. The small intestine moves chyme from the stomach to the colon and completes the digestive processes by adding enzymes secreted by the intestinal mucosa and accessory glands (liver and pancreas). Its primary function, however, is absorption. Approximately 8 to 9 liters of fluid enters the small intestine on a daily basis. Food and liquid intake represents 1-2 liters of this volume the remainder coming from endogenous sources such as salivary, gastric, intestinal, pancreatic, and biliary secretions. Of this volume 6-7 liters is absorbed in the small intestine with only 1-2 liters entering the colon the majority of which is absorbed at this location. Only as very small amount of fluid is evacuated in the stool. The majority of water is absorbed passively in the gut and is largely dependent on an osmotic gradient. Specializations for Absorption Three specializations - plicae circulares, intestinal villi, and microvilli - markedly increase the surface area of the intestinal mucosa to enhance the absorptive process. It is estimated that these morphological features provide an absorptive surface area of 200 M2. Plicae circulares are large, permanent folds that consist of the intestinal mucosa and a core of submucosa.