Epinephrine Training Protocol for Allergic Reaction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Congenital Adrenal Hyperplasia in the Newborn
The Leo Fung Center for CAH and Disorders of Sex Development Congenital Adrenal Hyperplasia in the Newborn Contents Introduction 1 What is congenital adrenal hyperplasia? 1 Types of CAH 3 Diagnosing CAH in newborns 4 Treating CAH 5 Untreated CAH 7 CAH in children and young adults 8 Frequently asked questions 9 Glossary 11 Resources 13 Acknowledgments 14 Congenital Adrenal Hyperplasia in the Newborn 1 Introduction This handbook will provide you and your family information about congenital adrenal hyperplasia (CAH). While this guide will not answer all of your questions, it will provide basic medical facts that will help you to talk to your doctors. It is important to know that CAH cannot be cured but it can be treated. Your child will need to take medicine for the rest of his or her life. If your child takes this medicine, he or she should have a completely normal life in every way. Successful treatment requires teamwork between you and your doctor. The doctor will monitor your child in order to know what dose of medicine is needed. We ask that you give your baby the medication on the schedule recommended by your doctor. Your family is not alone. The Leo Fung Center for CAH and Disorders of Sex Development (DSD) at University of Minnesota Amplatz Children’s Hospital, provides a large network of support, including medical specialists, therapists and counselors who all have expertise in caring for patients with CAH. What is congenital adrenal hyperplasia? Let’s begin by examining each word. • Congenital means existing at birth (inherited). • Adrenal means that the adrenal glands are involved. -

Emerging Evidence for a Central Epinephrine-Innervated A1- Adrenergic System That Regulates Behavioral Activation and Is Impaired in Depression
Neuropsychopharmacology (2003) 28, 1387–1399 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Perspective Emerging Evidence for a Central Epinephrine-Innervated a1- Adrenergic System that Regulates Behavioral Activation and is Impaired in Depression ,1 1 1 1 1 Eric A Stone* , Yan Lin , Helen Rosengarten , H Kenneth Kramer and David Quartermain 1Departments of Psychiatry and Neurology, New York University School of Medicine, New York, NY, USA Currently, most basic and clinical research on depression is focused on either central serotonergic, noradrenergic, or dopaminergic neurotransmission as affected by various etiological and predisposing factors. Recent evidence suggests that there is another system that consists of a subset of brain a1B-adrenoceptors innervated primarily by brain epinephrine (EPI) that potentially modulates the above three monoamine systems in parallel and plays a critical role in depression. The present review covers the evidence for this system and includes findings that brain a -adrenoceptors are instrumental in behavioral activation, are located near the major monoamine cell groups 1 or target areas, receive EPI as their neurotransmitter, are impaired or inhibited in depressed patients or after stress in animal models, and a are restored by a number of antidepressants. This ‘EPI- 1 system’ may therefore represent a new target system for this disorder. Neuropsychopharmacology (2003) 28, 1387–1399, advance online publication, 18 June 2003; doi:10.1038/sj.npp.1300222 Keywords: a1-adrenoceptors; epinephrine; motor activity; depression; inactivity INTRODUCTION monoaminergic systems. This new system appears to be impaired during stress and depression and thus may Depressive illness is currently believed to result from represent a new target for this disorder. -

Conduct Protocol in Emergency: Acute Adrenal Insufficiency
ORIGINAL ARTICLE FARES AND SANTOS Conduct protocol in emergency: Acute adrenal insufficiency ADIL BACHIR FARES1*, RÔMULO AUGUSTO DOS SANTOS2 1Medical Student, 6th year, Faculdade de Medicina de São José do Rio Preto (Famerp), São José do Rio Preto, SP, Brazil 2Degree in Endocrinology and Metabology from Sociedade Brasileira de Endocrinologia e Metabologia (SBEM). Assistant Physician at the Internal Medicine Service of Hospital de Base. Researcher at Centro Integrado de Pesquisa (CIP), Hospital de Base, São José do Rio Preto. Endocrinology Coordinator of the Specialties Outpatient Clinic (AME), São José do Rio Preto, SP, Brazil SUMMARY Introduction: Acute adrenal insufficiency or addisonian crisis is a rare comor- bidity in emergency; however, if not properly diagnosed and treated, it may progress unfavorably. Objective: To alert all health professionals about the diagnosis and correct treatment of this complication. Method: We performed an extensive search of the medical literature using spe- cific search tools, retrieving 20 articles on the topic. Results: Addisonian crisis is a difficult diagnosis due to the unspecificity of its signs and symptoms. Nevertheless, it can be suspected in patients who enter the emergency room with complaints of abdominal pain, hypotension unresponsive to volume or vasopressor agents, clouding, and torpor. This situation may be associated with symptoms suggestive of chronic adrenal insufficiency such as hyperpigmentation, salt craving, and association with autoimmune diseases such as vitiligo and Hashimoto’s thyroiditis. Hemodynamically stable patients Study conducted at Faculdade may undergo more accurate diagnostic methods to confirm or rule out addiso- de Medicina de São José do nian crisis. Delay to perform diagnostic tests should be avoided, in any circum- Rio Preto (Famerp), São José do Rio Preto, SP, Brazil stances, and unstable patients should be immediately medicated with intravenous glucocorticoid, even before confirmatory tests. -

Preventable Deaths: Panhypopituitarism and Adrenal Insufficiency
Preventable Deaths: Panhypopituitarism and adrenal insufficiency. What you need to know What is panhypopituitarism? Your child has been diagnosed with a big scary sounding word, and all you can think is: 'What does this mean? and 'Why have I never heard of this?' Simply put, panhypopituitarism means that your child's pituitary gland does not function properly and as a result, your child is deficient in one or several hormones. Some children have congenital panhypopituitarism, meaning they are born with it. Others have acquired panhypopituitarism following an event such as head trauma, brain tumor surgery, or brain radiation. It is rare enough that is entirely possible, in fact, probable, that you will not initially know anyone else with this disorder. What will my child need? Although the diagnosis and condition can seem intimidating, it is very manageable once you understand what is needed. Unfortunately the condition cannot be cured or reversed, but again, it can be effectively managed. Your child will need to take medications to replace the missing hormones. These might include thyroid hormone, growth hormone, cortisol, and/or possibly others. Your doctor will go over these with you, as dosages vary from child to child. Most medications are taken orally, but growth hormone must be taken by daily injection. Your endocrinologist will work with you and your child to achieve the proper dosages and will guide you in how to administer any necessary medications. Why is it sometimes life threatening? What is adrenal insufficiency? Of the hormone deficiencies your child may have, the most critical is cortisol, also known as the 'stress hormone.' Cortisol is essential for life , and is therefore the central focus of this guide. -

Cocaine Intoxication and Hypertension
THE EMCREG-INTERNATIONAL CONSENSUS PANEL RECOMMENDATIONS Cocaine Intoxication and Hypertension Judd E. Hollander, MD From the Department of Emergency Medicine, University of Pennsylvania, Philadelphia, PA. 0196-0644/$-see front matter Copyright © 2008 by the American College of Emergency Physicians. doi:10.1016/j.annemergmed.2007.11.008 [Ann Emerg Med. 2008;51:S18-S20.] with cocaine intoxication is analogous to that of the patient with hypertension: the treatment should be geared toward the Cocaine toxicity has been reported in virtually all organ patient’s presenting complaint. systems. Many of the adverse effects of cocaine are similar to When the medical history is clear and symptoms are mild, adverse events that can result from either acute hypertensive laboratory evaluation is usually unnecessary. In contrast, if the crisis or chronic effects of hypertension. Recognizing when the patient has severe toxicity, evaluation should be geared toward specific disease requires treatment separate from cocaine toxicity the presenting complaint. Laboratory evaluation may include a is paramount to the treatment of patients with cocaine CBC count; determination of electrolyte, glucose, blood urea intoxication. nitrogen, creatine kinase, and creatinine levels; arterial blood The initial physiologic effect of cocaine on the cardiovascular gas analysis; urinalysis; and cardiac marker determinations. system is a transient bradycardia as a result of stimulation of the Increased creatine kinase level occurs with rhabdomyolysis. vagal nuclei. Tachycardia typically ensues, predominantly from Cardiac markers are increased in myocardial infarction. Cardiac increased central sympathetic stimulation. Cocaine has a troponin I is preferred to identify acute myocardial13 infarction. cardiostimulatory effect through sensitization to epinephrine A chest radiograph should be obtained in patients with and norepinephrine. -

Mechanisms and Clinical Consequences of Critical Illness Associated Adrenal Insufficiency Paul E
Mechanisms and clinical consequences of critical illness associated adrenal insufficiency Paul E. Marik Purpose of review Abbreviations Adrenal insufficiency is being diagnosed with increasing ACTH adrenocorticotrophic hormone frequency in critically ill patients. There exists, however, ARDS acute respiratory distress syndrome CBG corticosteroid-binding globulin much controversy in the literature as to the nature of this CIRCI critical illness-related corticosteroid insufficiency entity, including its pathophysiology, epidemiology, CRH corticotrophin-releasing hormone HDL high-density lipoprotein diagnosis and treatment. The review summarizes our HPA hypothalamic–pituitary–adrenal current understanding of the causes and consequences of SAS sympatho-adrenal system TNF tumor necrosis factor adrenal insufficiency in critically ill patients. Relevant findings Activation of the hypothalamic–pituitary–adrenal axis with ß 2007 Lippincott Williams & Wilkins the production of cortisol is a fundamental component of 1070-5295 the stress response and is essential for survival of the host. Dysfunction of the hypothalamic–pituitary–adrenal axis with decreased glucocorticoid activity is being increasingly Introduction recognized in critically ill patients, particularly those with The stress system receives and integrates a diversity of sepsis. This condition is best referred to as ‘critical illness- cognitive, emotional, neurosensory and peripheral related corticosteroid insufficiency’. Critical illness-related somatic signals that arrive through distinct -
Atopic Children and Use of Prescribed Medication: a Comprehensive Study in General Practice
RESEARCH ARTICLE Atopic children and use of prescribed medication: A comprehensive study in general practice David H. J. Pols1*, Mark M. J. Nielen2, Arthur M. Bohnen1, Joke C. Korevaar2, Patrick J. E. Bindels1 1 Department of General Practice, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, 2 NIVEL, Netherlands Institute for Health Services Research, Utrecht, The Netherlands a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 Purpose A comprehensive and representative nationwide general practice database was explored to study associations between atopic disorders and prescribed medication in children. OPEN ACCESS Citation: Pols DHJ, Nielen MMJ, Bohnen AM, Korevaar JC, Bindels PJE (2017) Atopic children Method and use of prescribed medication: A All children aged 0±18 years listed in the NIVEL Primary Care Database in 2014 were comprehensive study in general practice. PLoS ONE 12(8): e0182664. https://doi.org/10.1371/ selected. Atopic children with atopic eczema, asthma and allergic rhinitis (AR) were journal.pone.0182664 matched with controls (not diagnosed with any of these disorders) within the same general Editor: Anthony Peter Sampson, University of practice on age and gender. Logistic regression analyses were performed to study the differ- Southampton School of Medicine, UNITED ences in prescribed medication between both groups by calculating odds ratios (OR); 93 dif- KINGDOM ferent medication groups were studied. Received: March 24, 2017 Accepted: July 13, 2017 Results Published: August 24, 2017 A total of 45,964 children with at least one atopic disorder were identified and matched with Copyright: © 2017 Pols et al. This is an open controls. Disorder-specific prescriptions seem to reflect evidence-based medicine guide- access article distributed under the terms of the lines for atopic eczema, asthma and AR. -

Anemia LECTURE in INTERNAL MEDICINE for IV COURSE
Essentials of Diagnosis, Treatment and Prevention of Major Endocrine Diseases: Diseases of the Adrenal Glands. Adrenal Insufficiency. Adrenal Hyperfunction. Hormonally Active Tumors. LECTURE IN INTERNAL MEDICINE FOR IV COURSE STUDENTS M. Yabluchansky, L. Bogun, L. Martymianova, O. Bychkova, N. Lysenko, N. Makienko V.N. Karazin National University Medical School’ Internal Medicine Dept. Plan of the Lecture • Definition • Epidemiology • Risk factors • Etiology • Mechanisms • Classification • Clinical presentation • Diagnosis • Treatment • Prognosis • Prophylaxis • Abbreviations • Diagnostic guidelines http://www.thelancet.com/pb/assets/raw/pb/assets/raw/Lancet/clinical/diseases/Cushing's.jpg http://peninsulamassage.com.au/wp-content/uploads/2012/08/Adrenal_Glands_1.jpg Definition Diseases of the Adrenal Glands • Diseases of the Adrenal Glands are conditions that interfere with the normal functioning of the adrenal glands and may cause hyperfunction (Overactive Adrenal Glands) or hypofunction (Underactive Adrenal Glands), and may be congenital or acquired. • There are two parts of the adrenal glands, the cortex, derived from mesenchymal cells, and the medulla, derived from neuroectodermal cells; first one produces mineralocorticoids, glucocorticoids, and androgens; and second one produces epinephrine (adrenaline) and norepinephrine(noradrenaline). https://en.wikipedia.org/wiki/Adrenal_gland_disorder Epidemiology Epidemiologic study of adrenal gland disorders in Japan • The total numbers of patients in Japan in 1997 were estimated as 1,450 -
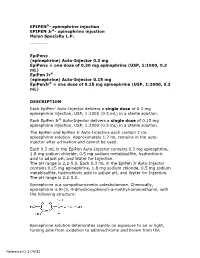
Epipen Injection Label
EPIPEN®- epinephrine injection EPIPEN Jr®- epinephrine injection Mylan Specialty L.P. ---------- EpiPen® (epinephrine) Auto-Injector 0.3 mg EpiPen® = one dose of 0.30 mg epinephrine (USP, 1:1000, 0.3 mL) EpiPen Jr® (epinephrine) Auto-Injector 0.15 mg EpiPenJr® = one dose of 0.15 mg epinephrine (USP, 1:2000, 0.3 mL) DESCRIPTION Each EpiPen® Auto-Injector delivers a single dose of 0.3 mg epinephrine injection, USP, 1:1000 (0.3 mL) in a sterile solution. Each EpiPen Jr® Auto-Injector delivers a single dose of 0.15 mg epinephrine injection, USP, 1:2000 (0.3 mL) in a sterile solution. The EpiPen and EpiPen Jr Auto-Injectors each contain 2 mL epinephrine solution. Approximately 1.7 mL remains in the auto- injector after activation and cannot be used. Each 0.3 mL in the EpiPen Auto-Injector contains 0.3 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Each 0.3 mL in the EpiPen Jr Auto-Injector contains 0.15 mg epinephrine, 1.8 mg sodium chloride, 0.5 mg sodium metabisulfite, hydrochloric acid to adjust pH, and Water for Injection. The pH range is 2.2-5.0. Epinephrine is a sympathomimetic catecholamine. Chemically, epinephrine is B-(3, 4-dihydroxyphenyl)-a-methyl-aminoethanol, with the following structure: Epinephrine solution deteriorates rapidly on exposure to air or light, turning pink from oxidation to adrenochrome and brown from the Reference ID: 3176782 formation of melanin. -
Patients on Beta-Blockers
Systemic Allergic & Immunoglobulin Disorders Bryan L. Martin, DO, MMAS, FACAAI, FAAAAI, FACP, FACOI Emeritus Professor of Medicine and Pediatrics President, American College of Allergy, Asthma & Immunology Disclosures . None 2 Objectives . Pass the boards! . Recognize anaphylaxis and understand the new guidelines for the treatment of anaphylaxis . Compare and contrast anaphylactic and anaphylactoid reactions 3 The Patient . 45 year old woman goes to lunch with her friends . While eating she develops GI upset, dizziness, shortness of breath and hives . Her friends drive her to your nearby clinic Initial Evaluation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating a shrimp salad. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Anaphylaxis presentation . Your nurse gets the history of sudden onset of GI upset, dizziness, shortness of breath and hives while eating lunch. The patient now has audible wheezing, tachycardia, and a blood pressure of 110/60 . Your initial response . Take a detailed history of everything the patient had to eat for lunch . Ask if she has a history of any medical issues such as asthma, diabetes or heart disease . Give nebulized beta agonist . Give 50 mg of oral diphenhydramine . Give 0.3 ml of IM epinephrine Initial Response to anaphylaxis . -

Diphenhydramine (Systemic) Epinephrine (Systemic)
DIPHENHYDRAMINE (SYSTEMIC) ^ Diphenhist [OTC] see DiphenhydrAMINE (Systemic) on page 34 Insomnia, occasional: Oral: Children 2 to 12 years, weighing 10 to 50 kg (off-label use): DiphenhydrAMINE (Systemic) Limited data available: 1 mg/kg administered 30 minutes before bedtime; maximum single dose: 50 mg (Russo, 1976) Brand Names: US Aler-Dryl [OTC]; Allergy Relief Childrens Children ≥12 years and Adolescents: Refer to adult dosing. [OTC]; Allergy Relief [OTC]; Altaryl [OTC]; Anti-Hist Allergy [OTC]; Motion sickness: Banophen [OTC]; Benadryl Allergy Childrens [OTC]; Benadryl Prophylaxis: Oral: Allergy [OTC]; Benadryl Dye-Free Allergy [OTC]; Benadryl [OTC]; Manufacturer's labeling: Infants, Children, and Adolescents: Complete Allergy Medication [OTC]; Complete Allergy Relief [OTC]; Note: Administer 30 minutes before motion Dicopanol FusePaq; Dicopanol RapidPaq; Diphen [OTC]; Diphenh- Weight-directed dosing: 5 mg/kg/day divided into 3 to 4 doses; ist [OTC]; Genahist [OTC]; Geri-Dryl [OTC]; GoodSense Allergy maximum: 300 mg daily Relief [OTC]; Naramin [OTC]; Nighttime Sleep Aid [OTC]; Nytol Fixed dosing: 12.5 to 25 mg 3 to 4 times daily Maximum Strength [OTC]; Nytol [OTC]; Ormir [OTC]; PediaCare Alternate dosing: Children 2 to 12 years: Limited data available: Childrens Allergy [OTC]; Pharbedryl; Pharbedryl [OTC]; Q-Dryl 0.5 to 1 mg/kg/dose every 6 hours; maximum single dose: [OTC]; QlearQuil Nighttime Allergy [OTC]; Quenalin [OTC] [DSC]; 25 mg. First dose should be administered 1 hour before travel Scot-Tussin Allergy Relief [OTC]; Siladryl -

A Case of Waterhouse-Friderichsen Syndrome in a Patient with Streptococcus Pyogenes Bacteremia
A Case of Waterhouse-Friderichsen Syndrome in a Patient with Streptococcus Pyogenes Bacteremia D. I. BACAL, B. E. CATALDO, P. M. LUCERI, G. VARALLO Rowan University School of Osteopathic Medicine, and Jefferson University Hospital System, NJ INTRODUCTION Waterhouse-Friderichsen Syndrome (WFS) is a rare condition of adrenal insufficiency (AI) due to adrenal hemorrhage after a severe infection. The incidence of WFS has been estimated at 0.14-1.8% based on post-mortem studies.1 It has been associated with a 55-60% mortality rate.2 Meningococcal disease comprises up to 80% of WFS, but additional causative agents continue to be identified.3 This is the case of a 52-year-old female with toxic shock syndrome from Group A Streptococcal (GAS) bacteremia who developed bilateral adrenal hemorrhage & subsequent AI. Septic shock occurred during an initial hospitalization & resolved. Four weeks after discharge she presented with evidence of an adrenal crisis. CT scans demonstrated bilateral adrenal enlargement concerning for adrenal hemorrhage. Primary AI was confirmed via ACTH stimulation testing. A literature search found fewer than ten cases of WFS described due to streptococcal bacteremia. BACKGROUND OF WATERHOUSE-FRIDERICHSEN SYNDROME CONCLUSIONS • Bilateral adrenal hemorrhage has multiple causes: coagulopathies, sepsis from infection, hypotension (i.e. MI), severe volume loss, or surgical WFS is a rare, often fatal, clinical condition that can develop after a intervention 4 severe infection & leads to adrenal hemorrhage. Many factors • Signs include pallor, weakness, fatigue, anorexia, nausea, vomiting, and lethargy 5,6 & labs often depict hyponatremia & hyperkalemia contribute to the pathogenicity of WFS, including coagulopathy, • Increased skin pigmentation develops due to an increase in proopiomelanocortin (POMC), Bacterial ischemia & bacterial toxins.