Constipation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nutritional Disturbances in Crohn's Disease ANTHONY D
Postgrad Med J: first published as 10.1136/pgmj.59.697.690 on 1 November 1983. Downloaded from Postgraduate Medical Journal (November 1983) 59, 690-697 Nutritional disturbances in Crohn's disease ANTHONY D. HARRIES RICHARD V. HEATLEY* M.A., M.R.C.P. M.D., M.R.C.P. Department of Gastroenterology, University Hospital of Wales, Cardiffand *Department ofMedicine, St James's University Hospital, Leeds LS9 7TF Summary deficiency in the same patient. The most important A wide range of nutritional disturbances may be causes of malnutrition are probably reduced food found in patients with Crohn's disease. As more intake, active inflammation and enteric loss of sophisticated tests become available to measure nutrients (Dawson, 1972). vitamin and trace element deficiencies, so these are being recognized as complications ofCrohn's disease. TABLE 1. Pathogenesis of malnutrition It is important to recognize nutritional deficiencies at an early stage and initiate appropriate treatment. Reduced food intake Anorexia Otherwise many patients, experiencing what can be a Fear of eating from abdominal pain chronic and debilitating illness, may suffer unneces- Active inflammation Mechanisms unknown Protected by copyright. sarily from the consequences of deprivation of vital Enteric loss of nutrients Exudation from intestinal mucosa nutrients. Interrupted entero-hepatic circulation Malabsorption Loss of absorptive surface from disease, resection or by-pass KEY WORDS: growth disturbance, Crohn's disease, anaemia, vitamin deficiency. Stagnant loop syndrome from strictures, fistulae or surgically created blind loops Introduction Miscellaneous Rapid gastrointestinal transit Effects of medical therapy Crohn's disease is a chronic inflammatory condi- Effects of parenteral nutrition tion ofunknown aetiology that may affect any part of without trace element supplements the gastrointestinal tract from mouth to anus. -

Does Your Patient Have Bile Acid Malabsorption?
NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #198 NUTRITION ISSUES IN GASTROENTEROLOGY, SERIES #198 Carol Rees Parrish, MS, RDN, Series Editor Does Your Patient Have Bile Acid Malabsorption? John K. DiBaise Bile acid malabsorption is a common but underrecognized cause of chronic watery diarrhea, resulting in an incorrect diagnosis in many patients and interfering and delaying proper treatment. In this review, the synthesis, enterohepatic circulation, and function of bile acids are briefly reviewed followed by a discussion of bile acid malabsorption. Diagnostic and treatment options are also provided. INTRODUCTION n 1967, diarrhea caused by bile acids was We will first describe bile acid synthesis and first recognized and described as cholerhetic enterohepatic circulation, followed by a discussion (‘promoting bile secretion by the liver’) of disorders causing bile acid malabsorption I 1 enteropathy. Despite more than 50 years since (BAM) including their diagnosis and treatment. the initial report, bile acid diarrhea remains an underrecognized and underappreciated cause of Bile Acid Synthesis chronic diarrhea. One report found that only 6% Bile acids are produced in the liver as end products of of British gastroenterologists investigate for bile cholesterol metabolism. Bile acid synthesis occurs acid malabsorption (BAM) as part of the first-line by two pathways: the classical (neutral) pathway testing in patients with chronic diarrhea, while 61% via microsomal cholesterol 7α-hydroxylase consider the diagnosis only in selected patients (CYP7A1), or the alternative (acidic) pathway via or not at all.2 As a consequence, many patients mitochondrial sterol 27-hydroxylase (CYP27A1). are diagnosed with other causes of diarrhea or The classical pathway, which is responsible for are considered to have irritable bowel syndrome 90-95% of bile acid synthesis in humans, begins (IBS) or functional diarrhea by exclusion, thereby with 7α-hydroxylation of cholesterol catalyzed interfering with and delaying proper treatment. -

Malabsorption and Exocrine Pancreatic Insuffiecienty (Pi)
MALABSORPTION AND EXOCRINE PANCREATIC INSUFFIECIENTY (PI) Pancreatic Insufficiency is a condition in which a person does not have enough enzymes and bicarbonate being delivered from the pancreas to the intestine for digestion. This causes mal- absorption of nutrients, failure to gain weight and grow, weight loss, vitamin and mineral deficiency, and gastrointestinal symptoms. Most people with CF have mal-absorption due to PI. Onset usually occurs in the first one to two years of life, often in early infancy, but can start at anytime. Symptoms of mal-absorption -Change in number of stools -Large, bulky stools -Stools may be bulky and soft -Greasy, oily or floating stools, oil in toilet water -Stools may smell worse than usual or normal -Rectal prolapse -Mal-absorption of calorie providing nutrients and poor weight gain or weight loss Fat …………………………………………….9 calories/gram Protein………………………………..…….4 calories/gram Complex Carbohydrate ……………..4 calories/gram -Results in poor weight gain, weight loss, poor growth, decreased immune function and decreased lung health. -Mal-absorption of FAT SOLUBLE VITAMIN and deficiency: Vitamin A, Vitamin D, Vitamin E, Vitamin K -Mineral deficiencies: Calcium, Zinc, Sodium, Chloride Learn more about vitamins and minerals at: http://www.cff.org/treatments/Therapies/Nutrition/Vitamins/ Tests to Diagnose PI and Mal-absorption -72 hr fecal fat test -Pancreatic Fecal Elastase Treatment of PI and Mal-absorption Pancreatic Enzyme Replacement Therapy (PERT) Pancreatic enzymes are taken with each meal, snack, breast feed, bottle , and drink that contains fat protein and or complex carbohydrate. Antacid and acid blocking medicines can be added to make enzymes work better Fat Soluble Vitamin Supplementation with special supplements made for mal-absorption are prescribed Each enzyme company offers programs that provide free nutritional support and/or CF therapy support High Calorie, high protein diet Even with PERT, not all calories and nutrients from food are absorbed as expected and calories and nutrients are lost and need replacement. -

Digestive Health Center Nutrition Services Nutrition Guidelines for Chronic Pancreatitis Patient Education
Digestive Health Center Nutrition Services Nutrition Guidelines for Chronic Pancreatitis Patient Education The pancreas is an organ that: Produces pancreatic enzymes to help digest (break down) food in the small intestine for absorption Makes hormones (such as insulin) to help control blood sugars Chronic pancreatitis is ongoing inflammation of the pancreas. Symptoms can be worse after eating. Symptoms include: Abdominal pain Nausea Vomiting Weight loss Fatty stools (stools may also float and/or have a foul odor) Malabsorption of nutrients can occur from poor digestion of food (due to reduced pancreatic enzyme activity), which will result in nutrients passing into the stools. This is seen especially with fat and fat soluble vitamins (A, D, E) as digestion of fat is highly dependent on pancreatic enzymes. In some cases, diabetes can develop if the pancreas is not able to make enough insulin to help control blood sugars, so blood sugars stay high. Nutritional Guidelines Follow a low fat diet, which for chronic pancreatitis is often restricted to 50 grams of fat, but could also range between 30-50 grams of fat depending on tolerance. If you have diabetes, eat recommended serving sizes of low fat carbohydrates to help control blood sugars (low fat/non fat dairy, fruits, vegetables, whole grains, beans, lentils etc). Information on serving sizes is available. Take pancreatic enzymes as prescribed by your doctor to treat malabsorption. Take the enzymes before each meal and snack. They will not work if taken at the end of the meal. 1 Low Fat Diet Tips Eat 4-6 small meals throughout the day Spread out your fat intake throughout the day Use butter, margarine and cooking oils sparingly Bake, grill, roast and/or steam foods. -

Nutrition Management in the Adult Patient with Crohn's Disease
Review Article: Nutrition management in the adult patient with Crohn’s disease Nutrition management in the adult patient with Crohn’s disease Basson A, MS RD(USA)(SA) Lecturer and Hospital Student Internship Supervisor, University of the Western Cape Correspondence to: Abigail Basson, email: [email protected] Keywords: inflammatory bowel disease, nutrition therapy, Crohn’s disease Abstract Malnutrition, nutrient deficiencies and osteoporosis are common in patients with Crohn’s disease, regardless of disease activity. While the role of diet in the pathogenesis of the disease remains inconclusive, upon diagnosis, nutrition therapy plays an integral role in patient care. Successful nutrition intervention involves appropriate nutritional assessment, supplemental nutrition and individualised counselling and support. Peer reviewed. (Submitted: 2012-05-08. Accepted: 2012-11-04.) © SAJCN S Afr J Clin Nutr 2012;25(4):164-172 Introduction Low-fibre, high-fat and high-sugar intakes have been implicated as some of the environmental triggers in disease development, Crohn’s disease (CD) is a chronic and recurrent immune-mediated although the role of a pre-illness diet in the pathogenesis of CD inflammatory disorder of the gastrointestinal tract.1,2 Typically, pa- remains inconclusive.16-18 However, upon diagnosis, nutrition therapy tients suffer from chronic intestinal inflammation that follows a plays an integral role in patient care, regardless of disea se activity. relapse-remitting pattern, as well as from a variety of complications 3,4 (Table I) that may or may not involve the gut. Disease activity can Malnutrition be classified by the Crohn’s Disease Activity Index5 (CDAI) (Table II), and usually, treatment includes various combinations of corticoste- Weight loss, low body mass index (BMI) and nutrient deficiencies roid, anti-inflammatory (aminosalicylates), immune-modulating or have been well documented in patients with CD, especially during biological therapy.4 While the exact cause of CD is not known, it is active disease. -
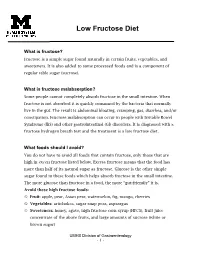
Low Fructose Diet
Low Fructose Diet What is fructose? Fructose is a simple sugar found naturally in certain fruits, vegetables, and sweeteners. It is also added to some processed foods and is a component of regular table sugar (sucrose). What is fructose malabsorption? Some people cannot completely absorb fructose in the small intestine. When fructose is not absorbed it is quickly consumed by the bacteria that normally live in the gut. The result is abdominal bloating, cramping, gas, diarrhea, and/or constipation. Fructose malabsorption can occur in people with Irritable Bowel Syndrome (IBS) and other gastrointestinal (GI) disorders. It is diagnosed with a fructose hydrogen breath test and the treatment is a low fructose diet. What foods should I avoid? You do not have to avoid all foods that contain fructose, only those that are high in excess fructose listed below. Excess fructose means that the food has more than half of its natural sugar as fructose. Glucose is the other simple sugar found in these foods which helps absorb fructose in the small intestine. The more glucose than fructose in a food, the more “gut-friendly” it is. Avoid these high fructose foods: Fruit: apple, pear, Asian pear, watermelon, fig, mango, cherries Vegetables: artichokes, sugar snap peas, asparagus Sweeteners: honey, agave, high fructose corn syrup (HFCS), fruit juice concentrate of the above fruits, and large amounts of sucrose (white or brown sugar) UMHS Division of Gastroenterology - 1 - Beverages: juices of the fruit listed above, regular soda and drinks that are sweetened with fructose or HFCS, rum General guidelines: Read labels and avoid products that contain fructose, crystalline fructose, HFCS, honey, agave, and fruit juice concentrates (i.e. -
University of Cincinnati
UNIVERSITY OF CINCINNATI Date:___________________ I, _________________________________________________________, hereby submit this work as part of the requirements for the degree of: in: It is entitled: This work and its defense approved by: Chair: _______________________________ _______________________________ _______________________________ _______________________________ _______________________________ Prevalence of Subclinical Vitamin K Deficiency in Cholestatic Liver Disease A thesis submitted to the Division of Research and Advanced Studies of the University of Cincinnati In partial fulfillment of the Requirements for the degree of MASTER OF SCIENCE In the Division of Epidemiology and Biostatistics, Department of Environmental Health of the College of Medicine 2004 by Jennifer A. Strople, M.D. B.A., University of Virginia, 1994 M.D., University of Alabama at Birmingham School of Medicine, 1998 Thesis committee: James E. Heubi, M.D. (Chair and Advisor) Paul Succop, Ph.D. Abstract Current practice is to monitor prothrombin time as an indicator of vitamin K sufficiency in cholestatic liver disease. Since prothrombin time is a surrogate marker, it may underestimate the actual prevalence of vitamin K deficiency in this population. This study investigates the frequency of vitamin K deficiency among a convenience sample of children and adults with cholestatic liver disease by determining plasma levels of protein induced in vitamin K absence II (PIVKA-II), and assesses the relationship between PIVKA-II levels and markers of cholestasis, measured prothrombin time, and vitamin A, E and 25-hydroxyvitamin D levels. Methods: Subjects with cholestatic liver disease were recruited from the Cincinnati referral area. Subjects with decompensated cirrhosis, malignancy, concurrent disease that results in fat malabsorption and AIDS were excluded. All subjects had blood collected for liver function tests, prothrombin time (PT), INR, bile acids, 25-hydroxyvitamin D, vitamin A, vitamin E and PIVKA-II levels. -

Chronic Pancreatitis: Introduction
Chronic Pancreatitis: Introduction Authors: Anthony N. Kalloo, MD; Lynn Norwitz, BS; Charles J. Yeo, MD Chronic pancreatitis is a relatively rare disorder occurring in about 20 per 100,000 population. The disease is progressive with persistent inflammation leading to damage and/or destruction of the pancreas . Endocrine and exocrine functional impairment results from the irreversible pancreatic injury. The pancreas is located deep in the retroperitoneal space of the upper part of the abdomen (Figure 1). It is almost completely covered by the stomach and duodenum . This elongated gland (12–20 cm in the adult) has a lobe-like structure. Variation in shape and exact body location is common. In most people, the larger part of the gland's head is located to the right of the spine or directly over the spinal column and extends to the spleen . The pancreas has both exocrine and endocrine functions. In its exocrine capacity, the acinar cells produce digestive juices, which are secreted into the intestine and are essential in the breakdown and metabolism of proteins, fats and carbohydrates. In its endocrine function capacity, the pancreas also produces insulin and glucagon , which are secreted into the blood to regulate glucose levels. Figure 1. Location of the pancreas in the body. What is Chronic Pancreatitis? Chronic pancreatitis is characterized by inflammatory changes of the pancreas involving some or all of the following: fibrosis, calcification, pancreatic ductal inflammation, and pancreatic stone formation (Figure 2). Although autopsies indicate that there is a 0.5–5% incidence of pancreatitis, the true prevalence is unknown. In recent years, there have been several attempts to classify chronic pancreatitis, but these have met with difficulty for several reasons. -

Nutritional Intervention for IBS Bette Bischoff, Fourth Year Medical Student, University of Kansas Medical Center
Nutritional Intervention for IBS Bette Bischoff, Fourth Year Medical Student, University of Kansas Medical Center Background Prior to medical school when I was a practicing dietician, I had the privilege of working with many patients who had irritable bowel syndrome (IBS). I found the subject of nutritional intervention related to IBS to be very rewarding and often challenging because there is no “perfect” diet for this syndrome. In light of the different etiologies potentially at work in each patient with IBS, nutrition therapy should be carefully and thoughtfully tailored to each person. This can be likened to times past when a cobbler hand-made each person’s shoes. Since each IBS patient can differ dramatically, careful documentation of exacerbating factors listed in the IBS diary maintained by patients may yield important clues to an effective approach to diet and nutrition. One of the issues is that patients with IBS may have a lower threshold to stressors compared to people without IBS. An example of this is patients with carbohydrate intolerances as well as a diagnosis of IBS, who experience an even greater response to problematic carbohydrates such as lactose or fructose as compared to someone who does not have IBS. Another important issue is being alert to unnecessary food aversions. Individuals may experience abdominal discomfort and associate this with eating a certain food, so they decide to avoid eating that particular item, even for life. This may lead to excessive food restriction and the potential for a full-blown eating disorder. What must be kept in mind is that IBS is characterized by increased gut and central nervous system (CNS) reactivity to stressors, and that these stressors can include any dietary excesses as well as sensitivities to particular foods that are unique to the individual rather than to the IBS condition. -

Intestinal Damage in Rotavirus and Adenovirus Gastroenteritis Assessed by D-Xylose Malabsorption
Arch Dis Child: first published as 10.1136/adc.52.7.589 on 1 July 1977. Downloaded from Short reports 589 ment of pneumonia in this condition. (1) Spasms and necropsies) formed the basis of a pathological study. convulsions, the main signs of tetanus, both cause Pulmonary pathology was found in 46 out of the contraction of the stomach, resulting in aspiration 54 necropsies: mainly pulmonary haemorrhage, pneumonia. (2) Apnoea, the direct effect of tetanus aspiration pneumonia, and bronchopneumonia, toxin upon respiratory centres. Though most drugs particularly of the right upper lobe. Adrenal used for sedation in tetanus cause respiratory haemorrhage and renal vein thrombosis also depression, so that shallow respirations might occurred. contribute to pulmonary collapse and secondary infection, we see bronchopneumonia predominantly I am indebted to Professor R. G. Hendrickse and among convulsing infants. Dr. P. Barns for criticism; to Mrs. N. Shiva and To detect this severe and common complication, Dr. A. Najafian for their encouragement; and to Dr. any clue would be valuable. Cough is rarely seen in F. Rafat who performed the necropsies. The study the heavily sedated infant, and lung signs are hard was supported by a grant from the Ministry of to detect as tetanic manifestations tend to obscure Science and Higher Education of Iran. them. Feeble respiratory movements, cyanosis, hypothermia, sudden loss of tetanic signs, and/or a References drop in the amount of sedation required, have Adams, E. B., Laurence, D. R., and Smith, J. W. G. (1969). proved to be the best indications of developing Tetanus, p. 89. Blackwell, Oxford. -

Irritable Bowel Syndrome: a Global Perspective
World Gastroenterology Organisation Global Guidelines Irritable Bowel Syndrome: a Global Perspective Update September 2015 Review team Eamonn M.M. Quigley USA (Chair) Michael Fried Switzerland Kok-Ann Gwee Singapore Igor Khalif Russia Pali Hungin United Kingdom Greger Lindberg Sweden Zaigham Abbas Pakistan Luis Bustos Fernandez Argentina Shobna J. Bhatia India Max Schmulson Mexico Carolina Olano Uruguay Anton Le Mair The Netherlands WGO Global Guidelines IBS 2 Contents 1 WGO cascades 3 1.1 Cascade options for resource-sensitive IBS diagnosis 3 1.2 Cascade options for resource-sensitive IBS management 4 2 Introduction 5 2.1 IBS subclassification 6 2.2 Global prevalence and incidence 7 2.3 Other observations on IBS epidemiology 7 2.4 IBS demographics, East/West differences in presenting features 8 3 Diagnosis of IBS 8 3.1 Clinical history 8 3.2 Psychological assessment 10 3.3 Physical examination 11 3.4 IBS diagnostic algorithm 11 4 Evaluation of IBS 11 4.1 Diagnostic criteria (Rome III) 12 4.2 Additional tests or investigatations 13 4.3 Differential diagnosis 13 4.4 Comorbidity with other diseases 17 5 Management of IBS 17 5.1 Introduction 17 5.2 Diet 19 5.3 Drug therapy 20 5.4 Psychological and other treatments 23 5.5 Prognosis 24 5.6 Follow-up 25 6 Appendix: useful resources 25 References 26 Figures Fig. 1 Algorithm for diagnosing irritable bowel syndrome (IBS) 11 Fig. 2 Management of patients with symptoms of irritable bowel syndrome 18 Tables Table 1 Rome III criteria for diagnosing IBS 12 © World Gastroenterology Organization, 2015 WGO Global Guidelines IBS 3 1 WGO cascades With this guideline, the World Gastroenterology Organisation (WGO) is aiming to guide health providers in the best management of irritable bowel disease (IBS) through a concise document with recommendations based on the latest evidence and resulting from our global expert consensus process based on best current practice. -

The Pathology of Malabsorption: Current Concepts
Histopathology 2007, 50, 64–82. DOI: 10.1111/j.1365-2559.2006.02547.x REVIEW The pathology of malabsorption: current concepts S R Owens & J K Greenson1 Departments of Pathology, University of Pittsburgh Medical Center, Pittsburgh, PA and 1University of Michigan Health System, Ann Arbor, MI, USA Owens S R & Greenson J K (2007) Histopathology 50, 64–82 The pathology of malabsorption: current concepts Intestinal malabsorption results from a wide variety of such as systemic sclerosis. Finally, microbial causes of causes, which can most easily be organized into three malabsorption include bacterial overgrowth, Whipple’s groups. Maldigestion arises from problems with mix- disease, and numerous infections or infestations that ing or with digestive mediators, and includes post- are most frequently seen in immunocompromised gastrectomy patients and those with deficiencies of patients. An overview of the most common and pancreatic or intestinal enzymes, or of bile salts. interesting entities in each of these categories follows, Mucosal and mural causes of malabsorption are along with a discussion of current concepts. Mucosal abundant, and include gluten-sensitive enteropathy, conditions and microbial causes of malabsorption are tropical sprue, autoimmune enteropathy, and HIV/ given special attention. AIDS-related enteropathy, as well as mural conditions Keywords: autoimmune enteropathy, bacterial overgrowth, coeliac disease, giardiasis, gluten-sensitive enteropathy, malabsorption, sprue, Whipple’s disease Abbreviations: AE, autoimmune enteropathy;