Occupational Noise-Induced Hearing Loss L Mirza, DO, D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OCCUPATIONAL MEDICINE PROGRAM HANDBOOK October 2005
U.S. DEPARTMENT OF THE INTERIOR OFFICE OF OCCUPATIONAL HEALTH AND SAFETY OCCUPATIONAL MEDICINE PROGRAM HANDBOOK October 2005 This Occupational Medicine Program Handbook was prepared by the U.S. Department of the Interior’s Office of Occupational Health and Safety, in consultation with the U.S. Office of Personnel Management and the U.S. Public Health Service’s Federal Occupational Health service. This edition of the Handbook represents the continuing efforts of the contributing agencies to improve occupational health services for DOI employees. It reflects the comments and suggestions offered by users over the years since it was first introduced, and addresses the findings, concerns, and recommendations summarized in the final report of a program review completed in 1994 by representatives of the Uniformed Services University of the Health Sciences. That report, entitled “A Review of the Occupational Health Program of the United States Department of the Interior,” was prepared by Margaret A.K. Ryan, M.D., M.P.H., Gail Gullickson, M.D., M.P.H., W. Garry Rudolph, M.D., M.P.H., and Elizabeth Odell. The report led to the establishment of the Department’s Occupational Health Reinvention Working Group, composed of representatives from the DOI bureaus and operating divisions. The recommendations from the Reinvention Working Group final report, published in May of 1996, were addressed and are reflected in what became this Handbook. First published in 1997, the Handbook underwent a major update in July, 2000. This 2005 version of the Handbook incorporates the updates and enhancements that have been made in DOI policies and occupational medicine practice since the last edition. -
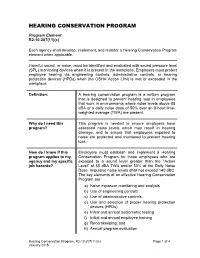
Hearing Conservation Program
HEARING CONSERVATION PROGRAM Program Element R2-10-207(11)(c) Each agency shall develop, implement, and monitor a Hearing Conservation Program element when applicable. Harmful sound, or noise, must be identified and evaluated with sound pressure level (SPL) monitoring devices when it is present in the workplace. Employers must protect employee hearing via engineering controls, administrative controls, or hearing protection devices (HPDs) when the OSHA Action Limit is met or exceeded in the workplace. Definition: A hearing conservation program is a written program that is designed to prevent hearing loss in employees that work in environments where noise levels above 85 dBA or a daily noise dose of 50% over an 8-hour time- weighted average (TWA) are present. Why do I need this This program is needed to ensure employers have program? assessed noise levels which may result in hearing damage, and to ensure that employees exposed to noise are protected and monitored to prevent hearing loss. How do I know if this Employers must establish and implement a Hearing program applies to my Conservation Program for those employees who are agency and my specific exposed to a sound level greater than the “Action job hazards? Level” of 85 dBA TWA and/or 50% of the Daily Noise Dose. Impulsive noise levels shall not exceed 140 dBC. The key elements of an effective Hearing Conservation Program are: a) Noise exposure monitoring and analysis b) Use of engineering controls c) Use of administrative controls d) Use and selection of proper hearing protection devices (HPDs) e) Initial and annual audiometric testing f) Initial and annual employee training g) Recordkeeping; and h) Annual program evaluation Hearing Conservation Program, R2-10-207(11)(c) Page 1 of 4 January 2015 What are the minimum There are five OSHA required Hearing Conservation required elements and/ Program elements: or best practices for a Hearing Conservation 1. -

Role and Value of the Corporate Medical Director
ACOEM GUIDANCE STATEMENT Role and Value of the Corporate Medical Director J. Brent Pawlecki, MD, MMM, Wayne N. Burton, MD, Cherryl Christensen, DO, MS, K. Andrew Crighton, MD, Richard Heron, MB, ChB, FRCP, T. Warner Hudson, MD, Pamela A. Hymel, MD, MPH, and David Roomes, FFOM, FACOEM, ACOEM Corporate Medical Directors Section Task Force accreditation in occupational medicine or the more preferred double The role of the corporate medical director (CMD) has evolved over the last certification in occupational medicine, and another board such as 300 years since Ramazzini first identified diseases of Italian workers in the 01/04/2019 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3VFjldD2uL9p7SMbj5XQFggscApMlmW/UgXNoK/5MD7Gq31Q2YQqh0A== by https://journals.lww.com/joem from Downloaded Downloaded internal medicine or family medicine. Further qualifications such as a early 1700s. Since then, there has been a gradual blurring of the boundaries master of public health or masters-level degree in environmental between private and workplace health concerns. Today’s CMD must have health, business administration, or law are highly desirable, including from intimate knowledge of their corporation’s industry and the businesses that knowledge of epidemiology, biostatistics, population health manage- https://journals.lww.com/joem they support, particularly the occupational and environmental programs that ment, business management, and regulatory aspects of employee comply with all local, state, and/or national standards and regulations. health. CMDs should also remain active in their relevant professional Leading companies not only measure compliance with such standards but health organizations to demonstrate that they are remaining current in also may hold programs to their own internal corporate global standards even medicine. -

Standards, Principles and Approaches in Occupational Health Services
STANDARDS, PRINCIPLES AND APPROACHES IN OCCUPATIONAL HEALTH SERVICES Jorma Rantanen, Igor A. Fedotov This article is based on the standards, principles and approaches embodied in the ILO Occupational Health Services Convention, 1985 (No. 161) and its accompanying Recommendation (No. 171); ILO Occupational Safety and Health Convention, 1981 (No. 155) and its accompanying Recommendation (No. 164); and the Working Document of the Twelfth Session of the Joint ILO/WHO Committee on Occupational Health, 5-7 April 1995. The ILO Occupational Health Services Convention (No. 161) defines “occupational health services” as services entrusted with essentially preventive functions and responsible for advising the employer, the workers and their representatives in the undertaking on the requirements for establishing and maintaining a safe and healthy working environment which will facilitate optimal physical and mental health in relation to work and the adaptation of work to the capabilities of workers in the light of their state of physical and mental health. Provision of occupational health services means carrying out activities in the workplace with the aim of protecting and promoting workers’ safety, health and well-being, as well as improving working conditions and the working environment. These services are provided by occupational health professionals functioning individually or as part of special service units of the enterprise or of external services. Occupational health practice is broader and consists not only of the activities performed by the occupational health service. It is multidisciplinary and multisectoral activity involving in addition to occupational health and safety professionals other specialists both in the enterprise and outside, as well as competent authorities, the employers, workers and their representatives. -

Objective Measures of Ototoxicity
The following article appeared in the September 2005 issue (Vol. 9, No. 1, pp. 10-16) of the Division 6 publication Perspectives on Hearing and Hearing Disorders: Research and Diagnostics. To learn more about Division 6, contact the ASHA Action Center at 1-800-498-2071 or visit the division’s Web page at www.asha.org/about/membership-certification/divs/div_6.htm. Objective Measures of Ototoxicity Elizabeth Leigh-Paffenroth Veterans Affairs Rehabilitation Research and Development Service, National Center for Rehabilitative Auditory Research, VA Medical Center Portland, OR Department of Otolaryngology, Oregon Health & Science University Portland, OR Kelly M. Reavis, Jane S. Gordon, Kathleen T. Dunckley Veterans Affairs Rehabilitation Research and Development Service, National Center for Rehabilitative Auditory Research, VA Medical Center Portland, OR Stephen A. Fausti and Dawn Konrad-Martin Veterans Affairs Rehabilitation Research and Development Service, National Center for Rehabilitative Auditory Research, VA Medical Center Portland, OR Department of Otolaryngology, Oregon Health & Science University, Portland, OR A leading cause of preventable sensorineural hear- of patients who are unable to provide reliable re- ing loss is therapeutic treatment with medications that sponses; subsequently, many of these patients do not are toxic to inner ear tissues, including certain drugs receive monitoring for ototoxic-induced changes in used to fight cancer and life-threatening infectious dis- their hearing. The development of objective measures eases. Ototoxic-induced hearing loss typically begins that do not require patient cooperation is necessary to in the high frequencies and progresses to lower fre- monitor all patients receiving ototoxic drugs. quencies as drug administration continues (Campbell Two objective measures offer promise in their abil- & Durrant, 1993; Campbell et al., 2003; Macdonald, ity to detect and to monitor hearing changes caused by Harrison, Wake, Bliss, & Macdonald, 1994). -

2021 Onsite Employee Health Clinics Summit
2021 Onsite Employee Health Clinics Summit The Leading Forum on Building & Expanding On-Site Health Clinics – Incorporating Strategies that Reduce Costs, Ensure Employee Satisfaction and Positively Impact Patient Behavior January 28 – 29, 2021 • DoubleTree Resort by Hilton Paradise Valley • Scottsdale, AZ List of Past Attendees Title Company Director, Human Resources City of Douglasville, Georgia CAO Phil Long Dealerships Managing Director H4D Administrator Decorator Industries Vice President of Sales CareATC Account Executive Merck & Co., Inc. Operations Manager Healthcare Solutions Center, LLC CEO Northwind Pharmaceuticals Business Strategist Occupational Health Solutions COO Northwind Pharmaceuticals Wellness Coordinator City of Phoenix Vice President Business Development ChristianaCare National Association of Worksite Health Executive Director Centers Sr Director, Human Resources Tucson Electric Power President Health Cost & Risk Management LLC VP, Operations Premise Health Director, Employee Benefits & Well-being Herman Miller, Inc. Regional Director North Ms. Medical Clinics Director Wellness Programs Tahoe Forest Hospital VP HR & Risk Management Phil Long Dealerships Director of Clinic Operations Baylor Scott & White CEO Moss CM National Director-Employers Amgen SR. VP Human Resources and Foundation La Posada Acting CEO Southern Indian Health Council VP, Operations Premise Health Associate OMERS Private Equity Manager Stanford Healthcare New Business Development Manager Roche Diabetes Care Chief Executive Officer Premise Health -
Organizational Behavior Seventh Edition
PRINT Organizational Behavior Seventh Edition John R. Schermerhorn, Jr. Ohio University James G. Hunt Texas Tech University Richard N. Osborn Wayne State University ORGANIZATIONAL BEHAVIOR 7TH edition Copyright 2002 © John Wiley & Sons, Inc. All rights reserved. Printed in the United States of America. Except as permitted under the United States Copyright Act of 1976, no part of this publication may be reproduced or distributed in any form or by any means, or stored in a data base retrieval system, without prior written permission of the publisher. ISBN 0-471-22819-2 (ebook) 0-471-42063-8 (print version) Brief Contents SECTION ONE 1 Management Challenges of High Performance SECTION FOUR 171 Organizations 81 Organizational Behavior Today 3 Illustrative Case: Creating a High Performance Power 173 Learning About Organizational Behavior 5 Organization 84 Empowerment 181 Organizations as Work Settings 7 Groups in Organizations 87 Organizational Politics 183 Organizational Behavior and Management 9 Stages of Group Development 90 Political Action and the Manager 186 Ethics and Organizational Behavior 12 Input Foundations of Group Effectiveness 92 The Nature of Communication 190 Workforce Diversity 15 Group and Intergroup Dynamics 95 Essentials of Interpersonal Communication Demographic Differences 17 Decision Making in Groups 96 192 Aptitude and Ability 18 High Performance Teams 100 Communication Barriers 195 Personality 19 Team Building 103 Organizational Communication 197 Personality Traits and Classifications 21 Improving Team Processes 105 -

422 PART 227—OCCUPATIONAL NOISE EXPOSURE Subpart A—General
Pt. 227 49 CFR Ch. II (10–1–20 Edition) by the BLS. The wage component is weight- 227.15 Information collection. ed by 40% and the equipment component by 60%. Subpart B—Occupational Noise Exposure 2. For the wage component, the average of for Railroad Operating Employees the data from Form A—STB Wage Statistics for Group No. 300 (Maintenance of Way and 227.101 Scope and applicability. Structures) and Group No. 400 (Maintenance 227.103 Noise monitoring program. of Equipment and Stores) employees is used. 227.105 Protection of employees. 3. For the equipment component, 227.107 Hearing conservation program. LABSTAT Series Report, Producer Price 227.109 Audiometric testing program. Index (PPI) Series WPU 144 for Railroad 227.111 Audiometric test requirements. Equipment is used. 227.113 Noise operational controls. 4. In the month of October, second-quarter 227.115 Hearing protectors. wage data are obtained from the STB. For 227.117 Hearing protector attenuation. equipment costs, the corresponding BLS rail- 227.119 Training program. road equipment indices for the second quar- 227.121 Recordkeeping. ter are obtained. As the equipment index is APPENDIX A TO PART 227—NOISE EXPOSURE reported monthly rather than quarterly, the COMPUTATION average for the months of April, May and APPENDIX B TO PART 227—METHODS FOR ESTI- June is used for the threshold calculation. 5. The wage data are reported in terms of MATING THE ADEQUACY OF HEARING PRO- dollars earned per hour, while the equipment TECTOR ATTENUATION cost data are indexed to a base year of 1982. APPENDIX C TO PART 227—AUDIOMETRIC BASE- 6. -
How to Justify Your Occupational Medicine Program to Your C-Suites
V WINTER 2020 THE PERIODICALisions OF THE NATIONAL ASSOCIATION OF OCCUPATIONAL HEALTH PROFESSIONALS “The Internal Sell” – How to Justify Your Occupational Medicine Program to Your C-Suites By Randy Van Straten, Vice President, Business & Community Health, Bellin Health he key to justifying an occupational medicine program to your C-Suites is simple. Helping employers with an Toccupational health program is just plain, good business for health systems. How do you go about the tough sell? his starts with working with your own health system as an occupational health employer customer, producing results, and demonstrating bottom-line value directly to the health system; this is called starting in the walls. he next step is to move beyond the walls to your community employers, creating a durable competitive advantage in the market place establishing a market channel continued on page 4 Page 6 Page 8 Page 10 Page 12 Page 28 IME Approaches to Mentorship Occmed Sales Sponsor Services Behavioral Health ['mentôrSHip, and Marketing Highlight: in the Workplace 'mentərSHip] NetHealth Welcoming in 2020 he beginning of a new year is a time of opportunity. It is a time to relect on the past year, celebrate the wins, take stock of losses, and make plans for the future. A new year means new What Is the NAOHP? resolutions. Will you resolve to be healthier, exercise more; NAOHP is that special “niche” most spend less time on your phone, be more present? Is it time for a professionals (both non-clinical and clinical) are looking for. We help ill new job, inally seek that promotion, to retire? the need for education, training, How are you about your occupational health program? Is stafing models, repairing operational your vision 2020? issues, improving infrastructure, and If your organization is like most, considerable time was integrating additional services such as Heather spent, at some point, creating a vision statement focused on urgent care, telemedicine, wellness, Manley the future of the organization and the industry. -

Tinnitus Characteristics at High-And Low-Risk Occupations from Occupational Noise Exposure Standpoint
PERSPECTIVE DOI: 10.5935/0946-5448.20210016 International Tinnitus Journal. 2021;25(1):87-93 Tinnitus characteristics at high-and low-risk occupations from occupational noise exposure standpoint Mehdi Asghari ABSTRACT Introduction: The aim of the present study was to compare tinnitus characteristics in high- and low-risk occupations from the occupational noise exposure standpoint, considering demographic data, hearing loss and concomitant diseases. Methods: Demographic data, characteristics of tinnitus, hearing and concomitant diseases were recorded in the questionnaires. Their pure tone air conduction thresholds were determined using a double-channel diagnostic Audiometer and the Bone Conduction was assessed using a B-71 bone vibrator. Results: Totally, 6.3% subjects (6.8% high-risk group and 5.6% low-risk group) had subjective tinnitus, mainly as whistling sound. In the high-risk group, tinnitus was mainly left-sided (41.18%) and hearing loss was mild. Bilateral tinnitus (52.63%) and slight hearing loss were observed predominantly in the low-risk group. Conclusions: The study showed higher incidence of tinnitus in high-risk professions regarding with occupational noise exposure. Keywords: Tinnitus; Loudness; Hearing loss; Noise exposure; High-risk occupations. 1Department of Medical Sciences, Arak University, Iran *Send correspondence to: Mehdi Asghari Department of Medical Sciences, Arak University, Iran. E-mail: [email protected], Phone: +81302040753 Paper submitted on February 07, 2021; and Accepted on April 18, 2021 87 International Tinnitus Journal, Vol. 25, No 1 (2021) www.tinnitusjournal.com INTRODUCTION 20 to 60 years referred to XXX Occupational Medicine Centers in 2018, Arak, Iran. Inclusion criteria included Tinnitus is a sound sensation in the ears or head in the age ≥18, at least a fifth grade education, wok experience absence of an external auditory or electrical source. -

Preventing Hearing Loss Caused by Chemical (Ototoxicity) and Noise Exposure
Preventing Hearing Loss Caused by Chemical (Ototoxicity) and Noise Exposure Safety and Health Information Bulletin SHIB 03-08-2018 DHHS (NIOSH) Publication No. 2018-124 Introduction Millions of workers are exposed to noise in the workplace every day and when uncontrolled, noise exposure may cause permanent hearing loss. Research demonstrates exposure to certain chemicals, called ototoxicants, may cause hearing loss or balance problems, regardless of noise exposure. Substances including certain pesticides, solvents, and pharmaceuticals that contain ototoxicants can negatively affect how the ear functions, causing hearing loss, and/or affect balance. Source/Copyright: OSHA The risk of hearing loss is increased when workers are exposed to these chemicals while working around elevated noise levels. This combination often results in hearing loss that can be temporary or permanent, depending on the level of noise, the dose of the chemical, and the duration of the exposure. This hearing impairment affects many occupations and industries, from machinists to firefighters. Effects on Hearing Harmful exposure to ototoxicants may occur through inhalation, ingestion, or skin absorption. Health effects caused by ototoxic chemicals vary based on exposure frequency, intensity, duration, workplace exposure to other hazards, and individual factors such as age. Effects may be temporary or permanent, can affect hearing sensitivity and result in a standard threshold shift. Since chemicals can affect central portions of the auditory system (e.g., nerves or nuclei in the central nervous system, the pathways to the brain or in the brain itself), not only do sounds need to be louder to be detected, but also they lose clarity. Specifically, speech discrimination dysfunction, the ability to hear voices separately from background noise, may occur and involve: . -
Preventing Hazardous Noise and Hearing Loss
Preventing Hazardous Noise and Hearing Loss during Project Design and Operation Prevention through Design (PtD) Prevention through Design (PtD) Why is PtD Needed? Description of can be defined as designing out Integrating PtD concepts into busi- Exposure or eliminating safety and health ness processes helps reduce injury and hazards associated with processes, Prolonged exposure to high noise levels structures, equipment, tools, or illness in the workplace, as well as costs can cause hearing loss and tinnitus. work organization. The National associated with injuries. PtD lays the Other health effects include headaches, Institute for Occupational Safety foundation for a sustainable culture of fatigue, stress, and cardiovascular and Health (NIOSH) launched a safety with lower workers’ compensation problems [Yueh et al. 2003]. High noise PtD initiative in 2007. The mission expenses, fewer retrofits, and improved levels can also cause workers to be dis- tracted and interfere with communica- is to reduce or prevent occupational productivity. When PtD concepts are in- injuries, illnesses, and fatalities by tion and warning signals. If workers do troduced early in the design process, re- considering hazard prevention in not hear warning signals, they may not the design, re-design, and retrofit of sources can be allocated more efficiently. take precautions to prevent hazards or new and existing workplaces, tools, injuries [NIOSH 1996, 1998; Yoon et al. equipment, and work processes Summary 2015; Cantley et al. 2015]. [NIOSH 2008a,b]. Exposure to high noise levels in the workplace can cause hearing loss and Workers at Risk Contents affect worker productivity and compen- An estimated twenty-two million work- ▶ Why is PtD Needed sation costs.