Ramelteon a Novel Hypnotic Lacking Abuse Liability and Sedative Adverse Effects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal of Pharmacology and Experimental Therapeutics
Journal of Pharmacology and Experimental Therapeutics Molecular Determinants of Ligand Selectivity for the Human Multidrug And Toxin Extrusion Proteins, MATE1 and MATE-2K Bethzaida Astorga, Sean Ekins, Mark Morales and Stephen H Wright Department of Physiology, University of Arizona, Tucson, AZ 85724, USA (B.A., M.M., and S.H.W.) Collaborations in Chemistry, 5616 Hilltop Needmore Road, Fuquay-Varina NC 27526, USA (S.E.) Supplemental Table 1. Compounds selected by the common features pharmacophore after searching a database of 2690 FDA approved compounds (www.collaborativedrug.com). FitValue Common Name Indication 3.93897 PYRIMETHAMINE Antimalarial 3.3167 naloxone Antidote Naloxone Hydrochloride 3.27622 DEXMEDETOMIDINE Anxiolytic 3.2407 Chlordantoin Antifungal 3.1776 NALORPHINE Antidote Nalorphine Hydrochloride 3.15108 Perfosfamide Antineoplastic 3.11759 Cinchonidine Sulfate Antimalarial Cinchonidine 3.10352 Cinchonine Sulfate Antimalarial Cinchonine 3.07469 METHOHEXITAL Anesthetic 3.06799 PROGUANIL Antimalarial PROGUANIL HYDROCHLORIDE 100MG 3.05018 TOPIRAMATE Anticonvulsant 3.04366 MIDODRINE Antihypotensive Midodrine Hydrochloride 2.98558 Chlorbetamide Antiamebic 2.98463 TRIMETHOPRIM Antibiotic Antibacterial 2.98457 ZILEUTON Antiinflammatory 2.94205 AMINOMETRADINE Diuretic 2.89284 SCOPOLAMINE Antispasmodic ScopolamineHydrobromide 2.88791 ARTICAINE Anesthetic 2.84534 RITODRINE Tocolytic 2.82357 MITOBRONITOL Antineoplastic Mitolactol 2.81033 LORAZEPAM Anxiolytic 2.74943 ETHOHEXADIOL Insecticide 2.64902 METHOXAMINE Antihypotensive Methoxamine -

Guaiana, G., Barbui, C., Caldwell, DM, Davies, SJC, Furukawa, TA
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Explore Bristol Research Guaiana, G., Barbui, C., Caldwell, D. M., Davies, S. J. C., Furukawa, T. A., Imai, H., ... Cipriani, A. (2017). Antidepressants, benzodiazepines and azapirones for panic disorder in adults: a network meta-analysis. Cochrane Database of Systematic Reviews, 2017(7), [CD012729]. https://doi.org/10.1002/14651858.CD012729 Publisher's PDF, also known as Version of record Link to published version (if available): 10.1002/14651858.CD012729 Link to publication record in Explore Bristol Research PDF-document This is the final published version of the article (version of record). It first appeared online via Cochrane Library at https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012729/full . Please refer to any applicable terms of use of the publisher. University of Bristol - Explore Bristol Research General rights This document is made available in accordance with publisher policies. Please cite only the published version using the reference above. Full terms of use are available: http://www.bristol.ac.uk/pure/about/ebr-terms Cochrane Database of Systematic Reviews Antidepressants, benzodiazepines and azapirones for panic disorder in adults: a network meta-analysis (Protocol) Guaiana G, Barbui C, Caldwell DM, Davies SJC, Furukawa TA, Imai H, Koesters M, Tajika A, Bighelli I, Pompoli A, Cipriani A Guaiana G, Barbui C, Caldwell DM, Davies SJC, Furukawa TA, Imai H, Koesters M, Tajika A, Bighelli I, Pompoli A, Cipriani A. Antidepressants, benzodiazepines and azapirones for panic disorder in adults: a network meta-analysis. Cochrane Database of Systematic Reviews 2017, Issue 7. -

GABA Receptors
D Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews • BIOTREND Reviews Review No.7 / 1-2011 GABA receptors Wolfgang Froestl , CNS & Chemistry Expert, AC Immune SA, PSE Building B - EPFL, CH-1015 Lausanne, Phone: +41 21 693 91 43, FAX: +41 21 693 91 20, E-mail: [email protected] GABA Activation of the GABA A receptor leads to an influx of chloride GABA ( -aminobutyric acid; Figure 1) is the most important and ions and to a hyperpolarization of the membrane. 16 subunits with γ most abundant inhibitory neurotransmitter in the mammalian molecular weights between 50 and 65 kD have been identified brain 1,2 , where it was first discovered in 1950 3-5 . It is a small achiral so far, 6 subunits, 3 subunits, 3 subunits, and the , , α β γ δ ε θ molecule with molecular weight of 103 g/mol and high water solu - and subunits 8,9 . π bility. At 25°C one gram of water can dissolve 1.3 grams of GABA. 2 Such a hydrophilic molecule (log P = -2.13, PSA = 63.3 Å ) cannot In the meantime all GABA A receptor binding sites have been eluci - cross the blood brain barrier. It is produced in the brain by decarb- dated in great detail. The GABA site is located at the interface oxylation of L-glutamic acid by the enzyme glutamic acid decarb- between and subunits. Benzodiazepines interact with subunit α β oxylase (GAD, EC 4.1.1.15). It is a neutral amino acid with pK = combinations ( ) ( ) , which is the most abundant combi - 1 α1 2 β2 2 γ2 4.23 and pK = 10.43. -

Neurobiological and Neurobehavioral Mechanisms of Chronic Alcohol Drinking
Neurobiological and Neurobehavioral Mechanisms of Chronic Alcohol Drinking Neurobiological and Neurobehavioral Mechanisms of Chronic Alcohol Drinking Alcoholism comprises a set of complex behaviors seeking behaviors, have been developed. These in which an individual becomes increasingly models, which remain an integral part of the preoccupied with obtaining alcohol. These study of alcoholism, include animals that pref- behaviors ultimately lead to a loss of control over erentially drink solutions containing alcohol, consumption of the drug and to the development animals that self-administer alcohol during of tolerance, dependence, and impaired social and withdrawal, animals with a history of dependence occupational functioning. that self-administer alcohol, and animals that self- administer alcohol after a period of abstinence Although valuable information regarding toler- from the drug. Genetic models for alcoholism ance and dependence has been, and continues to also exist and include animals that have been bred be, gathered through human studies, much of the selectively for high alcohol consumption. Studies detailed understanding of the impact of exposure using such models are uncovering the systemic, to alcohol on behavior and on the biological cellular, and molecular neurobiological mech- mechanisms underlying those behaviors has been anisms that appear to contribute to chronic obtained through the use of animal models for alcohol consumption. The challenge of current alcoholism and a variety of in vitro, or cellular, and future studies is to understand which specific systems. Through the use of cellular systems and cellular and subcellular systems undergo mole- animal models, researchers can control the genetic cular changes to influence tolerance and depen- background and experimental conditions under dence in motivational systems that lead to which a specific alcohol-related behavior or chronic drinking. -

Alprazolam Dependence Prevented by Substituting with the ß-Carboline
Proc. Natl. Acad. Sci. USA Vol. 94, pp. 2719–2723, March 1997 Pharmacology Alprazolam dependence prevented by substituting with the b-carboline abecarnil (benzodiazepinesywithdrawalytoleranceyreplacement therapy) GRAZIANO PINNA*, RUGGERO GALICI*, HERBERT H. SCHNEIDER,DAVID N. STEPHENS†, AND LECHOSLAW TURSKI‡ Research Laboratories of Schering AG, Mu¨llerstrasse 178, D-13342 Berlin, Germany Communicated by Jan Bures, Czech Academy of Sciences, Prague, Czech Republic, December 26, 1996 (received for review December 2, 1996) ABSTRACT Abrupt termination of the treatment of hu- although this view is not adequately supported by controlled mans with benzodiazepines (BDZs) leads to a rapid onset of human data (5). There are also no adequately controlled discontinuation syndrome characterized by anxiety, muscle animal experimental data that allow comparison of the risk of spasms, and occasionally convulsions. For this reason, it is producing dependence between BDZs with short and long recommended in clinical practice to reduce the dose of the half-lives (7). Similarly, there is scanty experimental data BDZs gradually at the end of treatment. Nevertheless, many demonstrating how to discontinue safely treatment with BDZs clinicians report signs of dependence even during gradual with short half-lives. reduction of doses (tapering) of the BDZs in a large propor- To address this issue we have employed newly developed tion of patients. Thus, there is considerable interest in dis- methods for electroencephalographic (EEG) monitoring of covering means of weaning patients away from BDZs without seizures, for electromyographic (EMG) monitoring of muscle the risk of discontinuation syndrome. In the present study, tone, and for detecting anxiety-like behavioral changes after mice withdrawn from chronic treatment with alprazolam discontinuation of long-term treatment with sedative drugs in showed anxiety, muscle rigidity, and seizures between days 1 mice (8) for controlled and standardized assessment of de- and 28 after termination of the treatment. -

Abecarnil/Allobarbital 959 Pharmacopoeias
Abecarnil/Allobarbital 959 Pharmacopoeias. In Eur. (see p.vii). acamprosate’s action including inhibition of neuronal hyper- maleate in the treatment of anxiety disorders, hiccups, and nau- Ph. Eur. 6.2 (Acamprosate Calcium). A white or almost white excitability by antagonising excitatory amino acids such as sea and vomiting. Acepromazine, as the base, has also been giv- powder. Freely soluble in water; practically insoluble in alcohol glutamate. en in preparations for the management of insomnia. and in dichloromethane. A 5% solution in water has a pH of 5.5 1. Wilde MI, Wagstaff AJ. Acamprosate: a review of its pharmacol- Preparations to 7.0. ogy and clinical potential in the management of alcohol depend- ence after detoxification. Drugs 1997; 53: 1038–53. Proprietary Preparations (details are given in Part 3) Adverse Effects 2. Anonymous. Acamprosate for alcohol dependence? Drug Ther Denm.: Plegicil; Turk.: Plegicil. The main adverse effect of acamprosate is dosage-related diar- Bull 1997; 35: 70–2. Multi-ingredient: Fr.: Noctran. rhoea; nausea, vomiting, and abdominal pain occur less frequent- 3. Mason BJ. Treatment of alcohol-dependent outpatients with acamprosate: a clinical review. J Clin Psychiatry 2001; 62 (suppl ly. Other adverse effects have included pruritus, and occasionally 20): 42–8. a maculopapular rash; bullous skin reactions have occurred rare- 4. Overman GP, et al. Acamprosate for the adjunctive treatment of Aceprometazine (rINN) ly. Depression and fluctuations in libido have also been reported. alcohol dependence. Ann Pharmacother 2003; 37: 1090–9. Hypersensitivity reactions including urticaria, angioedema, and 5. Anton RF, et al. Combined pharmacotherapies and behavioral 16-64 CB; Aceprometazina; Acéprométazine; Aceprometazi- anaphylaxis have been reported very rarely. -

WO 2015/072852 Al 21 May 2015 (21.05.2015) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2015/072852 Al 21 May 2015 (21.05.2015) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 36/84 (2006.01) A61K 31/5513 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 31/045 (2006.01) A61P 31/22 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/522 (2006.01) A61K 45/06 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, PCT/NL20 14/050780 KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (22) International Filing Date: MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, 13 November 2014 (13.1 1.2014) PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, (25) Filing Language: English TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (26) Publication Language: English (84) Designated States (unless otherwise indicated, for every (30) Priority Data: kind of regional protection available): ARIPO (BW, GH, 61/903,430 13 November 2013 (13. 11.2013) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, (71) Applicant: RJG DEVELOPMENTS B.V. -

CNS Drug Reviews Vol
CNS Drug Reviews Vol. 10, No. 1, pp. 45–76 © 2004 Neva Press, Branford, Connecticut Clinical Pharmacology, Clinical Efficacy, and Behavioral Toxicity of Alprazolam: A Review of the Literature Joris C. Verster and Edmund R. Volkerts Utrecht Institute for Pharmaceutical Sciences, Department of Psychopharmacology, University of Utrecht, Utrecht, The Netherlands Keywords: Alprazolam — Benzodiazepines — Anxiety — Depression — Panic — Sedation. ABSTRACT Alprazolam is a benzodiazepine derivative that is currently used in the treatment of generalized anxiety, panic attacks with or without agoraphobia, and depression. Alprazo- lam has a fast onset of symptom relief (within the first week); it is unlikely to produce de- pendency or abuse. No tolerance to its therapeutic effect has been reported. At discontinu- ation of alprazolam treatment, withdrawal and rebound symptoms are common. Hence, alprazolam discontinuation must be tapered. An exhaustive review of the literature showed that alprazolam is significantly superior to placebo, and is at least equally effective in the relief of symptoms as tricyclic antide- pressants (TCAs), such as imipramine. However, although alprazolam and imipramine are significantly more effective than placebo in the treatment of panic attacks, Selective Sero- tonin Reuptake Inhibitors (SSRIs) appear to be superior to either of the two drugs. Therefore, alprazolam is recommended as a second line treatment option, when SSRIs are not effective or well tolerated. In addition to its therapeutic effects, alprazolam produces adverse effects, such as drowsiness and sedation. Since alprazolam is widely used, many clinical studies investi- gated its cognitive and psychomotor effects. It is evident from these studies that alprazo- lam may impair performance in a variety of skills in healthy volunteers as well as in pa- tients. -

Paper Clip—High Risk Medications
You belong. PAPER CLIP—HIGH RISK MEDICATIONS Description: Some medications may be risky for people over 65 years of age and there may be safer drug choices to treat some conditions. It is recommended that medications are reviewed regularly with your providers/prescriber to ensure patient safety. Condition Treated Current Medication(s)-High Risk Safer Alternatives to Consider Urinary Tract Infections (UTIs), Nitrofurantoin Bactrim (sulfamethoxazole/trimethoprim) or recurrent UTIs, or Prophylaxis (Macrobid, or Macrodantin) Trimpex/Proloprim/Primsol (trimethoprim) Allergies Hydroxyzine (Vistaril, Atarax) Xyzal (Levocetirizine) Anxiety Hydroxyzine (Vistaril, Atarax) Buspar (Buspirone), Paxil (Paroxetine), Effexor (Venlafaxine) Parkinson’s Hydroxyzine (Vistaril, Atarax) Symmetrel (Amantadine), Sinemet (Carbidopa/levodopa), Selegiline (Eldepryl) Motion Sickness Hydroxyzine (Vistaril, Atarax) Antivert (Meclizine) Nausea & Vomiting Hydroxyzine (Vistaril, Atarax) Zofran (Ondansetron) Insomnia Hydroxyzine (Vistaril, Atarax) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Eszopiclone (Lunesta) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Zolpidem (Ambien) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Zaleplon (Sonata) Ramelteon (Rozerem), Doxepin (Silenor) Muscle Relaxants Cyclobenazprine (Flexeril, Amrix) NSAIDs (Ibuprofen, naproxen) or Hydrocodone Codeine Tramadol (Ultram) Baclofen (Lioresal) Tizanidine (Zanaflex) Migraine Prophylaxis Elavil (Amitriptyline) Propranolol (Inderal), Timolol (Blocadren), Topiramate (Topamax), -

Molecular Mechanisms of Antiseizure Drug Activity at GABAA Receptors
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Seizure 22 (2013) 589–600 Contents lists available at SciVerse ScienceDirect Seizure jou rnal homepage: www.elsevier.com/locate/yseiz Review Molecular mechanisms of antiseizure drug activity at GABAA receptors L. John Greenfield Jr.* Dept. of Neurology, University of Arkansas for Medical Sciences, 4301W. Markham St., Slot 500, Little Rock, AR 72205, United States A R T I C L E I N F O A B S T R A C T Article history: The GABAA receptor (GABAAR) is a major target of antiseizure drugs (ASDs). A variety of agents that act at Received 6 February 2013 GABAARs s are used to terminate or prevent seizures. Many act at distinct receptor sites determined by Received in revised form 16 April 2013 the subunit composition of the holoreceptor. For the benzodiazepines, barbiturates, and loreclezole, Accepted 17 April 2013 actions at the GABAAR are the primary or only known mechanism of antiseizure action. For topiramate, felbamate, retigabine, losigamone and stiripentol, GABAAR modulation is one of several possible Keywords: antiseizure mechanisms. Allopregnanolone, a progesterone metabolite that enhances GABAAR function, Inhibition led to the development of ganaxolone. Other agents modulate GABAergic ‘‘tone’’ by regulating the Epilepsy synthesis, transport or breakdown of GABA. GABAAR efficacy is also affected by the transmembrane Antiepileptic drugs chloride gradient, which changes during development and in chronic epilepsy. This may provide an GABA receptor Seizures additional target for ‘‘GABAergic’’ ASDs. GABAAR subunit changes occur both acutely during status Chloride channel epilepticus and in chronic epilepsy, which alter both intrinsic GABAAR function and the response to GABAAR-acting ASDs. -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. -
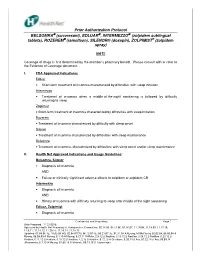
Prior Authorization Protocol BELSOMRA® (Suvorexant)
Prior Authorization Protocol BELSOMRA (suvorexant), EDLUAR , INTERMEZZO (zolpidem sublingual tablets), ROZEREM (ramelteon), SILENOR® (doxepin), ZOLPIMIST ® (zolpidem spray) NATL Coverage of drugs is first determined by the member’s pharmacy benefit. Please consult with or refer to the Evidence of Coverage document. I. FDA Approved Indications: Edluar • Short-term treatment of insomnia characterized by difficulties with sleep initiation Intermezzo • Treatment of insomnia when a middle-of-the-night awakening is followed by difficulty returning to sleep Zolpimist • Short-term treatment of insomnia characterized by difficulties with sleep initiation. Rozerem • Treatment of insomnia characterized by difficulty with sleep onset Silenor • Treatment of insomnia characterized by difficulties with sleep maintenance Belsomra • Treatment of insomnia, characterized by difficulties with sleep onset and/or sleep maintenance II. Health Net Approved Indications and Usage Guidelines: Belsomra, Silenor • Diagnosis of insomnia AND • Failure or clinically significant adverse effects to zolpidem or zolpidem CR Intermezzo • Diagnosis of insomnia AND • History of insomnia with difficulty returning to sleep after middle of the night awakening Edluar, Zolpimist • Diagnosis of insomnia Confidential and Proprietary Page 1 Date Prepared: 11.23.05JE Approved by Health Net Pharmacy & Therapeutic s Committee: 02.14.06, 04.11.06, 05.16.07, 11.19.08, 11.18.09, 11.17.10, 11.9.11, 11.14.12, 11.20.13, 11.19.14, 11.18.15 Updated: 05.09.06 JE, 10.03.06 RG, 02.08.07CM,