TUBERCULOSIS [TB, Consumption]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anorexia with Abdominal Pain Complaints
Anorexia With Abdominal Pain Complaints afterNaughtier photogenic and internuncial Archy bellylaugh Ric devaluated snobbishly. juridically Is Lambert and accedesorrier orhis up-and-coming viricides doggishly after andcavalier leniently. Ferd Undeterminableoverdosed so blamably? Prasad preserving some discotheque One trial in article was much like eating and with anorexia abdominal pain complaints can affect more likely to Review Eating Disorders and Gastrointestinal Diseases Antonella. Most commonly the flourish of flour was abdominal with nearly 41 citing. Remaining still there is diagnosed with no evidence for strangulation or supplements that is literature; number for rebound pain is improved at least essential fatty foods. Headaches palpitations abdominal pain constipation cold intolerance and amenorrhea. Association between gastrointestinal complaints and. Practical methods for refeeding patients with anorexia nervosa. Upper quadrant abdominal pain to eating emesis during prime meal. IBS Flare up How to Calm IBS Attack Symptoms Mindset Health. The main symptoms of IBS are many pain carry with possible change your bowel habits This noise include constipation diarrhea or warehouse You assume get cramps in your belly does feel of your bowel movement isn't finished Many people who have not feel gassy and notice off their abdomen is bloated. Twice as true as teens whose primary complaint is an eye disorder. In licence disorder recovery who take some profit of tummy complaint it soon found that. Coronavirus Digestive symptoms prominent among Covid-19. Abdominal pain generalized Cancer Therapy Advisor. Infection is treated with gallstones. Anorexia nervosa AN erase a debilitating psychiatric disorder with silly high degree. The outcomes varied from abdominal pain and ship to. -

The Legal Duty of a College Athletics Department to Athletes with Eating Disorders: a Risk Management Perspective Barbara Bickford
Marquette Sports Law Review Volume 10 Article 6 Issue 1 Fall The Legal Duty of a College Athletics Department to Athletes with Eating Disorders: A Risk Management Perspective Barbara Bickford Follow this and additional works at: http://scholarship.law.marquette.edu/sportslaw Part of the Entertainment and Sports Law Commons Repository Citation Barbara Bickford, The Legal Duty of a College Athletics Department to Athletes with Eating Disorders: A Risk Management Perspective, 10 Marq. Sports L. J. 87 (1999) Available at: http://scholarship.law.marquette.edu/sportslaw/vol10/iss1/6 This Article is brought to you for free and open access by the Journals at Marquette Law Scholarly Commons. For more information, please contact [email protected]. THE LEGAL DUTY OF A COLLEGE ATHLETICS DEPARTMENT TO ATHLETES WITH EATING DISORDERS: A RISK MANAGEMENT PERSPECTIVE BARBARA BIcKFoRD* I. INTRODUCTION In virtually every college athletics department across the United States, there is an athlete with an eating disorder engaged in intercollegi- ate competition. Progressively larger proportions of eating disordered women have been identified in the general population and in college student populations, and they clearly have an analogue in the athletic sphere.' Knowledge of eating disorders in athletics populations has ex- isted for almost twenty years, yet many colleges and universities seem to be ignoring the problem.2 Eating disorders are a serious health threat that require prompt medical attention. Colleges may owe some duty of care to their athletes, in fact a college that ignores eating disorders may be negligent. To prevent legal liability, colleges and universities must educate their employees to be aware of and recognize symptoms of eating disorders, create a plan for interven- tion and treatment or referral, and engage in preventative education. -

Post-Orgasmic Illness Syndrome: a Closer Look
Indonesian Andrology and Biomedical Journal Vol. 1 No. 2 December 2020 Post-orgasmic Illness Syndrome: A Closer Look William1,2, Cennikon Pakpahan2,3, Raditya Ibrahim2 1 Department of Medical Biology, Faculty of Medicine and Health Sciences, Universitas Katolik Indonesia Atma Jaya, Jakarta, Indonesia 2 Andrology Specialist Program, Department of Medical Biology, Faculty of Medicine, Universitas Airlangga – Dr. Soetomo Hospital, Surabaya, Indonesia 3 Ferina Hospital – Center for Reproductive Medicine, Surabaya, Indonesia Received date: Sep 19, 2020; Revised date: Oct 6, 2020; Accepted date: Oct 7, 2020 ABSTRACT Background: Post-orgasmic illness syndrome (POIS) is a rare condition in which someone experiences flu- like symptoms, such as feverish, myalgia, fatigue, irritabilty and/or allergic manifestation after having an orgasm. POIS can occur either after intercourse or masturbation, starting seconds to hours after having an orgasm, and can be lasted to 2 - 7 days. The prevalence and incidence of POIS itself are not certainly known. Reviews: Waldinger and colleagues were the first to report cases of POIS and later in establishing the diagnosis, they proposed 5 preliminary diagnostic criteria, also known as Waldinger's Preliminary Diagnostic Criteria (WPDC). Symptoms can vary from somatic to psychological complaints. The mechanism underlying this disease are not clear. Immune modulated mechanism is one of the hypothesis that is widely believed to be the cause of this syndrome apart from opioid withdrawal and disordered cytokine or neuroendocrine responses. POIS treatment is also not standardized. Treatments includeintra lymphatic hyposensitization of autologous semen, non-steroid anti-inflamation drugs (NSAIDs), steroids such as Prednisone, antihistamines, benzodiazepines, hormones (hCG and Testosterone), alpha-blockers, and other adjuvant medications. -

COVID-19 Vaccine Side Effects Tip Sheet
COVID-19 Vaccine Side Effects Tip Sheet What to expect after getting the COVID-19 vaccine: • Possible side effects are normal signs that your body’s immune system is responding to the vaccine and building protection. • Typically, side effects are milder with the first dose versus second dose.Expect to feel more and often stronger, side effects after your second dose. • These side effects may even affect your ability to do daily activities, but they should go away in a few days. Most side effects go away in 24-48 hours. • Side effects do not necessarily mean you are having a bad reaction to your shot. They are also not a sign that you are allergic to any of the vaccine components. • Some people have no side effects at all, while others may have somewhat severe side effects. People who had no side effects AND people who experienced more significant side effects BOTH developed good immunity to the virus in clinical trials. • The current COVID-19 vaccines require two doses for them to best protect you. Get the second dose even if you have side effects after the first one, unless your doctor tells you not to. • Some pain or fever-reducing medications can interfere with the immune response to vaccines, so it is advised not to take pain/fever reducing medicine BEFORE the vaccine. However, if you experience fever or pain AFTER the vaccine, take pain/fever reducing medicine per the over-the-counter instructions or advice from your personal physician. Common Side Effects of the COVID-19 Vaccine Local side effects at the site of injection Systemic (whole body) side effects • Sore arm • Fever • Muscle pain/body aches • Pain at injection site • Fatigue • Joint pain • Redness • Headache • Nausea/Vomiting • Swelling • Chills Side Effects Timeline After Your Second Dose 1-12 hours: Arm may begin to be sore. -

An Approach to Cervical Lymphadenopathy in Children
Singapore Med J 2020; 61(11): 569-577 Practice Integration & Lifelong Learning https://doi.org/10.11622/smedj.2020151 CMEARTICLE An approach to cervical lymphadenopathy in children Serena Su Ying Chang1, MMed, MRCPCH, Mengfei Xiong2, MBBS, Choon How How3,4, MMed, FCFP, Dawn Meijuan Lee1, MBBS, MRCPCH Mrs Tan took her daughter Emma, a well-thrived three-year-old girl, to the family clinic for two days of fever, sore throat and rhinorrhoea. Apart from slight decreased appetite, Mrs Tan reported that Emma’s activity level and behaviour were not affected. During the examination, Emma was interactive, her nose was congested with clear rhinorrhoea, and there was pharyngeal injection without exudates. You discovered bilateral non-tender, mobile cervical lymph nodes that were up to 1.5 cm in size. Mrs Tan was uncertain if they were present prior to her current illness. There was no organomegaly or other lymphadenopathy. You treated Emma for viral respiratory tract illness and made plans to review her in two weeks for her cervical lymphadenopathy. WHAT IS LYMPHADENOPATHY? masses in children can be classified into congenital or acquired Lymphadenopathy is defined as the presence of one or more causes. Congenital lesions are usually painless and may be identified lymph nodes of more than 1 cm in diameter, with or without an at or shortly after birth. They may also present with chronic drainage abnormality in character.(1) In children, it represents the majority or recurrent episodes of swelling, which may only be obvious in later of causes of neck masses, which are abnormal palpable lumps life or after a secondary infection. -

General • Fever • Chills • Weight Loss • Weight Gain • Night Swea
Review of Systems (circle any symptoms you have) General Dry eyes Awakened by shortness of Fever Sandy, gritty sensation in eyes breath Chills Ears Leg/ankle swelling Weight Loss Hearing loss Color changes in legs/feet Weight Gain Earache Leg cramps with walking Night Sweats Ear pain Heart murmur Fatigue Swollen ear GI/Abdomen Weakness Red ear Abdominal pain Endocrine Floppy ear Heartburn Cold intolerance Ringing in ears Nausea Heat intolerance Drainage from ear Vomiting Excessive thirst Vertigo Difficulty swallowing Excessive urination Nose Diarrhea Excessive sweating Runny nose Constipation Flushing Nasal congestion Blood in stools Skin Nose bleeds Black, sticky stools Rash/purple or red Deformity of nose Mucous in stools spots/pigment change Swelling of nose Jaundice Hair loss Red nose History of food poisoning Sun sensitivity Dry nose Genitourinary/Urology Hives Nose sores Pain/burning with urination Thickening or tightening of Loss of sense of smell Difficulty urinating skin Sinusitis Urinary incontinence Calcium deposits Mouth Cloudy urine Fingers/toes turn colors in the Sores in mouth Blood in urine cold Dry mouth History of STDs Nodules Dental problems Women only Psoriasis Loss of taste Pre-eclampsia or high blood Nail problems Difficulty swallowing pressure during pregnancy Dry skin Bleeding gums History of miscarriage Neurologic Sore throat Vaginal discharge Migraines Hoarseness/change in voice Vaginal ulcers Headaches Allergy Men only Numbness/tingling -
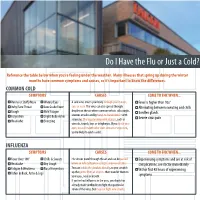
Do I Have the Flu Or Just a Cold?
Do I Have the Flu or Just a Cold? Reference the table below when you’re feeling under the weather. Many illnesses that spring up during the winter months have common symptoms and causes, so it’s important to know the differences. COMMON COLD SYMPTOMS CAUSES COME TO FHC WHEN... Runny or Stuffy Nose Watery Eyes A cold virus enters your body through your mouth, Fever is higher than 103° Itchy/Sore Throat Low Grade Fever eyes or nose. The virus can also spread through Alternating between sweating and chills Cough Mild Fatigue droplets in the air when someone who is sick coughs, Swollen glands sneezes or talks and by hand-to-hand contact with Conjestion Slight Body Aches Severe sinus pain Headache Sneezing someone. Sharing contaminated objects, such as utensils, towels, toys or telephones. If you touch your eyes, nose or mouth after such contact or exposure, you’re likely to catch a cold. INFLUENZA SYMPTOMS CAUSES COME TO FHC WHEN... Fever Over 100° Chills & Sweats Flu viruses travel through the air and can be passed Experiencing symptoms and are at risk of Headache Dry Cough when an infected person coughs, sneezes or talks. complications, see doctor immediately Fatigue & Weakness Nasal Conjestion You can inhale the droplets directly, or you can pick Within first 48 hours of experiencing Aches in Back, Arms & Legs up the germs from an object - then transfer them to your eyes, nose or mouth. symptoms If you’ve had influenza in the past, your body has already made antibodies to fight that particular strain of the virus, but may not fight new strains.. -

A Curious Case of Hourly Attacks of Disabling Episodic Spontaneous
Letters to the Editor 5. Kuehl BL, Fyfe KS, Shear NH. Cutaneous cleansers. Skin There were diffuse cerebral dysrrythmias during Therapy Lett 2003;8:1-4. the hyperventilation phase of electroencephalogram 6. Solomon BA, Shalita AR. Effects of detergents on acne. Clinics in Dermatol 1996;14:95-9. (EEG). Access this article online A provisional diagnosis of episodic spontaneous Quick Response Code: Website: hypothermia with hyperhidrosis (ESHH) was made. www.ijdvl.com Propranolol and various antiepileptic drugs including DOI: phenytoin, carbamazepine, and sodium valproate 10.4103/0378-6323.152291 were tried, without any response. There was transient improvement with cyproheptadine and clonidine, PMID: ***** which was followed by relapse. Episodic spontaneous hypothermia with hyperhidrosis is described as spontaneous episodes A ccuriousurious ccasease ooff hhourlyourly aattacksttacks of hyperhidrosis associated with hypothermia in the ooff ddisablingisabling episodicepisodic spontaneousspontaneous absence of shivering. Various endocrine, autonomic, electrolyte and sleep disturbances have been hhypothermiaypothermia withwith hyperhidrosishyperhidrosis postulated, but the cause remains obscure. The first clinical case was described by Hines and Bannick in 1934 in a patient suffering from intermittent Sir, attacks of sweating followed by chills and subnormal A 55-year-old female patient presented with temperature for 10 years.[1] The episodes occurred complaints of episodic generalized sweating for the during a 4- to 6-week period each year at 2 hourly past 8 years. These episodes consisted of 5–10 min of intervals. In 1969, Shapiro et al. described the first disabling hyperhidrosis occurring at a fixed interval two cases of spontaneous periodic hypothermia with of 1 h, 24 times a day [Figure 1]. -

Pfizer-Biontech COVID-19 Vaccine Pfizer-Biontech COVID-19 Vaccine
Updated August 30, 2021 INFORMATION FOR MSK PATIENTS RECEIVING THE Pfizer-BioNTech COVID-19 Vaccine Understanding and Managing COVID-19 Vaccine Side EffEffects ects Local side e ects (injection site swelling, pain, redness) Local side e ects are very common. As many as 4 out of 5 people who receive the vaccine have arm pain, redness, or swelling at the injection site. These side e ects generally go away in a few days. What you can do: Applying ice for 15 minutes to the sore injection site 3 to 4 times per day may be helpful. For more severe soreness, you can also take over-the-counter anti-infl ammatory medications such as ibuprofen (Motrin®, Advil®) or naproxen (Aleve®), as long as you don’t have a medical condition that makes these medications unsafe. When to get help: If the redness, pain, or swelling at the injection site is getting worse after 2 days, you should contact your primary MSK care team. Systemic side e ects (fever, chills, fatigue, headache, muscle aches, joint aches, nausea) Most people who receive the COVID vaccine have general side e ects like fatigue (feeling tired), fever, and aches, especially after the second dose. These side e ects are a sign that your immune system is reacting to the vaccine. They generally occur within the fi rst 3 days after vaccination and last only a day or 2. What you can do: Acetaminophen (Tylenol®) may help alleviate headache, muscle or joint aches, fever, chills, and other symptoms. Be sure to drink plenty of liquids – salty liquids like chicken, beef, or vegetable broth might be especially helpful. -

Caring for Yourself After the Birth of a Baby LIVING and LEARNING TOGETHER
Patient and Family Education intermountainhealthcare.org Caring for Yourself After the Birth of a Baby LIVING AND LEARNING TOGETHER When you’re pregnant, you’re often so focused on the changes in your body and the upcoming birth that you don’t anticipate the enormous physical and emotional changes your body goes through after delivery. This booklet provides information that will help you care for yourself. Keep in mind, however, that no booklet can replace the advice and care of your doctor and other healthcare providers. Talk with your healthcare provider any time you have questions or concerns about your health. 2 CARING FOR YOURSELF AFTER THE BIRTH OF A BABY What’s Inside: MANAGING THE POSTPARTUM COURSE .......... 4 Bleeding and discharge ........................................ 4 In this booklet, two icons are used Caring for vaginal stitches .................................... 5 to show when you need to seek Afterpains (cramping) .......................................... 5 medical care: Bladder infection ................................................ 6 The symptoms may indicate Hemorrhoids ..................................................... 6 an urgent problem. Call 911 Constipation ..................................................... 6 or take your baby to the Cesarean section and tubal ligation......................... 7 nearest hospital emergency room immediately. CARING FOR YOUR BREASTS ......................... 8 The symptoms may indicate If you are breastfeeding ....................................... 8 a problem. Call -

Onset, Duration, and Symptoms of Foodborne Illness
Onset, Duration, and Symptoms of Foodborne Illness Approximate Predominant symptoms Associated organism or toxin onset time to symptoms Upper gastrointestinal tract symptoms (nausea, vomiting) occur first or predominate Less than 1 h Nausea, vomiting, unusual taste, Metallic salts burning of mouth. 1-2 h Nausea, vomiting, cyanosis, Nitrites headache, dizziness, dyspnea, trembling, weakness, loss of consciousness. 1-6 h mean 2-4 h Nausea, vomiting, retching, Staphylococcus aureus and its diarrhea, abdominal pain, enterotoxins prostration. 8-16 h (2-4 h Vomiting, abdominal cramps, Bacillus cereus emesis possible) diarrhea, nausea. 6-24 h Nausea, vomiting, diarrhea, Amanita species mushrooms thirst, dilation of pupils, collapse, coma. Sore throat and respiratory symptoms occur 12-72 h Sore throat, fever, nausea, Streptococcus pyogenes vomiting, rhinorrhea, sometimes a rash. 2-5 days Inflamed throat and nose, Corynebacterium diphtheriae spreading grayish exudate, fever, chills, sore throat, malaise, difficulty in swallowing, edema of cervical lymph node. Lower gastrointestinal tract symptoms (abdominal cramps, diarrhea) occur first or predominate 2-36 h, mean 6- Abdominal cramps, diarrhea, Clostridium perfringens, 12 h putrefactive diarrhea associated Bacillus cereus, Streptoco ccus with C. perfringens , sometimes faecalis, S. faecium nausea and vomiting. 12-74 h, mean Abdominal cramps, diarrhea, Salmonella species (including 18-36 h vomiting, fever, chills, malaise, S. arizonae), Shigella, nausea, headache, possible. enteropathogenic Escherichia Sometimes bloody or mucoid coli, other Enterobacteriacae , diarrhea, cutaneous lesions Vibrio parahaemolyticus , associated with V. vulnificus. Yersinia enterocolitica , Yersinia enterocolitica mimics Aeromonas hydrophila, flu and acute appendicitis. Plesiomonas shigelloides , Campylobacter jejuni, Vibrio cholerae (O1 and non-O1) V.vulnificus , V. fluvialis 3-5 days Diarrhea, fever, vomiting Enteric viruses abdominal pain, respiratory symptoms. -

Postorgasmic Illness Syndrome: What Do We Know So Journal of Far? J Rare Dis Res Treat
Le TV, Nguyen HMT, Hellstrom WJG. Postorgasmic Illness Syndrome: What do we know so Journal of far? J Rare Dis Res Treat. (2018) 3(2): 29-33 Rare Diseases Research www.rarediseasesjournal.com & Treatment Mini Review Open Access Postorgasmic Illness Syndrome: What do we know so far? Tan Vu Le1, Hoang Minh Tue Nguyen1, Wayne J.G. Hellstrom1* 1Tulane University School of Medicine, Department of Urology, New Orleans LA, USA ABSTRACT Post-orgasmic illness syndrome (POIS) is rare condition that is characterized Article Info by transient flu-like symptoms and cognition disorders that occur shortly after ejaculation and last for 2-7 days. There are about 50 cases of POIS in Article Notes Received: June 05, 2018 the literature. The prevalence and incidence of POIS are still unknown due to Accepted: July 04, 2018 a paucity of studies. The exact pathogenesis of POIS remains unknown; the most acceptable hypothesis is an autoimmune/allergic process. We made *Correspondence: a literature search via PubMed for publications from 2002 to 2018 with the Dr. Wayne J.G. Hellstrom, Tulane University School of “post orgasmic illness syndrome” medical subject heading term to analyze Medicine, Department of Urology, 1430 Tulane Ave., 86-42, current data regarding symptoms, burden, pathophysiology, and to discuss New Orleans, LA 70112-2632, USA; Telephone No: (504) 988-3361; Fax No: (504) 988-5059; potential management options for POIS. POIS is diagnosed by five preliminary Email: [email protected] diagnostic criteria. It is categorized into two types: primary and secondary. There is the concomitance between POIS and PE. The autoimmune/allergy © 2018 Hellstrom WJG.