Irritable Bowel Syndrome (IBS): Introduction
Total Page:16
File Type:pdf, Size:1020Kb
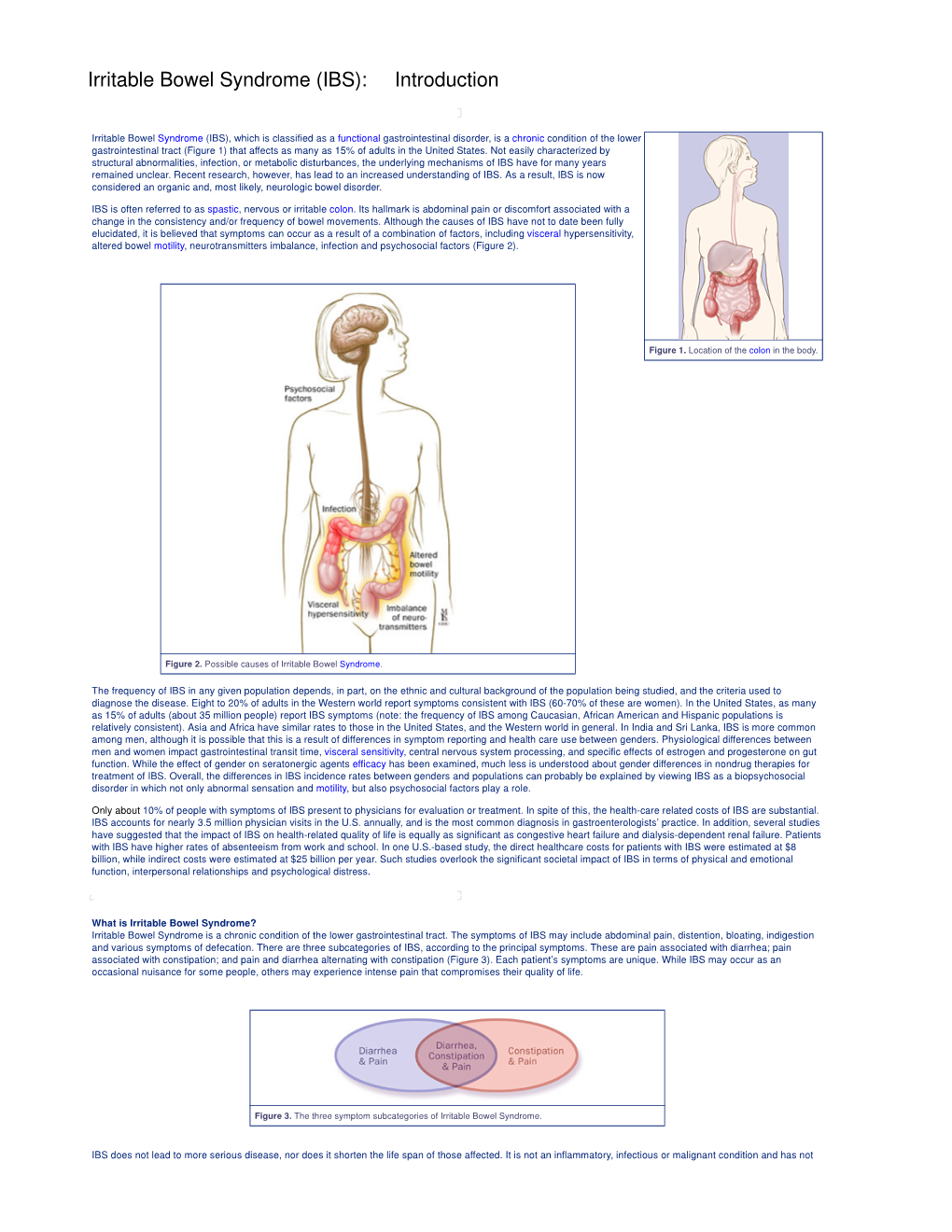
Load more
Recommended publications
-

Print This Article
International Surgery Journal Lew D et al. Int Surg J. 2021 May;8(5):1575-1578 http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902 DOI: https://dx.doi.org/10.18203/2349-2902.isj20211831 Case Report Acute gangrenous appendicitis and acute gangrenous cholecystitis in a pregnant patient, a difficult diagnosis: a case report David Lew, Jane Tian*, Martine A. Louis, Darshak Shah Department of Surgery, Flushing Hospital Medical Center, Flushing, New York, USA Received: 26 February 2021 Accepted: 02 April 2021 *Correspondence: Dr. Jane Tian, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Abdominal pain is a common complaint in pregnancy, especially given the physiological and anatomical changes that occur as the pregnancy progresses. The diagnosis and treatment of common surgical pathologies can therefore be difficult and limited by the special considerations for the fetus. While uncommon in the general population, concurrent or subsequent disease processes should be considered in the pregnant patient. We present the case of a 36 year old, 13 weeks pregnant female who presented with both acute appendicitis and acute cholecystitis. Keywords: Appendicitis, Cholecystitis, Pregnancy, Pregnant INTRODUCTION population is rare.5 Here we report a case of concurrent appendicitis and cholecystitis in a pregnant woman. General surgeons are often called to evaluate patients with abdominal pain. The differential diagnosis list must CASE REPORT be expanded in pregnant woman and the approach to diagnosing and treating certain diseases must also be A 36 year old, 13 weeks pregnant female (G2P1001) adjusted to prevent harm to the fetus. -

Adult Congenital Megacolon with Acute Fecal Obstruction and Diabetic Nephropathy: a Case Report
2726 EXPERIMENTAL AND THERAPEUTIC MEDICINE 18: 2726-2730, 2019 Adult congenital megacolon with acute fecal obstruction and diabetic nephropathy: A case report MINGYUAN ZHANG1,2 and KEFENG DING1 1Colorectal Surgery Department, Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, Zhejiang 310000; 2Department of Gastrointestinal Surgery, Yinzhou Peoples' Hospital, Ningbo, Zhejiang 315000, P.R. China Received November 27, 2018; Accepted June 20, 2019 DOI: 10.3892/etm.2019.7852 Abstract. Megacolon is a congenital disorder. Adult congen- sufficient amount of bowel should be removed, particularly the ital megacolon (ACM), also known as adult Hirschsprung's aganglionic segment (2). The present study reports on a case of disease, is rare and frequently manifests as constipation. ACM a 56-year-old patient with ACM, fecal impaction and diabetic is caused by the absence of ganglion cells in the submucosa nephropathy. or myenteric plexus of the bowel. Most patients undergo treat- ment of megacolon at a young age, but certain patients cannot Case report be treated until they develop bowel obstruction in adulthood. Bowel obstruction in adults always occurs in complex clinical A 56-year-old male patient with a history of chronic constipa- situations and it is frequently combined with comorbidities, tion presented to the emergency department of Yinzhou including bowel tumors, volvulus, hernias, hypertension or Peoples' Hospital (Ningbo, China) in February 2018. The diabetes mellitus. Surgical intervention is always required in patient had experienced vague abdominal distention for such cases. To avoid recurrence, a sufficient amount of bowel several days. Prior to admission, chronic bowel obstruction should be removed, particularly the aganglionic segment. -

Intestinal Obstruction
Intestinal obstruction Prof. Marek Jackowski Definition • Any condition interferes with normal propulsion and passage of intestinal contents. • Can involve the small bowel, colon or both small and colon as in generalized ileus. Definitions 5% of all acute surgical admissions Patients are often extremely ill requiring prompt assessment, resuscitation and intensive monitoring Obstruction a mechanical blockage arising from a structural abnormality that presents a physical barrier to the progression of gut contents. Ileus a paralytic or functional variety of obstruction Obstruction: Partial or complete Simple or strangulated Epidemiology 1 % of all hospitalization 3-5 % of emergency surgical admissions More frequent in female patients - gynecological and pelvic surgical operations are important etiologies for postop. adhesions Adhesion is the most common cause of intestinal obstruction 80% of bowel obstruction due to small bowel obstruction - the most common causes are: - Adhesion - Hernia - Neoplasm 20% due to colon obstruction - the most common cause: - CR-cancer 60-70%, - diverticular disease and volvulus - 30% Mortality rate range between 3% for simple bowel obstruction to 30% when there is strangulation or perforation Recurrent rate vary according to method of treatment ; - conservative 12% - surgical treatment 8-32% Classification • Cause of obstruction: mechanical or functional. • Duration of obstruction: acute or chronic. • Extent of obstruction: partial or complete • Type of obstruction: simple or complex (closed loop and strangulation). CLASSIFICATION DYNAMIC ADYNAMIC (MECHANICAL) (FUNCTIONAL) Peristalsis is Result from atony of working against a the intestine with loss mechanical of normal peristalsis, obstruction in the absence of a mechanical cause. or it may be present in a non-propulsive form (e.g. mesenteric vascular occlusion or pseudo-obstruction) Etiology Mechanical bowel obstruction: A. -

Inflammatory Bowel Disease Irritable Bowel Syndrome
Inflammatory Bowel Disease and Irritable Bowel Syndrome Similarities and Differences 2 www.ccfa.org IBD Help Center: 888.MY.GUT.PAIN 888.694.8872 Important Differences Between IBD and IBS Many diseases and conditions can affect the gastrointestinal (GI) tract, which is part of the digestive system and includes the esophagus, stomach, small intestine and large intestine. These diseases and conditions include inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). IBD Help Center: 888.MY.GUT.PAIN 888.694.8872 www.ccfa.org 3 Inflammatory bowel diseases are a group of inflammatory conditions in which the body’s own immune system attacks parts of the digestive system. Inflammatory Bowel Disease Inflammatory bowel diseases are a group of inflamma- Causes tory conditions in which the body’s own immune system attacks parts of the digestive system. The two most com- The exact cause of IBD remains unknown. Researchers mon inflammatory bowel diseases are Crohn’s disease believe that a combination of four factors lead to IBD: a (CD) and ulcerative colitis (UC). IBD affects as many as 1.4 genetic component, an environmental trigger, an imbal- million Americans, most of whom are diagnosed before ance of intestinal bacteria and an inappropriate reaction age 35. There is no cure for IBD but there are treatments to from the immune system. Immune cells normally protect reduce and control the symptoms of the disease. the body from infection, but in people with IBD, the immune system mistakes harmless substances in the CD and UC cause chronic inflammation of the GI tract. CD intestine for foreign substances and launches an attack, can affect any part of the GI tract, but frequently affects the resulting in inflammation. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

FDA Warns About an Increased Risk of Serious Pancreatitis with Irritable Bowel Drug Viberzi (Eluxadoline) in Patients Without a Gallbladder
FDA warns about an increased risk of serious pancreatitis with irritable bowel drug Viberzi (eluxadoline) in patients without a gallbladder Safety Announcement [03-15-2017] The U.S. Food and Drug Administration (FDA) is warning that Viberzi (eluxadoline), a medicine used to treat irritable bowel syndrome with diarrhea (IBS-D), should not be used in patients who do not have a gallbladder. An FDA review found these patients have an increased risk of developing serious pancreatitis that could result in hospitalization or death. Pancreatitis may be caused by spasm of a certain digestive system muscle in the small intestine. As a result, we are working with the Viberzi manufacturer, Allergan, to address these safety concerns. Patients should talk to your health care professional about how to control your symptoms of irritable bowel syndrome with diarrhea (IBS-D), particularly if you do not have a gallbladder. The gallbladder is an organ that stores bile, one of the body’s digestive juices that helps in the digestion of fat. Stop taking Viberzi right away and get emergency medical care if you develop new or worsening stomach-area or abdomen pain, or pain in the upper right side of your stomach-area or abdomen that may move to your back or shoulder. This pain may occur with nausea and vomiting. These may be symptoms of pancreatitis, an inflammation of the pancreas, an organ important in digestion; or spasm of the sphincter of Oddi, a muscular valve in the small intestine that controls the flow of digestive juices to the gut. Health care professionals should not prescribe Viberzi in patients who do not have a gallbladder and should consider alternative treatment options in these patients. -

Therapeutic Class Overview Irritable Bowel Syndrome Agents
Therapeutic Class Overview Irritable Bowel Syndrome Agents Therapeutic Class Overview/Summary: This review will focus on agents used for the treatment of Irritable Bowel Syndrome (IBS).1-5 IBS is a gastrointestinal syndrome characterized primarily by non-specific chronic abdominal pain, usually described as a cramp-like sensation, and abnormal bowel habits, either constipation or diarrhea, in which there is no organic cause. Other common gastrointestinal symptoms may include gastroesophageal reflux, dysphagia, early satiety, intermittent dyspepsia and nausea. Patients may also experience a wide range of non-gastrointestinal symptoms. Some notable examples include sexual dysfunction, dysmenorrhea, dyspareunia, increased urinary frequency/urgency and fibromyalgia-like symptoms.6 IBS is defined by one of four subtypes. IBS with constipation (IBS-C) is the presence of hard or lumpy stools with ≥25% of bowel movements and loose or watery stools with <25% of bowel movements. When IBS is associated with diarrhea (IBS-D) loose or watery stools are present with ≥25% of bowel movements and hard or lumpy stools are present with <25% of bowel movements. Mixed IBS (IBS-M) is defined as the presence of hard or lumpy stools with ≥25% and loose or water stools with ≥25% of bowel movements. Final subtype, or unsubtyped, is all other cases of IBS that do not fall into the other classes. Pharmacological therapy for IBS depends on subtype.7 While several over-the-counter or off-label prescription agents are used for the treatment of IBS, there are currently only two agents approved by the Food and Drug Administration (FDA) for the treatment of IBS-C and three agents approved by the FDA for IBS-D. -

Diagnostic Approach to Chronic Constipation in Adults NAMIRAH JAMSHED, MD; ZONE-EN LEE, MD; and KEVIN W
Diagnostic Approach to Chronic Constipation in Adults NAMIRAH JAMSHED, MD; ZONE-EN LEE, MD; and KEVIN W. OLDEN, MD Washington Hospital Center, Washington, District of Columbia Constipation is traditionally defined as three or fewer bowel movements per week. Risk factors for constipation include female sex, older age, inactivity, low caloric intake, low-fiber diet, low income, low educational level, and taking a large number of medications. Chronic constipa- tion is classified as functional (primary) or secondary. Functional constipation can be divided into normal transit, slow transit, or outlet constipation. Possible causes of secondary chronic constipation include medication use, as well as medical conditions, such as hypothyroidism or irritable bowel syndrome. Frail older patients may present with nonspecific symptoms of constipation, such as delirium, anorexia, and functional decline. The evaluation of constipa- tion includes a history and physical examination to rule out alarm signs and symptoms. These include evidence of bleeding, unintended weight loss, iron deficiency anemia, acute onset constipation in older patients, and rectal prolapse. Patients with one or more alarm signs or symptoms require prompt evaluation. Referral to a subspecialist for additional evaluation and diagnostic testing may be warranted. (Am Fam Physician. 2011;84(3):299-306. Copyright © 2011 American Academy of Family Physicians.) ▲ Patient information: onstipation is one of the most of 1,028 young adults, 52 percent defined A patient education common chronic gastrointes- constipation as straining, 44 percent as hard handout on constipation is 1,2 available at http://family tinal disorders in adults. In a stools, 32 percent as infrequent stools, and doctor.org/037.xml. -

Abdominal Pain - Gastroesophageal Reflux Disease
ACS/ASE Medical Student Core Curriculum Abdominal Pain - Gastroesophageal Reflux Disease ABDOMINAL PAIN - GASTROESOPHAGEAL REFLUX DISEASE Epidemiology and Pathophysiology Gastroesophageal reflux disease (GERD) is one of the most commonly encountered benign foregut disorders. Approximately 20-40% of adults in the United States experience chronic GERD symptoms, and these rates are rising rapidly. GERD is the most common gastrointestinal-related disorder that is managed in outpatient primary care clinics. GERD is defined as a condition which develops when stomach contents reflux into the esophagus causing bothersome symptoms and/or complications. Mechanical failure of the antireflux mechanism is considered the cause of GERD. Mechanical failure can be secondary to functional defects of the lower esophageal sphincter or anatomic defects that result from a hiatal or paraesophageal hernia. These defects can include widening of the diaphragmatic hiatus, disturbance of the angle of His, loss of the gastroesophageal flap valve, displacement of lower esophageal sphincter into the chest, and/or failure of the phrenoesophageal membrane. Symptoms, however, can be accentuated by a variety of factors including dietary habits, eating behaviors, obesity, pregnancy, medications, delayed gastric emptying, altered esophageal mucosal resistance, and/or impaired esophageal clearance. Signs and Symptoms Typical GERD symptoms include heartburn, regurgitation, dysphagia, excessive eructation, and epigastric pain. Patients can also present with extra-esophageal symptoms including cough, hoarse voice, sore throat, and/or globus. GERD can present with a wide spectrum of disease severity ranging from mild, intermittent symptoms to severe, daily symptoms with associated esophageal and/or airway damage. For example, severe GERD can contribute to shortness of breath, worsening asthma, and/or recurrent aspiration pneumonia. -

Acute Abdomen
Acute abdomen: Shaking down the Acute abdominal pain can be difficult to diagnose, requiring astute assessment skills and knowledge of abdominal anatomy 2.3 ANCC to discover its cause. We show you how to quickly and accurately CONTACT HOURS uncover the clues so your patient can get the help he needs. By Amy Wisniewski, BSN, RN, CCM Lehigh Valley Home Care • Allentown, Pa. The author has disclosed that she has no significant relationships with or financial interest in any commercial companies that pertain to this educational activity. NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 43 suspects Determining the cause of acute abdominal rapidly, indicating a life-threatening process, pain is often complex due to the many or- so fast and accurate assessment is essential. gans in the abdomen and the fact that pain In this article, I’ll describe how to assess a may be nonspecific. Acute abdomen is a patient with acute abdominal pain and inter- general diagnosis, typically referring to se- vene appropriately. vere abdominal pain that occurs suddenly over a short period (usually no longer than What a pain! 7 days) and often requires surgical interven- Acute abdominal pain is one of the top tion. Symptoms may be severe and progress three symptoms of patients presenting in www.NursingMadeIncrediblyEasy.com January/February 2010 Nursing made Incredibly Easy! 43 NIE0110_124_CEAbdomen.qxd:Deepak 26/11/09 9:38 AM Page 44 the ED. Reasons for acute abdominal pain Visceral pain can be divided into three Your patient’s fall into six broad categories: subtypes: age may give • inflammatory—may be a bacterial cause, • tension pain. -

Constipation
Constipation Caris Diagnostics Health Improvement Series What is constipation? Constipation means that a person has three bowel movements or fewer in a week. The stool is hard and dry. Sometimes it is painful to pass. You may feel‘draggy’and full. Some people think they should have a bowel movement every day. That is not really true. There is no‘right’number of bowel movements. Each person's body finds its own normal number of bowel movements. It depends on the food you eat, how much you exercise, and other things. At one time or another, almost everyone gets constipated. In most cases, it lasts for a short time and is not serious. When you understand what causes constipation, you can take steps to prevent it. What can I do about constipation? Changing what you 4. Allow yourself enough time to have a bowel movement. eat and drink and how much you exercise will help re- Sometimes we feel so hurried that we don't pay atten- lieve and prevent constipation. Here are some steps you tion to our body's needs. Make sure you don't ignore the can take. urge to have a bowel movement. 1. Eat more fiber. Fiber helps form soft, bulky stool. It 5. Use laxatives only if a doctor says you should. is found in many vegetables, fruits, and grains. Be sure Laxatives are medicines that will make you pass a stool. to add fiber a little at a time, so your body gets used to Most people who are mildly constipated do not need it slowly.