"When Someone Has Low Vision" Community Eye Health Journal Vol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Euraseans: Journal on Global Socio-Economic Dynamics, № 6 (7
“The EUrASEANs: journal on global socio-economic dynamics” Volume 6 (7); November - December, Year 2017; ISSN 2539 – 5645 (Print) Copyright © 2017, [The EUrASEANs] on-line access: https://www.euraseans.com/6(7) IMPACTS ON CONSUMER BEHAVIOR: THE CASE STUDY ON VIETNAM MULTI-LABEL FASHION STORE Irina V. Onyusheva Panirat Kaewpradit Stamford International University, Thailand, Bangkok The purpose of this paper is to study customer behavior which nearly always can be impacted by the environment around a particular store. There is a tremendous rising demand for fashion items in Vietnam. Recently, some Vietnam designer brands have become available at the market without own flagship store. A multi-label fashion store representing a variety of designer brand items enable the Vietnamese to select the needed appreciating the whole variety of fashionable quality outfits in one place. The multi-label fashion store is often difficult to manage in terms of planning and design, also, it is very different from a flagship store. Becoming aware of the environment surrounding a multi-label fashion store enable marketers to create new opportunities in terms of sales. This study has been carried out in the form of surveys so that to analyze the behavior in Vietnamese consumers purchasing fashion items. This has helped us understand how multilabel fashion retail stores are using the merchandising display and space layout so that to influence Vietnamese customers’ behavior, in both positive and negative ways. Therefore, marketers may consider our results as important information to be used further to improve the store environment in order to meet customer need better and thus – to enhance sales. -
Panelist Agenda
REGIONAL WINNERS CONFERENCE Thursday Dec 5th 2019, 0915 - 1545 hrs Venue Host: Baker Mckenzie Wong & Leow, Raffles Room at 8 Marina Boulevard #05-01 Marina Bay Financial Centre Tower 1, Singapore 018981 9.15 - 9.25 Registration 9.25 - 9.30 Welcome and Introduction by Patrick Schult (Host) 9.30 - 9.45 OPENING INSIGHTS by Ricky Ow, President WarnerMedia APAC & Chairperson of AAA 2019 9.45 - 10.30 INSIDERS GUIDE TO AWESOME KIDS TV moderated by Jamie Turner, WarnerMedia Panelists: Kiko S2 by Ella Kartika, MNC- Studio International TBK Ollie and Friends (S5) by Seng- Choon Meng, Infinite Studios Shimajiro: A World of WOW! - Life & Survival - Living Together, Living Creatively by Ai Aochi, Benesse Corp Japan Hiccup & Sneeze S2 / Kooki’s Crafty Show by Susan Oliver, Beach House Kids 10.30 - 11.00 HOW TO IMMERSE IN BEST OF IMMERSIVE moderated by Dennis Breckenridge, Elevate Broadcast Panelists: VR Experience for Santos de Cartier Launch by Arturo Casares, LR Studio 360 Perspective: Women of the Mountains by Voltaire Tupaz, FYT 11.00 - 11.15 INDUSTRY INSIGHTS: Top 5 tips for Producers on media insurance by Ronald Loke, Arthur J Gallagher 11.15 - 11.30 COFFEE 11.30 - 11.45 INDUSTRY INSIGHTS: “The Future of Content Distribution and Acquisition” by Ian Mckee, VUULR 11.45 - 12.15 ALL THE FANTASTIC FORMATS ONE IS LOOKING FOR GLOBALLY moderated by Natasha Malhotra, VUULR Panelists: Designated Survivor: 60 Days by Seryeong Jeong, CJ ENM The Bridge by Min Lim, Double Vision for Viu Descendants of the Sun (Vietnamese Remake) by Ngo Bich Hanh, Vietnam Media -

Tiên Hắc Ám 2 Maleficent:Mistress of Evil
AMAZING INFLIGHT ENTERTAINMENT 01-02 | 2020 Tiên Hắc Ám 2 Maleficent: Mistress of Evil Tổng thời lượng chương trình giải trí trên 600 giờ More than 600 hours of entertainment © 2020 Disney Chương trình nổi bật Mục lục Vietnam Airlines recommends Contents Hướng dẫn 03 Information Danh sách phim 04 điện ảnh Movie listings Danh sách phim 05 truyền hình TV listings Chương trình mới 08 New on-board Danh sách phim 24 truyền hình TV listings Sách nói 33 Audio book Trò chơi 33 Games Âm nhạc 34 Music 10 16 25 32 Chùm Phim Bom Tấn Tiên Hắc Ám 2 Will Smith Ngọt Blockbuster Boxsets Maleficent: Mistress of Evil © 2020 WBEI TM & © DC Comics © 2020 Disney © 2019 Paramount Pictures Với hình ảnh bông sen vàng chơi lôi cuốn, hấp dẫn. Tất cả LotuStar. The pages of the Ngôn ngữ Thể loại Hướng dẫn Chào mừng thân quen, LotuStar là thành các nội dung trên đều được booklet will guide you to the Language Genre Information quả của quá trình không sắp xếp, trình bày theo từng enjoyment of audio-visual Quý khách ngừng nỗ lực của Vietnam chuyên mục để thuận tiện entertainment that includes Tiếng Việt PG-13 - Parents strongly cautioned Chương trình giải trí của chúng tôi Airlines với mong muốn mang cho lựa chọn của Quý khách. classic movies, blockbusters, Vietnamese Hành động | Action trên chuyến Có một số cảnh không thích hợp với thay đổi tùy thuộc vào loại máy bay đến cho Quý khách những timeless and favourite Tiếng Anh và đường bay. -

A Branding Revolutionist
1I SUCCESSFUL BRANDING LESSONS: Jack Ma, Richard Branson & Usain Bolt YUSUF TAIYOOB : The King Of Dates MYDIN : Heartland Retail Empire SAY YES2BRAND : Aspiring for a Better Tomorrow, Today TAN SRI DATO’ SRI LEONG HOY KUM RM15 WM RM18 EM A BRANDING REVOLUTIONIST DECEMBERMAY-JANUARY’ - JUNE’ 1714 #ISSUE4119 II 1 All information herein is correct at time of publication. THE TEAM | The views and opinions expressed or implied in The BrandLaureate Business World Review ADVISOR are those of the authors and contributors and do not necessarily Dr KKJohan reflect those of The BrandLaureate, its editorial & staff. All editorial content and materials are copyright of PUBLISHER/EDITOR-IN-CHIEF THE BRANDLAUREATE BUSINESS WORLD REVIEW Chew Bee Peng No Permit KDN PQ/PP16972/08/2011)(028331) MANAGING EDITOR The BrandLaureate Business World Review is published by Ida Ibrahim THE BRANDLAUREATE SDN BHD (690453K), 39B & 41B, SS21/60, Damansara Utama, 47400 Petaling Jaya. Tel: (603) 7710 0348 Fax: (603) 7710 0350 SENIOR WRITER Ian Gregory Edward Masselamani Printed in Malaysia by PERCETAKAN SKYLINE SDN BHD (PQ 1780/2317) WRITERS 35 & 37, Jalan 12/32B, TSI Business Industrial Park, Batu 6 1/2, Nurilya Anis Rahim Off Jalan Kepong, 52000 Kuala Lumpur, Malaysia. Ain M.C. Gerald Chuah CONTRIBUTORS Anu Venugopal, Tony Thompson, Justin Chew, Sean Tan CREATIVE MANAGER Ibtisam Basri ASSISTANT CREATIVE MANAGER Mohd Shahril Hassan SENIOR GRAPHIC DESIGNER Mohd Zaidi Yusof MULTIMEDIA DESIGNER Zulhelmi Yarabi EDITORIAL ASSISTANTS Kalwant Kaur Lau Swee Ching For suggestions and comments or further enquiries on THE BRANDLAUREATE BUSINESS WORLD REVIEW, please contact [email protected]. “Position Your Brand on a World Class Platform” THE BRANDLAUREATE • BUSINESS WORLD REVIEW MAY - JUNE’ 17 #ISSUE41 2 3 PUBLISHER NOTE | What’s in a name, you may ask? Minister of Canada show that age does not really W Everything if I may say! matter. -

Đại Úy Marvel Captain Marvel
AMAZING INFLIGHT ENTERTAINMENT 07-08 | 2019 ĐẠI ÚY MARVEL CAPTAIN MARVEL Tổng thời lượng chương trình giải trí trên 600 giờ More than 600 hours of entertainment Plus de 600 heures de divertissement © 2019 MARVEL Chương trình nổi bật. Mục Lục Vietnam Airlines Recommends Contents / Sommaire Vietnam Airlines recommande 03 Hướng dẫn Information Informations 04 Danh sách phim điện ảnh Movie listings Liste des Films 05 Danh sách phim truyền hình TV listings Liste des programmes TV 08 Chương trình mới New on-board Nouveautés à bord 22 Phim truyền hình TV listings Liste des programmes TV 33 Sách nói Audio book Livres audio 33 Trò chơi Games Jeux vidéos 34 Âm nhạc Music Musique 14 21 Đại Úy Marvel Tim Burton Captain Marvel © 2019 MARVEL © 2019 Disney Enterprises, Inc. All Rights Reserved Với hình ảnh bông sen vàng chơi lôi cuốn, hấp dẫn. Tất cả LotuStar. The pages of the services. Les pages de cette Chào mừng thân quen, LotuStar là thành các nội dung trên đều được booklet will guide you to the brochure vous guideront quả của quá trình không sắp xếp, trình bày theo từng enjoyment of audio-visual au travers du système de Quý khách ngừng nỗ lực của Vietnam chuyên mục để thuận tiện entertainment that includes divertissement audiovisuel Airlines với mong muốn mang cho lựa chọn của Quý khách. classic movies, blockbusters, qui inclut de grands films trên chuyến đến cho Quý khách những timeless and favourite classiques, des blockbusters, bay của phút giây giải trí thư giãn trên Và bây giờ, xin mời Quý musical compositions, audio des compositions musicales chuyến bay. -

Advertising Price List
BẢNG GIÁ QUẢNG CÁO (Áp dụng từ ngày 1.7.2017) Thaânh phêím: 200 x 280 mm Àún võ tñnh: àöìng KÑCH THÛÚÁC TRANG VÕ TRÑ ÀÚN GIAÁ Bìa 4 45.000.000 Bìa 2 38.000.000 Bìa 3 28.000.000 Trang số 1 38.000.000 Trang số 3 45.000.000 Nguyên trang: 175x250 mm Nguyên trang (tràn lề): 203x286 mm Nguyên trang 29.000.000 Trang phải đầu tiên 30.000.000 BẢNG GIÁ QUẢNG CÁO/ ADVERTISING1/2 trang PRICEdọc LIST 21.000.000 (Áp dụng từ ngày 01/01/2020 - The price is appied from 01/01/2020) 1/2 trang ngang 16.000.000 Thành phẩm/Finished products: 215mm x 275mm 1/3 trang dọc Đơn vị tính/Unit:11.000.000 VNĐ Kích thước trang/Page size Vị1/4 trí/Location trang góc Đơn8.500.000 giá/Price 1/2 trang dọc: 85x250 mm 1/3 trang dọc: 55x250 mm 1/2 trang ngang: 175x123 mm 1/4 trang góc: 85x123 mm 1/8 trang 4.000.000 1/8 trang: 85x60 mm Bìa 4/Back cover 70,000,000 Chân trang: 175x30 mm BìaChân 2/Behind trang the main cover 60,000,0006.000.000 Trang đơn Bìa 3/Cover front of back cover 55,000,000 Full page Trang* Tự giới 3 (trang thiệu phải(nội dungđầu tiên)/The khách hàng 3rd pagecung cấp) 70,000,000 Nguyên trang phải/ Full right page 50,000,000 1 trang 29.000.000 Nguyên trang trái/Full left page 45,000,000 Nguyên trang/Full page: 215mm x 275mm Trang 1/2 trang đôi/ Double pages 80,000,00016.000.000 * Tự giới thiệu (Saigontimes thực hiện nội dung) Tự giới thiệu/Editorial/Advertorial 1 trang 31.000.000 Nội dung do khách hàng cung cấp (Advertorial) Tự giới thiệu 1 trang: 175x250 mm Logo trang mục lục: 55x30 mm 1/2 trang 20.000.000 Tự giới thiệu 1/2Trang trang:175x123 đơn mm Rao vặt: -

Tiên Hắc Ám 2 Maleficent: Mistress of Evil 말레피센트 2
AMAZING INFLIGHT ENTERTAINMENT 01-02 | 2020 Tiên Hắc Ám 2 Maleficent: Mistress of Evil 말레피센트 2 Tổng thời lượng chương trình giải trí trên 600 giờ More than 600 hours of entertainment 600시간 이상 제공되는 엔터테인먼트 © 2020 Disney Chương trình nổi bật Mục lục Vietnam Airlines recommends Contents / 목록 베트남 항공 추천 Hướng dẫn 03 Information 안내 Danh sách phim 04 điện ảnh Movie listings 영화 목록 Danh sách phim 05 truyền hình TV listings TV 목록 Chương trình mới 08 New on-board 신규 추가 목록 Danh sách phim 24 truyền hình TV listings TV 목록 Sách nói 33 Audio book 오디오 북 Trò chơi 33 Games 게임 Âm nhạc 34 Music 음악 10 16 25 32 Chùm Phim Bom Tấn Tiên Hắc Ám 2 Will Smith Ngọt Blockbuster Boxsets Maleficent: Mistress of Evil 블록버스터 박스 세트 말레피센트 2 © 2020 WBEI TM & © DC Comics © 2020 Disney © 2019 Paramount Pictures Với hình ảnh bông sen vàng chơi lôi cuốn, hấp dẫn. Tất cả LotuStar. The pages of the 책자에는 고전 영화, 블록버스터, Chương trình giải trí của chúng tôi Chào mừng thân quen, LotuStar là thành các nội dung trên đều được booklet will guide you to the 세월이 흘러도 변함없이 Ngôn ngữ Thể loại Hướng dẫn 사랑받는 음악, 언어 안내 thay đổi tùy thuộc vào loại máy bay quả của quá trình không sắp xếp, trình bày theo từng enjoyment of audio-visual Language / Genre / 장르 Information / và đường bay. Vì vậy, một số chương 오디오북 및 흥미로운 게임 Quý khách ngừng nỗ lực của Vietnam chuyên mục để thuận tiện entertainment that includes trình có thể không có trên chuyến 등이 수록된 시청각 오락물이 Tiếng Việt Airlines với mong muốn mang cho lựa chọn của Quý khách. -

Tim Minh Trong the Gioi Hau Tuoi Tho (Sua Taiban)
1. “TÔI MUỐN MỌI NGƯỜI BIẾT RẰNG CÓ NHIỀU ĐỨA TRẺ VẪN ĐANG CHỐNG CHỌI TỪNG NGÀY ĐỂ LỚN LÊN THÀNH NGƯỜI TỬ TẾ” (Phương Anh, 20 tuổi, bỏ đại học)(1) Bạn đã xem Gordon Ramsay chửi như điên trong bếp, đúng không? Fuck! Fuck! Fuck! Fuck! Gordon Ramsay trong Master Chef ấy. Tôi cũng nóng tính như vậy. Hôm trước tôi rẽ qua tiệm bánh, nơi tôi làm bán thời gian kể từ khi bỏ Đại học Thương Mại để học làm bánh và quản lý nhà hàng. Tôi sẽ không kể là bố mẹ tôi phản ứng như thế nào, nhưng khi cấp Hai bạn học trường điểm và cấp Ba chuyên Chu Văn An thì bạn có thể đoán là chuyện bạn đi học nghề nó kinh khủng với bố mẹ như thế nào. Đến giờ tôi vẫn phải nói dối bạn bè của bố mẹ để giữ sĩ diện cho họ. 1. Nhân vật dùng danh tính thật. Ngoài những chỗ có chú thích thì danh tính của nhân vật đã được thay đổi để bảo vệ sự riêng tư. 12 ĐẶNG HOÀNG GIANG Chỗ tiệm bánh tôi đang làm cũng có tới bảy, tám đứa bỏ đại học hoặc bảo lưu. Tôi hơi giật mình, “Có nhiều đứa giống mình vậy à?” Chưa bao giờ tôi hối hận. Từ khi học nghề tôi biết trân trọng lao động hơn. Tôi không ngại việc. Tôi chấp nhận một mức lương bèo bọt hay một công việc nặng nhọc nếu như tôi được học hỏi. Và tôi không phàn nàn khi phải đợi đồ uống lâu ở nhà hàng nữa, tôi biết là họ đang rất bận, họ đang rất cố gắng. -
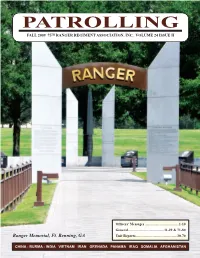
Patrolling Fall 2009 75 TH Ranger REGIMENT Association, INC
PaTROllING Fall 2009 75 TH RaNGER REGIMENT aSSOCIaTION, INC. VOlUME 24 ISSUE II Officers’ Messages ......................................1-10 General ........................................11-29 & 71-80 Ranger Memorial, Ft. Benning, GA Unit Reports ..............................................30-70 CHINA - BURMA - INDIA VIETNAM IRAN GRENADA PANAMA IRAQ SOMALIA AFGHANISTAN PATROLLING – FALL 2009 Don & Vergie Bizadi at the banquet, Saturday, August 8, 2009. Behind them is a larger replica of the Navajo rug they presented to the Association at the banquet. PATROLLING – FALL 2009 WHO WE ARE: The 75th Ranger Regiment Association, Inc., is a We have funded trips for families to visit their wounded sons and registered 501 (c) corporation, registered in the State of Georgia. We were husbands while they were in the hospital. We have purchased a learning founded in 1986 by a group of veterans of F/58, (LRP) and L/75 (Ranger). program soft ware for the son of one young Ranger who had a brain The first meeting was held on June 7, 1986, at Ft. Campbell, KY. tumor removed. The Army took care of the surgery, but no means existed OUR MISSION: to purchase the learning program. We fund the purchase of several awards 1. To identify and offer membership to all eligible 75th Infantry Rangers, for graduates of RIP and Ranger School. We have contributed to each of and members of the Long Range Reconnaissance Patrol the three Battalion’s Memorial Funds and Ranger Balls, Companies, Long Range Patrol Companies, Ranger and to the Airborne Memorial at Ft. Benning. Companies and Detachments, Vietnamese Ranger We have bi-annual reunions and business meetings. -

Accept, Adopt & Accelerate Changing Role Of
+ 5 October-December 2020+ + www.apb-news.com OCTOBER-DECEMBER 2020 NEWS & VIEWS 6 CREATION 14 MANAGEMENT 17 +TELECOM & ICT 21 DISTRIBUTION 25 Accept, adopt & accelerate changing role of technology ... or die! The Covid-19 pandemic in 2020 has cast a pall on ❝IABM, early in the pandemic, the broadcast industry, halting production, disrupting took radical action and created workflows and forcing the cancellation of live events a Virtual Platform … hugely and trade shows such as NAB Show and IBC Showcase. successful in helping members How can we recover, what changes will define to communicate and the next 12 months and how should broadcasters put them in front of navigate themselves in 2021? APB+ Managing Editor technology buyers.❞ Raymond Tan speaks to Peter White, Chairman of — Peter White, Chairman, IABM the International Trade Association for the Broadcast & Media Industry (IABM), on his thoughts of what lies consolidation as well as increased investment in content. ahead … The move to DTC with its thin- ner margins also requires increased APB+: What is the state of the mar- a new generation of IT and environ- efficiency and agility, producing a ket now and how has the pandemic ment-aware talent. greater focus on business models. – from lockdown restrictions to The pandemic and ensuing lock- Technology has become merely an the cancellation of trade events – downs have driven digital subscrip- enabler for those business models, impacted the broadcast and media tions massively upwards, while tradi- and broadcasters are increasingly industry, derailing growth and tional pay-TV and advertising-based turning to insourcing for better innovation in 2020? business models have been hit hard control and responsiveness. -

"Low Vision: We Can All Do More" Community Eye Health Journal Vol
Community Eye Health JOURNALVOLUME 25 | ISSUE 77 Low vision: we can all do more Hasan Minto Regional Director for the Eastern Mediterranean, International Centre for Eyecare Education. Karin van Dijk Clare Gilbert Co-director, International Centre for Eye Health, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT, UK; Clinical Advisor, Sightsavers. Despite all the treatments, operations, and medication at our disposal, there is still a significant number of people whose sight we cannot fully restore. What happens to these patients once they leave our care? Without the neces- sary support, advice, and low vision devices, their remaining vision will not be very good; this can make life a struggle. Support may be difficult to find, as low vision services are often inadequate or Use real tasks to inaccessible in many low- and middle- assess near vision. income countries. Professionals, such as TANZANIA rehabilitation workers, ophthalmologists, mid-level eye care workers, optometrists/ and/or optical) have been given. The people’s lives. People with low vision may refractionists, and special education definition also emphasises the importance struggle to look after themselves without teachers, may not know what to do about of vision for day-to-day functioning. help. Having low vision affects their people with low vision, leaving them with People who may be able to benefit from status in the eyes of others and can make no-one else to turn to. low vision care will want to do a range of social situations difficult. It reduces the Individuals who can only see light or different things. -

Low Vision: We Can All Do More Hasan Minto Regional Director for the Eastern Mediterranean, International Centre For
internationalArticles edition from C ommunity Eye Health CEHJ 77&78 JOURNAVOLUMEL 2 | ISSUE 4 | DecembeR 2012 INDIAN EDITION Low vision: we can all do more Hasan Minto Regional Director for the Eastern Mediterranean, International Centre for Eyecare Education. Dole Kuldeep Clare Gilbert Co-director, International Centre for Eye Health, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT, UK; Clinical Advisor, Sightsavers. Despite all the treatments, operations, and medication at our disposal, there is still a significant number of people whose sight we cannot fully restore. What happens to these patients once they leave our care? Without the neces- sary support, advice, and low vision devices, their remaining vision will not be very good; this can make life a struggle. Low vision assessment. Support may be difficult to find, as low INDIA vision services are often inadequate or inaccessible in many low- and middle- vision interventions once all other treat- Low vision has a significant impact on income countries. Professionals, such as ments the person needs (surgical, medical people’s lives. People with low vision may rehabilitation workers, ophthalmologists, and/or optical) have been given. The struggle to look after themselves without mid-level eye care workers, optometrists/ definition also emphasises the importance help. Having low vision affects their refractionists, and special education of vision for day-to-day functioning. status in the eyes of others and can make teachers, may not know what to do about People who may be able to benefit from social situations difficult. It reduces the people with low vision, leaving them with low vision care will want to do a range of ability of people to pursue an education, to no-one else to turn to.