Nonbenzodiazepine Sedatives
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal of Pharmacology and Experimental Therapeutics
Journal of Pharmacology and Experimental Therapeutics Molecular Determinants of Ligand Selectivity for the Human Multidrug And Toxin Extrusion Proteins, MATE1 and MATE-2K Bethzaida Astorga, Sean Ekins, Mark Morales and Stephen H Wright Department of Physiology, University of Arizona, Tucson, AZ 85724, USA (B.A., M.M., and S.H.W.) Collaborations in Chemistry, 5616 Hilltop Needmore Road, Fuquay-Varina NC 27526, USA (S.E.) Supplemental Table 1. Compounds selected by the common features pharmacophore after searching a database of 2690 FDA approved compounds (www.collaborativedrug.com). FitValue Common Name Indication 3.93897 PYRIMETHAMINE Antimalarial 3.3167 naloxone Antidote Naloxone Hydrochloride 3.27622 DEXMEDETOMIDINE Anxiolytic 3.2407 Chlordantoin Antifungal 3.1776 NALORPHINE Antidote Nalorphine Hydrochloride 3.15108 Perfosfamide Antineoplastic 3.11759 Cinchonidine Sulfate Antimalarial Cinchonidine 3.10352 Cinchonine Sulfate Antimalarial Cinchonine 3.07469 METHOHEXITAL Anesthetic 3.06799 PROGUANIL Antimalarial PROGUANIL HYDROCHLORIDE 100MG 3.05018 TOPIRAMATE Anticonvulsant 3.04366 MIDODRINE Antihypotensive Midodrine Hydrochloride 2.98558 Chlorbetamide Antiamebic 2.98463 TRIMETHOPRIM Antibiotic Antibacterial 2.98457 ZILEUTON Antiinflammatory 2.94205 AMINOMETRADINE Diuretic 2.89284 SCOPOLAMINE Antispasmodic ScopolamineHydrobromide 2.88791 ARTICAINE Anesthetic 2.84534 RITODRINE Tocolytic 2.82357 MITOBRONITOL Antineoplastic Mitolactol 2.81033 LORAZEPAM Anxiolytic 2.74943 ETHOHEXADIOL Insecticide 2.64902 METHOXAMINE Antihypotensive Methoxamine -

Sedative Hypnotics
Louisiana Medicaid Sedative Hypnotics The Louisiana Uniform Prescription Drug Prior Authorization Form should be utilized to request: • Prior authorization for non-preferred sedative hypnotics; OR • Clinical authorization for tasimelteon (Hetlioz®, Hetlioz LQ™). Additional Point-of-Sale edits may apply. Some of tThese agents may have Black Box Warnings and/or may be subject to Risk Evaluation and Mitigation Strategy (REMS) under FDA safety regulations. Please refer to individual prescribing information for details. ___________________________________________________________________________________ Non-Preferred Agents Approval Criteria for Initial and Reauthorization Requests • There is no preferred alternative that is the exact same chemical entity, formulation, strength, etc.; AND • The requested medication has been prescribed for an approved diagnosis (if applicable); AND • Previous use of a preferred product - ONE of the following is required: o The recipient has had a treatment failure with at least one preferred product; OR o The recipient has had an intolerable side effect to at least one preferred product; OR o The recipient has documented contraindication(s) to all of the preferred products that are appropriate to use for the condition being treated; OR o There is no preferred product that is appropriate to use for the condition being treated; AND • By submitting the authorization request, the prescriber attests to the following: o The prescribing information for the requested medication has been thoroughly reviewed, including -

Paper Clip—High Risk Medications
You belong. PAPER CLIP—HIGH RISK MEDICATIONS Description: Some medications may be risky for people over 65 years of age and there may be safer drug choices to treat some conditions. It is recommended that medications are reviewed regularly with your providers/prescriber to ensure patient safety. Condition Treated Current Medication(s)-High Risk Safer Alternatives to Consider Urinary Tract Infections (UTIs), Nitrofurantoin Bactrim (sulfamethoxazole/trimethoprim) or recurrent UTIs, or Prophylaxis (Macrobid, or Macrodantin) Trimpex/Proloprim/Primsol (trimethoprim) Allergies Hydroxyzine (Vistaril, Atarax) Xyzal (Levocetirizine) Anxiety Hydroxyzine (Vistaril, Atarax) Buspar (Buspirone), Paxil (Paroxetine), Effexor (Venlafaxine) Parkinson’s Hydroxyzine (Vistaril, Atarax) Symmetrel (Amantadine), Sinemet (Carbidopa/levodopa), Selegiline (Eldepryl) Motion Sickness Hydroxyzine (Vistaril, Atarax) Antivert (Meclizine) Nausea & Vomiting Hydroxyzine (Vistaril, Atarax) Zofran (Ondansetron) Insomnia Hydroxyzine (Vistaril, Atarax) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Eszopiclone (Lunesta) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Zolpidem (Ambien) Ramelteon (Rozerem), Doxepin (Silenor) Chronic Insomnia Zaleplon (Sonata) Ramelteon (Rozerem), Doxepin (Silenor) Muscle Relaxants Cyclobenazprine (Flexeril, Amrix) NSAIDs (Ibuprofen, naproxen) or Hydrocodone Codeine Tramadol (Ultram) Baclofen (Lioresal) Tizanidine (Zanaflex) Migraine Prophylaxis Elavil (Amitriptyline) Propranolol (Inderal), Timolol (Blocadren), Topiramate (Topamax), -

New Drug Evaluation Monograph Template
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35, Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Abbreviated Class Update: Newer Drugs for Insomnia Month/Year of Review: November 2014 End date of literature search: August Week 3 2014 New drug(s): tasimelteon (Hetlioz™) Manufacturer: Vanda Pharmaceuticals Inc. suvorexant (Belsomra™) Merck & Co., Inc. Current Status of Preferred Drug List (PDL) Class: Preferred Agents: ZOLPIDEM TABLET Non Preferred Agents: ZALEPLON CAPSULE, ZOLPIDEM EXTENDED-RELEASE TABLET, ZOLPIMIST™, LUNESTA™, ROZEREM™, SILENOR™, EDULAR™, INTERMEZZO™ Prior Authorization (PA) Criteria: A quantity limit is in place to prevent chronic daily use of all sedatives (Appendix 2) and to determine if the diagnosis is funded. Treatment of sleep disorders without sleep apnea is not a funded diagnosis (Line 636) by Oregon Health Plan (OHP). Treatment of insomnia contributing to a covered comorbid condition is funded. Electronic step edits were incorporated into the PA process as recommended at the March 2014 P&T meeting to streamline this process. There is also a PA required to prevent a patient from receiving two concurrent oral sedative medications. Research Questions: Is there new comparative effectiveness or safety evidence since the last scan (literature search end date of Week 2, June 2013) of newer drugs for insomnia to warrant a change to the preferred drug list (PDL)? Is there evidence that tasimelteon or suvorexant is more effective or safer than currently available newer drugs for insomnia? Is there evidence that tasimelteon or suvorexant is more effective of safer for a sub-set of patients with insomnia? Conclusions: There is no new comparative evidence for newer drugs for insomnia since the last scan. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Specialty Pharmacy Program Drug List
Specialty Pharmacy Program Drug List The Specialty Pharmacy Program covers certain drugs commonly referred to as high-cost Specialty Drugs. To receive in- network benefits/coverage for these drugs, these drugs must be dispensed through a select group of contracted specialty pharmacies or your medical provider. Please call the BCBSLA Customer Service number on the back of your member ID card for information about our contracted specialty pharmacies. All specialty drugs listed below are limited to the retail day supply listed in your benefit plan (typically a 30-day supply). As benefits may vary by group and individual plans, the inclusion of a medication on this list does not imply prescription drug coverage. Please refer to your benefit plan for a complete list of benefits, including specific exclusions, limitations and member cost-sharing amounts you are responsible for such as a deductible, copayment and coinsurance. Brand Name Generic Name Drug Classification 8-MOP methoxsalen Psoralen ACTEMRA SC tocilizumab Monoclonal Antibody/Arthritis ACTHAR corticotropin Adrenocortical Insufficiency ACTIMMUNE interferon gamma 1b Interferon ADCIRCA tadalafil Pulmonary Vasodilator ADEMPAS riociguat Pulmonary Vasodilator AFINITOR everolimus Oncology ALECENSA alectinib Oncology ALKERAN (oral) melphalan Oncology ALUNBRIG brigatinib Oncology AMPYRA ER dalfampridine Multiple Sclerosis APTIVUS tipranavir HIV/AIDS APOKYN apomorphine Parkinson's Disease ARCALYST rilonacept Interleukin Blocker/CAPS ATRIPLA efavirenz-emtricitabine-tenofovir HIV/AIDS AUBAGIO -

Can We Induce Lucid Dreams? a Pharmacological Point of View Firas Hasan Bazzari Faculty of Pharmacy, Cairo University, Cairo, Egypt
A pharmacological view on lucid dream induction I J o D R Can we induce lucid dreams? A pharmacological point of view Firas Hasan Bazzari Faculty of Pharmacy, Cairo University, Cairo, Egypt Summary. The phenomenon of lucid dreaming, in which an individual has the ability to be conscious and in control of his dreams, has attracted the public attention, especially in the era of internet and social media platforms. With its huge pop- ularity, lucid dreaming triggered passionate individuals, particularly lucid dreamers, to spread their thoughts and experi- ences in lucid dreaming, and provide a number of tips and techniques to induce lucidity in dreams. Scientific research in the field of sleep and dreams has verified the phenomenon of lucid dreaming for decades. Nevertheless, various aspects regarding lucid dreaming are not fully understood. Many hypotheses and claims about lucid dreaming induction are yet to be validated, and at present lucid dreaming still lacks efficient and reliable induction methods. Understanding the molecular basis, brain physiology, and underlying mechanisms involved in lucid dreaming can aid in developing novel and more target-specific induction methods. This review will focus on the currently available scientific findings regarding neurotransmitters’ behavior in sleep, drugs observed to affect dreams, and proposed supplements for lucid dreaming, in order to discuss the possibility of inducing lucid dreams from a pharmacological point of view. Keywords: Lucid dreaming, Dreams, REM sleep, Neurotransmitters, Supplements, Pharmacology of lucid dreaming. 1. Introduction different methods and labeled according to the method’s success rate in inducing lucid dreams. Techniques, such as Lucid dreaming is a unique psychological phenomenon in mnemonic induced lucid dreams (MILD), reflection/reality which a dreaming individual is aware that he/she is dreaming testing, Tholey’s combined technique, light stimulus, and (Voss, 2010). -

Tasimelteon (Hetlioz) for Treatment of Non–24-Hour Sleep-Wake Disorder
AHRQ Healthcare Horizon Scanning System – Potential High-Impact Interventions Report Priority Area 08: Functional Limitations and Disability Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA290-2010-00006-C Prepared by: ECRI Institute 5200 Butler Pike Plymouth Meeting, PA 19462 June 2015 Statement of Funding and Purpose This report incorporates data collected during implementation of the Agency for Healthcare Research and Quality (AHRQ) Healthcare Horizon Scanning System by ECRI Institute under contract to AHRQ, Rockville, MD (Contract No. HHSA290-2010-00006-C). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. This report’s content should not be construed as either endorsements or rejections of specific interventions. As topics are entered into the System, individual topic profiles are developed for technologies and programs that appear to be close to diffusion into practice in the United States. Those reports are sent to various experts with clinical, health systems, health administration, and/or research backgrounds for comment and opinions about potential for impact. The comments and opinions received are then considered and synthesized by ECRI Institute to identify interventions that experts deemed, through the comment process, to have potential for high impact. Please see the methods section for more details about this process. -

Your Pharmacy Benefits Welcome to Your Pharmacy Plan
Your Pharmacy Benefits Welcome to Your Pharmacy Plan OptumRx manages your pharmacy benefits for your health plan sponsor. We look forward to helping you make informed decisions about medicines for you and your family. Please review this information to better understand your pharmacy benefit plan. Using Your Member ID Card You can use your pharmacy benefit ID card at any pharmacy participating in your plan’s pharmacy network. Show your ID card each time you fill a prescription at a network pharmacy. They will enter your card information and automatically file it with OptumRx. Your pharmacy will then collect your share of the payment. Your Pharmacy Network Your plan’s pharmacy network includes more than 67,000 independent and chain retail pharmacies nationwide. To find a network pharmacy near you, use the Locate a Pharmacy tool at www.optumrx.com. Or call Customer Service at 1-877-559-2955. Using Non -Network Pharmacies If you do not show the pharmacy your member ID card, or you fill a prescription at a non-network pharmacy, you must pay 100 percent of the pharmacy’s price for the drug. If the drug is covered by your plan, you can be reimbursed. To be reimbursed for eligible prescriptions, simply fill out and send a Direct Member Reimbursement Form with the pharmacy receipt(s) to OptumRx. Reimbursement amounts are based on contracted pharmacy rates minus your copayment or coinsurance. For a copy of the form, go to www.optumrx.com. Or call the Customer Service number above. The number is also on the back of your ID card. -
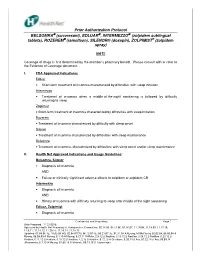
Prior Authorization Protocol BELSOMRA® (Suvorexant)
Prior Authorization Protocol BELSOMRA (suvorexant), EDLUAR , INTERMEZZO (zolpidem sublingual tablets), ROZEREM (ramelteon), SILENOR® (doxepin), ZOLPIMIST ® (zolpidem spray) NATL Coverage of drugs is first determined by the member’s pharmacy benefit. Please consult with or refer to the Evidence of Coverage document. I. FDA Approved Indications: Edluar • Short-term treatment of insomnia characterized by difficulties with sleep initiation Intermezzo • Treatment of insomnia when a middle-of-the-night awakening is followed by difficulty returning to sleep Zolpimist • Short-term treatment of insomnia characterized by difficulties with sleep initiation. Rozerem • Treatment of insomnia characterized by difficulty with sleep onset Silenor • Treatment of insomnia characterized by difficulties with sleep maintenance Belsomra • Treatment of insomnia, characterized by difficulties with sleep onset and/or sleep maintenance II. Health Net Approved Indications and Usage Guidelines: Belsomra, Silenor • Diagnosis of insomnia AND • Failure or clinically significant adverse effects to zolpidem or zolpidem CR Intermezzo • Diagnosis of insomnia AND • History of insomnia with difficulty returning to sleep after middle of the night awakening Edluar, Zolpimist • Diagnosis of insomnia Confidential and Proprietary Page 1 Date Prepared: 11.23.05JE Approved by Health Net Pharmacy & Therapeutic s Committee: 02.14.06, 04.11.06, 05.16.07, 11.19.08, 11.18.09, 11.17.10, 11.9.11, 11.14.12, 11.20.13, 11.19.14, 11.18.15 Updated: 05.09.06 JE, 10.03.06 RG, 02.08.07CM, -

Insomnia in Adults
New Guideline February 2017 The AASM has published a new clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults. These new recommendations are based on a systematic review of the literature on individual drugs commonly used to treat insomnia, and were developed using the GRADE methodology. The recommendations in this guideline define principles of practice that should meet the needs of most adult patients, when pharmacologic treatment of chronic insomnia is indicated. The clinical practice guideline is an essential update to the clinical guideline document: Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307–349. SPECIAL ARTICLE Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults Sharon Schutte-Rodin, M.D.1; Lauren Broch, Ph.D.2; Daniel Buysse, M.D.3; Cynthia Dorsey, Ph.D.4; Michael Sateia, M.D.5 1Penn Sleep Centers, Philadelphia, PA; 2Good Samaritan Hospital, Suffern, NY; 3UPMC Sleep Medicine Center, Pittsburgh, PA; 4SleepHealth Centers, Bedford, MA; 5Dartmouth-Hitchcock Medical Center, Lebanon, NH Insomnia is the most prevalent sleep disorder in the general popula- and disease management of chronic adult insomnia, using existing tion, and is commonly encountered in medical practices. Insomnia is evidence-based insomnia practice parameters where available, and defined as the subjective perception of difficulty with sleep initiation, consensus-based recommendations to bridge areas where such pa- duration, consolidation, or quality that occurs despite adequate oppor- rameters do not exist. -

Tasimelteon (Hetlioz®) EOCCO POLICY
tasimelteon (Hetlioz®) EOCCO POLICY Policy Type: PA/SP Pharmacy Coverage Policy: EOCCO215 Description Tasimelteon (Hetlioz, Hetlioz LQ) is an agonist of melatonin MT1 and MT2 receptors which are thought to be involved in the control of circadian rhythms. Length of Authorization • Initial: Six months • Renewal: 12 months Quantity Limits Product Name Dosage Form Indication Quantity Limit Non 24-Hour Sleep-Wake tasimelteon Disorder; Nighttime Sleep 20 mg capsules 30 capsules/30 days (Hetlioz) Disturbances in Smith- Magenis Syndrome (SMS) Nighttime Sleep tasimelteon 4 mg/mL oral 0.7 mg/kg* Disturbances in Smith- (Hetlioz LQ) suspension Magenis Syndrome (SMS) 158 ml bottle** * for members weighing 28kg or less ** for members weighing more than 28kg Initial Evaluation I. Tasimelteon (Hetlioz, Hetlioz LQ) may be considered medically necessary when the following criteria are met: A. Medication is prescribed by, or in consultation with, a neurologist, sleep specialist, or psychiatrist; AND B. Treatment with melatonin (for at least three months continuously) has been ineffective, contraindicated, or not tolerated; AND C. A diagnosis of Non-24-hour sleep-wake disorder (N24HSWD) when the following are met: 1. Member is 18 years of age or older; AND 2. Member has a diagnosis of total blindness in both eyes without light perception; AND 3. Provider has documented progressively shifting sleep-wake times with sleep diaries and/or actigraphy for at least 14 days; AND 4. Treatment with at least TWO of the following groups has been ineffective or not tolerated, or all are contraindicated: i. benzodiazepines (eg. flurazepam, lorazepam, temazepam) 1 tasimelteon (Hetlioz®) EOCCO POLICY ii.