Epipen As an Alternative to Glucagon in the Treatment of Hypoglycemia in Children with Diabetes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emerging Evidence for a Central Epinephrine-Innervated A1- Adrenergic System That Regulates Behavioral Activation and Is Impaired in Depression
Neuropsychopharmacology (2003) 28, 1387–1399 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Perspective Emerging Evidence for a Central Epinephrine-Innervated a1- Adrenergic System that Regulates Behavioral Activation and is Impaired in Depression ,1 1 1 1 1 Eric A Stone* , Yan Lin , Helen Rosengarten , H Kenneth Kramer and David Quartermain 1Departments of Psychiatry and Neurology, New York University School of Medicine, New York, NY, USA Currently, most basic and clinical research on depression is focused on either central serotonergic, noradrenergic, or dopaminergic neurotransmission as affected by various etiological and predisposing factors. Recent evidence suggests that there is another system that consists of a subset of brain a1B-adrenoceptors innervated primarily by brain epinephrine (EPI) that potentially modulates the above three monoamine systems in parallel and plays a critical role in depression. The present review covers the evidence for this system and includes findings that brain a -adrenoceptors are instrumental in behavioral activation, are located near the major monoamine cell groups 1 or target areas, receive EPI as their neurotransmitter, are impaired or inhibited in depressed patients or after stress in animal models, and a are restored by a number of antidepressants. This ‘EPI- 1 system’ may therefore represent a new target system for this disorder. Neuropsychopharmacology (2003) 28, 1387–1399, advance online publication, 18 June 2003; doi:10.1038/sj.npp.1300222 Keywords: a1-adrenoceptors; epinephrine; motor activity; depression; inactivity INTRODUCTION monoaminergic systems. This new system appears to be impaired during stress and depression and thus may Depressive illness is currently believed to result from represent a new target for this disorder. -

Cocaine Intoxication and Hypertension
THE EMCREG-INTERNATIONAL CONSENSUS PANEL RECOMMENDATIONS Cocaine Intoxication and Hypertension Judd E. Hollander, MD From the Department of Emergency Medicine, University of Pennsylvania, Philadelphia, PA. 0196-0644/$-see front matter Copyright © 2008 by the American College of Emergency Physicians. doi:10.1016/j.annemergmed.2007.11.008 [Ann Emerg Med. 2008;51:S18-S20.] with cocaine intoxication is analogous to that of the patient with hypertension: the treatment should be geared toward the Cocaine toxicity has been reported in virtually all organ patient’s presenting complaint. systems. Many of the adverse effects of cocaine are similar to When the medical history is clear and symptoms are mild, adverse events that can result from either acute hypertensive laboratory evaluation is usually unnecessary. In contrast, if the crisis or chronic effects of hypertension. Recognizing when the patient has severe toxicity, evaluation should be geared toward specific disease requires treatment separate from cocaine toxicity the presenting complaint. Laboratory evaluation may include a is paramount to the treatment of patients with cocaine CBC count; determination of electrolyte, glucose, blood urea intoxication. nitrogen, creatine kinase, and creatinine levels; arterial blood The initial physiologic effect of cocaine on the cardiovascular gas analysis; urinalysis; and cardiac marker determinations. system is a transient bradycardia as a result of stimulation of the Increased creatine kinase level occurs with rhabdomyolysis. vagal nuclei. Tachycardia typically ensues, predominantly from Cardiac markers are increased in myocardial infarction. Cardiac increased central sympathetic stimulation. Cocaine has a troponin I is preferred to identify acute myocardial13 infarction. cardiostimulatory effect through sensitization to epinephrine A chest radiograph should be obtained in patients with and norepinephrine. -
Atopic Children and Use of Prescribed Medication: a Comprehensive Study in General Practice
RESEARCH ARTICLE Atopic children and use of prescribed medication: A comprehensive study in general practice David H. J. Pols1*, Mark M. J. Nielen2, Arthur M. Bohnen1, Joke C. Korevaar2, Patrick J. E. Bindels1 1 Department of General Practice, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, 2 NIVEL, Netherlands Institute for Health Services Research, Utrecht, The Netherlands a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 Purpose A comprehensive and representative nationwide general practice database was explored to study associations between atopic disorders and prescribed medication in children. OPEN ACCESS Citation: Pols DHJ, Nielen MMJ, Bohnen AM, Korevaar JC, Bindels PJE (2017) Atopic children Method and use of prescribed medication: A All children aged 0±18 years listed in the NIVEL Primary Care Database in 2014 were comprehensive study in general practice. PLoS ONE 12(8): e0182664. https://doi.org/10.1371/ selected. Atopic children with atopic eczema, asthma and allergic rhinitis (AR) were journal.pone.0182664 matched with controls (not diagnosed with any of these disorders) within the same general Editor: Anthony Peter Sampson, University of practice on age and gender. Logistic regression analyses were performed to study the differ- Southampton School of Medicine, UNITED ences in prescribed medication between both groups by calculating odds ratios (OR); 93 dif- KINGDOM ferent medication groups were studied. Received: March 24, 2017 Accepted: July 13, 2017 Results Published: August 24, 2017 A total of 45,964 children with at least one atopic disorder were identified and matched with Copyright: © 2017 Pols et al. This is an open controls. Disorder-specific prescriptions seem to reflect evidence-based medicine guide- access article distributed under the terms of the lines for atopic eczema, asthma and AR. -
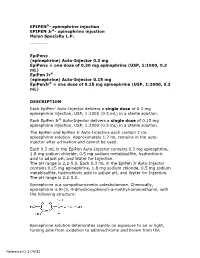
Epipen Injection Label
EPIPEN®- epinephrine injection EPIPEN Jr®- epinephrine injection Mylan Specialty L.P. ---------- EpiPen® (epinephrine) Auto-Injector 0.3 mg EpiPen® = one dose of 0.30 mg epinephrine (USP, 1:1000, 0.3 mL) EpiPen Jr® (epinephrine) Auto-Injector 0.15 mg EpiPenJr® = one dose of 0.15 mg epinephrine (USP, 1:2000, 0.3 mL) DESCRIPTION Each EpiPen® Auto-Injector delivers a single dose of 0.3 mg epinephrine injection, USP, 1:1000 (0.3 mL) in a sterile solution. Each EpiPen Jr® Auto-Injector delivers a single dose of 0.15 mg epinephrine injection, USP, 1:2000 (0.3 mL) in a sterile solution. The EpiPen and EpiPen Jr Auto-Injectors each contain 2 mL epinephrine solution. Approximately 1.7 mL remains in the auto- injector after activation and cannot be used. Each 0.3 mL in the EpiPen Auto-Injector contains 0.3 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Each 0.3 mL in the EpiPen Jr Auto-Injector contains 0.15 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Epinephrine is a sympathomimetic catecholamine. Chemically, epinephrine is B-(3, 4-dihydroxyphenyl)-a-methyl-aminoethanol, with the following structure: Epinephrine solution deteriorates rapidly on exposure to air or light, turning pink from oxidation to adrenochrome and brown from the Reference ID: 3176782 formation of melanin. -
Patients on Beta-Blockers
Systemic Allergic & Immunoglobulin Disorders Bryan L. Martin, DO, MMAS, FACAAI, FAAAAI, FACP, FACOI Emeritus Professor of Medicine and Pediatrics President, American College of Allergy, Asthma & Immunology Disclosures . None 2 Objectives . Pass the boards! . Recognize anaphylaxis and understand the new guidelines for the treatment of anaphylaxis . Compare and contrast anaphylactic and anaphylactoid reactions 3 The Patient . 45 year old woman goes to lunch with her friends . While eating she develops GI upset, dizziness, shortness of breath and hives . Her friends drive her to your nearby clinic Initial Evaluation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating a shrimp salad. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Anaphylaxis presentation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating lunch. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Initial Response to anaphylaxis . -

Diphenhydramine (Systemic) Epinephrine (Systemic)
DIPHENHYDRAMINE (SYSTEMIC) ^ Diphenhist [OTC] see DiphenhydrAMINE (Systemic) on page 34 Insomnia, occasional: Oral: Children 2 to 12 years, weighing 10 to 50 kg (off-label use): DiphenhydrAMINE (Systemic) Limited data available: 1 mg/kg administered 30 minutes before bedtime; maximum single dose: 50 mg (Russo, 1976) Brand Names: US Aler-Dryl [OTC]; Allergy Relief Childrens Children ≥12 years and Adolescents: Refer to adult dosing. [OTC]; Allergy Relief [OTC]; Altaryl [OTC]; Anti-Hist Allergy [OTC]; Motion sickness: Banophen [OTC]; Benadryl Allergy Childrens [OTC]; Benadryl Prophylaxis: Oral: Allergy [OTC]; Benadryl Dye-Free Allergy [OTC]; Benadryl [OTC]; Manufacturer's labeling: Infants, Children, and Adolescents: Complete Allergy Medication [OTC]; Complete Allergy Relief [OTC]; Note: Administer 30 minutes before motion Dicopanol FusePaq; Dicopanol RapidPaq; Diphen [OTC]; Diphenh- Weight-directed dosing: 5 mg/kg/day divided into 3 to 4 doses; ist [OTC]; Genahist [OTC]; Geri-Dryl [OTC]; GoodSense Allergy maximum: 300 mg daily Relief [OTC]; Naramin [OTC]; Nighttime Sleep Aid [OTC]; Nytol Fixed dosing: 12.5 to 25 mg 3 to 4 times daily Maximum Strength [OTC]; Nytol [OTC]; Ormir [OTC]; PediaCare Alternate dosing: Children 2 to 12 years: Limited data available: Childrens Allergy [OTC]; Pharbedryl; Pharbedryl [OTC]; Q-Dryl 0.5 to 1 mg/kg/dose every 6 hours; maximum single dose: [OTC]; QlearQuil Nighttime Allergy [OTC]; Quenalin [OTC] [DSC]; 25 mg. First dose should be administered 1 hour before travel Scot-Tussin Allergy Relief [OTC]; Siladryl -

Xylocaine® (Lidocaine Hcl and Epinephrine Injection, USP) for Infiltration and Nerve Block Rx Only
XYLOCAINE MPF- lidocaine hydrochloride injection, solution XYLOCAINE - lidocaine hydrochloride injection, solution XYLOCAINE MPF- lidocaine hydrochloride,epinephrine bitartrate injection, solution XYLOCAINE - lidocaine hydrochloride,epinephrine bitartrate injection, solution Fresenius Kabi USA, LLC ---------- Xylocaine® (lidocaine HCl Injection, USP) Xylocaine® (lidocaine HCl and epinephrine Injection, USP) For Infiltration and Nerve Block Rx only DESCRIPTION Xylocaine (lidocaine HCl) Injections are sterile, nonpyrogenic, aqueous solutions that contain a local anesthetic agent with or without epinephrine and are administered parenterally by injection. See INDICATIONS AND USAGE section for specific uses. Xylocaine solutions contain lidocaine HCl, which is chemically designated as acetamide, 2- (diethylamino)-N-(2,6-dimethylphenyl)-, monohydrochloride and has the molecular wt. 270.8. Lidocaine HCl (C 14H 22N 2O • HCl) has the following structural formula: Epinephrine is (-) -3, 4-Dihydroxy-α-[(methylamino) methyl] benzyl alcohol and has the molecular wt. 183.21. Epinephrine (C 9H 13NO 3) has the following structural formula: Dosage forms listed as Xylocaine-MPF indicate single dose solutions that are Methyl Paraben Free (MPF). Xylocaine MPF is a sterile, nonpyrogenic, isotonic solution containing sodium chloride. Xylocaine in multiple dose vials: Each mL also contains 1 mg methylparaben as antiseptic preservative. The pH of these solutions is adjusted to approximately 6.5 (5.0 to 7.0) with sodium hydroxide and/or hydrochloric acid. Xylocaine MPF with Epinephrine is a sterile, nonpyrogenic, isotonic solution containing sodium chloride. Each mL contains lidocaine hydrochloride and epinephrine, with 0.5 mg sodium metabisulfite as an antioxidant and 0.2 mg citric acid as a stabilizer. Xylocaine with Epinephrine in multiple dose as an antioxidant and 0.2 mg citric acid as a stabilizer. -

Emergency Treatment for Vaccine Reactions
Massachusetts Department of Public Health Division of Epidemiology and Immunization Model Standing Orders Emergency Treatment for Vaccine Reactions Note: These model standing orders are current as of December 2010. They should be reviewed carefully against the most current recommendations and may be revised by the clinician signing them. Because of possible hypersensitivity to vaccine components, people administering biologic products or serum should be prepared to recognize and treat allergic reactions, including anaphylaxis. The necessary medications, equipment, and staff competent to maintain the patency of the airway and to manage cardiovascular collapse, must be immediately available. Vaccine providers must be in close proximity to a telephone so that emergency medical personnel can be summoned immediately, if necessary. All providers should be familiar with the facility/agency emergency plan and should be certified in cardio- pulmonary resuscitation (CPR). Whenever possible, patients should be observed for an allergic reaction for 15 to 20 minutes after receiving vaccine. I. Medical Management of Non-Anaphylactic Vaccine Reactions Reaction Symptoms Management Soreness, redness, itching, or Apply a cold compress to the injection site. Consider giving an analgesic or Localized swelling at the injection site antipruritic medication (See Medication Table 1 for dosing) Slight bleeding Apply an adhesive compress over the injection site. Continuous bleeding Place thick layer of gauze pads over site and maintain direct and firm pressure; -

Albuterol: Effects on the Beta-2 Receptor
ALBUTEROL: EFFECTS ON THE BETA-2 RECEPTOR Poster group: Rostian Akpor-Mensah, Laura Clark, Brooke Koenig, Emily Komp, Ashley Voigt, Jennifer Watzig Jmol group: Jacob Kachelmeier, Adam Naker, Staci Prise Research advisor: Dr. Daniel Sem Faculty advisor: Dr. Ernest Stremski Institution: Concordia School of Pharmacy, 12800 N Lake Shore Dr, Mequon, WI 53097 Preceptors: Tom Wilke, RPH, Edward Merle Johnson, PharmD, Vicktoria McGruder, PharmD, Jeffery Kotwicka, PharmD, Liza Papi, RPh ABSTRACT MOLECULAR STORY FURTHER RESEARCH D RUG TARGET Albuterol causes off-target effects on β -receptors in the heart leading to Asthma is a chronic airway disease that inflames and narrows the bronchi 1 • The binding site is a β2-adrenergic receptor in the and bronchioles, thus making breathing very difficult. The absolute tachycardia. Future research should identify an antagonist to reduce or lungs. It is a G-protein coupled receptor (GPCR), etiology of asthma is unknown but hereditary, food and environmental prevent tachycardia after albuterol administration. One study which is a transmembrane receptor2 allergens seem to play significant roles in its onset. Unfortunately, there is successfully utilized magnesium sulfate to prevent tachycardia after The ligand binding site is inside the barrel formed 7 no cure for asthma. Management focuses on treating symptoms in acute • administration of salbutamol . events and avoiding known triggers. The standard treatments are by the 7 transmembrane helices of the GPCR bronchodilators and steroids1. ALBUTEROL Another option is to utilize the R enantiomer, levalbuterol. Levalbuterol • Short-acting β2-adrenergic receptor agonist has higher affinity for the β -receptors in the lungs. Research has shown 2 • Exists as a racemic mixture: equal amounts of the Figure 2. -

1 How to Use an Epipen® (Epinephrine Injection, USP) Auto
How to use an EpiPen® (epinephrine injection, USP) Auto-Injector 1 PREPARE Remove the Auto-Injector from the clear carrier tube. Flip open the yellow cap of your EpiPen® or the green cap of your EpiPen Jr® carrier tube. Tip and slide the auto-injector out of the carrier tube. Hold the auto-injector in your fist with the orange tip pointing downward. ® NEVER-SEE-NEEDLE ® helps with protection. Protects against needle Blue to the sky, orange to the thigh . exposure before and after use. With your other hand, remove the blue NOTE: safety release by pulling straight up • The needle comes out of the orange tip. without bending or twisting it. • To avoid an accidental injection, never put your thumb, fingers or hand over the orange tip. If an accidental injection happens, get medical help right away. 2 ADMINISTER If you are administering to a young child, hold the leg firmly in place while administering an injection. Place the orange tip against the middle of the outer thigh (upper leg) at a right angle (perpendicular) to the thigh. Swing and push the auto-injector firmlyuntil it “clicks.” The click signals that the injection has started. Hold firmly in place for 3 seconds (count slowly 1, 2, 3). Remove the auto-injector from the thigh. The orange tip will extend to cover the needle. If the needle is still visible, do not attempt to reuse it. Massage the injection area for 10 seconds. 3 GET EMERGENCY MEDICAL HELP RIGHT AWAY You may need further medical attention. If symptoms continue or recur, you may need to use a second EpiPen® or EpiPen Jr® Auto-Injector. -

Epinephrine and Lidocaine Hydrochloride
DESCRIPTION: The pharmacological/toxicological actions allergic-type reactions including anaphylactic nant hyperthermia should be available. Early formed, the type and amount of drug used, and Xylocaine (lidocaine HCl) Injections are sterile, of these metabolites are similar to, but less symptoms and life-threatening or less severe unexplained signs of tachycardia, tachypnea, the technique of drug administration. Adverse nonpyrogenic, aqueous solutions that contain potent than, those of lidocaine HCl. Approxi- asthmatic episodes in certain susceptible peo- labile blood pressure and metabolic acidosis reactions in the parturient, fetus and neonate a local anesthetic agent with or without epi- mately 90% of lidocaine HCl administered is ple. The overall prevalence of sulfite sensitivity in may precede temperature elevation. Success- involve alterations of the central nervous system, nephrine and are administered parenterally by excreted in the form of various metabolites, the general population is unknown and probably ful outcome is dependent on early diagnosis, peripheral vascular tone and cardiac function. injection. See INDICATIONS for specific uses. and less than 10% is excreted unchanged. The low. Sulfite sensitivity is seen more frequently in prompt discontinuance of the suspect triggering Maternal hypotension has resulted from Xylocaine solutions contain lidocaine HCl, primary metabolite in urine is a conjugate of asthmatic than in non-asthmatic people. agent(s) and institution of treatment, including regional anesthesia. Local anesthetics produce which is chemically designated as acetamide, 4-hydroxy-2,6-dimethylaniline. Anaphylactic reactions may occur following oxygen therapy, indicated supportive measures vasodilation by blocking sympathetic nerves. 2-(diethylamino)-N-(2,6-dimethylphenyl)-, The elimination half-life of lidocaine HCl fol- administration of lidocaine hydrochloride (see and dantrolene (consult dantrolene sodium Elevating the patient’s legs and positioning her monohydrochloride and has the molecular wt. -

Review of Existing Classification Efforts
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.1.1 Review of existing classification efforts Due date of deliverable: (15.01.2008) Actual submission date: (07.02.2008) Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UGent Revision 1.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public X PP Restricted to other programme participants (including the Commission Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) Task 4.1 : Review of existing classification efforts Authors: Kristof Pil, Elke Raes, Thomas Van den Neste, An-Sofie Goessaert, Jolien Veramme, Alain Verstraete (Ghent University, Belgium) Partners: - F. Javier Alvarez (work package leader), M. Trinidad Gómez-Talegón, Inmaculada Fierro (University of Valladolid, Spain) - Monica Colas, Juan Carlos Gonzalez-Luque (DGT, Spain) - Han de Gier, Sylvia Hummel, Sholeh Mobaser (University of Groningen, the Netherlands) - Martina Albrecht, Michael Heiβing (Bundesanstalt für Straßenwesen, Germany) - Michel Mallaret, Charles Mercier-Guyon (University of Grenoble, Centre Regional de Pharmacovigilance, France) - Vassilis Papakostopoulos, Villy Portouli, Andriani Mousadakou (Centre for Research and Technology Hellas, Greece) DRUID 6th Framework Programme Deliverable D.4.1.1. Revision 1.0 Review of Existing Classification Efforts Page 2 of 127 Introduction DRUID work package 4 focusses on the classification and labeling of medicinal drugs according to their influence on driving performance.