Effect of Submucosal Midazolam on Behavior and Physiologic Response When Combined with Oral Chloral Hydrate and Nitrous Oxide Sedation Gary R
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Midazolam Injection, USP
Midazolam Injection, USP 2 mg per 2 mL | NDC 70860-600-02 50 mg per 10 mL | NDC 70860-601-10 ATHENEX AccuraSEETM PACKAGING AND LABELING BIG, BOLD AND BRIGHT — TO HELP YOU SEE IT, SAY IT AND PICK IT RIGHT DIFFERENTIATION IN EVERY LABEL, DESIGNED TO HELP REDUCE MEDICATION ERRORS PLEASE SEE FULL PRESCRIBING INFORMATION, INCLUDING BOXED WARNING, FOR MIDAZOLAM INJECTION, USP, ENCLOSED. THE NEXT GENERATION OF PHARMACY INNOVATION To order, call 1-855-273-0154 or visit www.Athenexpharma.com Midazolam Injection, USP 2 5 mg NDC 70860-600-02 0 NDC 70860-601-10 2 mg per 2 mL mg 50 mg per 10 mL DESCRIPTION Glass Vial DESCRIPTION Glass Vial CONCENTRATION 1 mg per mL CONCENTRATION 5 mg per mL CLOSURE 13 mm CLOSURE 20 mm UNIT OF SALE 25 vials UNIT OF SALE 10 vials BAR CODED Yes BAR CODED Yes STORAGE Room Temp. STORAGE Room Temp. • AP RATED • PRESERVATIVE-FREE • AP RATED • NOT MADE WITH NATURAL RUBBER LATEX • NOT MADE WITH NATURAL RUBBER LATEX CHOOSE AccuraSEETM FOR YOUR PHARMACY Our proprietary, differentiated and highly-visible label designs can assist pharmacists in accurate medication selection. With a unique label design for every Athenex product, we’re offering your pharmacy added AccuraSEE. The idea is simple: “So what you see is exactly what you get.” Athenex, AccuraSEE and all label designs are copyright of Athenex. ©2020 Athenex. 000527 To order, call 1-855-273-0154 or visit www.Athenexpharma.com • Midazolam hydrochloride mufti-dose vial, is not intended for intrathecal or epidural • Anesthetic and sedation drugs are a necessary part of the care of children needing Midazolam Injection, USP administration, and is contraindicated for use in premature infants, because the formulation surgery, other procedures, or tests that cannot be delayed, and no specific medications INDICATIONS AND USAGE contains benzyl alcohol as a preservative. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -
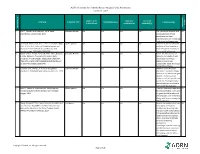
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures
Volume 2- Issue 1 : 2018 DOI: 10.26717/BJSTR.2018.02.000695 Eduardo de Oliveira Duque-Estrada. Biomed J Sci & Tech Res ISSN: 2574-1241 Mini Review Open Access The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures Eduardo de Oliveira Duque-Estrada MD* Received: January 17, 2018; Published: January 25, 2018 *Corresponding author: Eduardo de Oliveira Duque-Estrada, Ex-Professor of Pediatrics and Pediatric Surgery, Teresópolis Schoolof Medicine, Rio de Janeiro, Rua Jose da Silva Ribeiro 119 apt 11 São Paulo, SP Brazil CEP: 05726-130, Email: Abstract The local anesthetics are widely u sed in minor pediatric surgical procedures. The major problem with their use is the resulted pain experienced by the patients at the time of injection. To discuss those situations in the light of the medical literature we present this mini-review. Key words: Local Injection; Pain; Buffer; pH; Lidocaine; Pediatric Surgery Procedure Introduction Table 1: Techniques for injection pain control*. a eutectic mixture of lidocaine and prilocaine (EMLA) cream [17] S.No Techniques for injection pain control before infiltration, and local external cooling (cryoanalgesia) have 1. Warming the anesthetic solution [18,19] (Table 1). also been used to reduce the pain of infiltration of local anesthetic 2. Buffering the anesthetic Buffering the Anesthetic 3. Injection technique 4. Distraction Local anesthesia is extremely useful either as the sole method the best results on the minor surgery in general [3,6]. Blocking 5. Combination anesthetic technique the pain pathway with local anesthetic solution will also reduce 6. Cooling of skin the family stress response to the surgical procedure. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC). -
Local Anesthesia for Carpal Tunnel Surgery
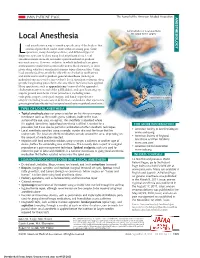
JAMA PATIENT PAGE The Journal of the American Medical Association ANESTHESIOLOGY Administration of local anesthetic Local Anesthesia for carpal tunnel surgery ocal anesthesia is a way to numb a specific area of the body so that a medical procedure can be done without causing pain. Some Loperations, many dental procedures, and different types of diagnostic tests can be done using local anesthesia alone. Local anesthesia medications do not make a person sedated or produce unconsciousness. However, sedation, in which individuals are given medications to make them comfortable and to block memory, is often given along with local anesthesia for many types of procedures. Using local anesthesia alone avoids the side effects of sedation medications and medications used to produce general anesthesia (making an individual unconscious for a procedure). Local anesthetic solutions often provide long-lasting pain relief to the area where they have been applied. Many operations, such as appendectomy (removal of the appendix), cholecystectomy (removal of the gallbladder), and open heart surgery, require general anesthesia. Other procedures, including some orthopedic surgery, urological surgery, and female reproductive Carpal tunnel surgery surgery (including most cesarean deliveries), can be done after a person is given regional anesthesia (such as spinal anesthesia or epidural anesthesia). TYPES OF LOCAL ANESTHESIA • Topical anesthesia places or sprays a solution on the skin or a mucous membrane (such as the mouth, gums, eardrum, inside of the nose, surface of the eye, anus, or vagina). The anesthetic is absorbed where it is applied. Sometimes topical local anesthesia is all that is needed for a FOR MORE INFORMATION procedure, but it can also be part of a combination of other anesthetic techniques. -

Veterinary Anesthesia and Pain Management Secrets / Edited by Stephen A
Publisher: HANLEY & BELFUS, INC. Medical Publishers 210 South 13th Street Philadelphia, PA 19107 (215) 546-7293; 800-962-1892 FAX (215) 790-9330 Web site: http://www.hanleyandbelfus.com Note to the reader Although the information in this book has been carefully reviewed for cor rectness of dosage and indications, neither the authors nor the editor nor the publisher can accept any legal responsibility for any errors or omissions that may be made. Neither the publisher nor the editor makes any warranty, expressed or implied, with respect to the material contained herein. Before prescribing any drug. the reader must review the manu facturer's correct product information (package inserts) for accepted indications, absolute dosage recommendations. and other information pertinent to the safe and effective use of the product described. This is especially important when drugs are given in combination or as an adjunct to other forms of therapy Library of Congress Cataloging-in-Publication Data Veterinary anesthesia and pain management secrets / edited by Stephen A. Greene. p. em. - (The Secrets Series®) Includes bibliographical references (p.). ISBN 1-56053-442-7 (alk paper) I. Veterinary anesthesia-Examinations, questions. etc. 2. Pain in animals Treatment-Examinations, questions, etc. I. Greene, Stephen A., 1956-11. Series. SF914.V48 2002 636 089' 796'076--dc2 I 2001039966 VETERINARY ANESTHESIA AND PAIN MANAGEMENT SECRETS ISBN 1-56053-442-7 © 2002 by Hanley & Belfus, Inc. All rights reserved. No part of this book may be repro duced, reused, republished. or transmitted in any form, or stored in a database or retrieval system, without written permission of the publisher Last digit is the print number: 9 8 7 6 5 4 3 2 CONTRIBUTORS G. -

The Emergence of New Psychoactive Substance (NPS) Benzodiazepines
Issue: Ir Med J; Vol 112; No. 7; P970 The Emergence of New Psychoactive Substance (NPS) Benzodiazepines. A Survey of their Prevalence in Opioid Substitution Patients using LC-MS S. Mc Namara, S. Stokes, J. Nolan HSE National Drug Treatment Centre Abstract Benzodiazepines have a wide range of clinical uses being among the most commonly prescribed medicines globally. The EU Early Warning System on new psychoactive substances (NPS) has over recent years detected new illicit benzodiazepines in Europe’s drug market1. Additional reference standards were obtained and a multi-residue LC- MS method was developed to test for 31 benzodiazepines or metabolites in urine including some new benzodiazepines which have been classified as New Psychoactive Substances (NPS) which comprise a range of substances, including synthetic cannabinoids, opioids, cathinones and benzodiazepines not covered by international drug controls. 200 urine samples from patients attending the HSE National Drug Treatment Centre (NDTC) who are monitored on a regular basis for drug and alcohol use and which tested positive for benzodiazepine class drugs by immunoassay screening were subjected to confirmatory analysis to determine what Benzodiazepine drugs were present and to see if etizolam or other new benzodiazepines are being used in the addiction population currently. Benzodiazepine prescription and use is common in the addiction population. Of significance we found evidence of consumption of an illicit new psychoactive benzodiazepine, Etizolam. Introduction Benzodiazepines are useful in the short-term treatment of anxiety and insomnia, and in managing alcohol withdrawal. 1 According to the EMCDDA report on the misuse of benzodiazepines among high-risk opioid users in Europe1, benzodiazepines, especially when injected, can prolong the intensity and duration of opioid effects. -

Local Anesthetic Agents Infiltration: Role of the Nurse
Doug Ducey Joey Ridenour Governor Executive Director Arizona State Board of Nursing 1740 W Adams Street, Suite 2000 Phoenix. AZ 85007 Phone (602) 771-7800 Home Page: http://www.azbn.gov OPINION: INFILTRATION OF LOCAL An advisory opinion adopted by AZBN is an interpretation of what the law requires. While an ANESTHETIC AGENTS: THE ROLE OF THE advisory opinion is not law, it is more than a recommendation. In other words, an advisory opinion NURSE is an official opinion of AZBN regarding the practice of nursing as it relates to the functions of APPROVED DATE: 3/2015 nursing. Facility policies may restrict practice further in their setting and/or require additional REVISED DATE: 7/2018 expectations related to competency, validation, training, and supervision to assure the safety of their patient population and or decrease risk. ORIGINATING COMMITTEE: SCOPE OF PRACTICE COMMITTEE Within the Scope of Practice of X RN x LPN ADVISORY OPINION LOCAL ANESTHETIC AGENTS INFILTRATION: ROLE OF THE NURSE It is within the scope of practice of a registered nurse (RN) and a licensed practical nurse (LPN) to administer certain local anesthetic agents intradermal, subcutaneous, and submucosal for the purposes of analgesia and/or anesthesia prior to potentially painful procedures. Tumescent lidocaine infiltration for ambulatory procedures, such as but not limited to, the treatment of hyperhidrosis, ambulatory phlebectomy and laser facial resurfacings would be within the RN scope under the direction of an licensed independent practitioner (LIP) and when certain criteria is met within this advisory opinion. The licensed nurse must meet the general requirements and course of instruction listed in parts I and II. -

Script For: Local Anesthetic Agents Surgery 101 Podcast Department of Surgery University of Alberta
Script for: Local Anesthetic Agents Surgery 101 Podcast Department of Surgery University of Alberta By Urooj Siddiqui Med 4 University of Alberta Hello, and welcome to another episode of Surgery 101. My name is Urooj Siddiqui, and I am pleased to be serving as a guest host this week! I am a fourth year University of Alberta Medical student just recently finishing an anesthesia elective here at the UofA. I’d like to recognize and thank Dr. Ronald Cheng for his input and feedback on this podcast. The objectives of this podcast are to: • Describe the pharmacology of local anesthetics • Look at the different types of local anesthetics • Highlight the different techniques used in local anesthesia • Outline the toxicities associated with common local anesthetic agents • Recognize the indications for and against the use of local anesthetics How many of you have ever had to get stitches, a tooth pulled or a small lump removed? Needless to say these would all be very painful procedures were it not for some local anesthetic. When applied to nerves, local anesthetics block the generation and propagation of action potentials. This essentially induces an absence of sensation in the nerve's distribution distal to the point of application. In regional anesthesia, local anesthetics are applied to large nerves or near the spinal cord to provide diminished sensation to a large area – such as a limb or lower segment of the body. If a small discrete portion of the body (i.e. tooth or incision/laceration) needs to be "frozen", the local anesthetics are applied more distally. -

The Waterloo Wellington Palliative Sedation Protocol
The Waterloo Wellington Palliative Sedation Protocol Waterloo Wellington Interdisciplinary HPC Education Committee; PST Task Force Chair: Dr. Deborah Robinson MD CCFP(F), Focused practice in Oncology and Palliative Care Co-chairs: Cathy Joy, Palliative Care Consultant, Waterloo Region Chris Bigelow, Palliative Care Consultant, Wellington County Revision due: November 2016 Last revised and activated: November 13, 2013 Committee responsible for revisions: WW Interdisciplinary HPC Education Committee Table of Contents Purpose and Definitions .................................................................................................................... 2 Indications for the use of PST .............................................................................................................. 3 Criteria for Initiation of PST ............................................................................................................... 4 Process ............................................................................................................................................. 4 Documentation for Initiation of PST .................................................................................................. 5 Medications ......................................................................................................................................... 6 1st Line (Initiating PST) ...................................................................................................................... 6 2nd Line (When 1st -

Important Clinical Factors Related to Local Anesthesia
ENDODONTICS: Colleagues for Excellence Winter 2009 Bonus Material A IMPORTANT CLINICAL FACTORS RELATED TO LOCAL ANESTHESIA Before reviewing the specifics of local anesthesia, we would like to provide an overview of some factors that are important to clinical anesthesia. How do we traditionally confirm anesthesia clinically? Traditional methods to confirm anesthesia usually involve questioning the patient (“Is your lip numb?ʺ), soft tissue testing (e.g., lack of mucosal responsiveness to a sharp explorer) or simply commencing with treatment. The problem with these approaches is they may not be effective for determining pulpal anesthesia.1‐4 Objective means of determining pulpal anesthesia in nonpainful, vital teeth. A more objective measurement of anesthesia, in nonpainful vital teeth, is obtained with an application of a cold refrigerant or by using an electric pulp tester. Clinically, application of cold or the electric pulp tester can be used to test the tooth under treatment for pulpal anesthesia prior to beginning a clinical procedure.5‐10 Determining pulpal anesthesia in painful, vital teeth. However, in painful, vital teeth (e.g., irreversible pulpitis), the lack of response to pulp testing may not guarantee pulpal anesthesia even if there is vital tissue present in the pulp chamber.5, 9, 10 Therefore, if a patient experiences pain when the endodontic procedure is started, after negative pulp testing, supplemental anesthesia is indicated. Naturally, if the chamber is necrotic and the canals are vital, no objective test can predict the level of clinical anesthesia. However, as suggested by Hsiao‐Wu, et al.10, cold testing adjacent teeth for anesthesia may provide evidence of anesthesia in the working area.