Require Initiation of Oral/IV Corticosteroids - Require a Corticosteroid Injection
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
NOTE: the Following Are Shirley Ryan Abilitylab's Standard Charges As of Jan. 1, 2019. These Standard Charges Often Do Not
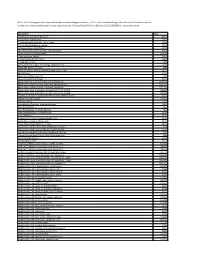
NOTE: The following are Shirley Ryan AbilityLab's standard charges as of Jan. 1, 2019. These standard charges often do not reflect what a patient or their insurance company/payer may be required to pay. Contact Patient Financial Services at 312-238-6039 for more information. Description Price 11-Deoxycortisol, Urine Random $531 12 Lead Ekg, Tracing Only $245 17 Hydroxycorticosteroids, Urine Timed $363 17 Hydroxyprogesterone, Serum $172 17 Ketosteroids, Urine Timed $273 17-Ketosteroids with Creatinine, Urine Random $273 2D Gait Analysis Charge(95999) $2,174 5' Nucleotidase, Serum $269 5.5 PDC PEDS CUFFED TRACH $226 5-HIAA-24 Hr Urine $99 A4566 Shoulder sling or vest design, abduction res $226 A4595 FES Electrode, each $38 A6545 Gradient Compression Wrap, Non-Elastic, Belo $171 ABO Rh Type $106 Above Knee Nylon Hose PR $83 Above Knee Suction Sheath $131 Above knee, for proximal femoral focal deficiency, $14,344 Above knee, molded socket, open end, SACH foot, en $10,751 Above knee, molded socket, single axis constant fr $10,935 Above knee, short prosthesis, no knee joint (""stu_L5210 $8,682 Above knee, short prosthesis, no knee joint (""stu_L5220 $7,429 ACAPELLA DH GREEN VIBRATORY PEP W/MOUTHPIECE DEVIC $181 Acetabuloplasty (27120) $4,493 Acetone, Serum $27 Acetylcholine Receptor Binding Antibody $405 Acid Phosphatase $66 Acid Phosphatase, Prostatic fraction $66 ACNE SURGERY MILIA CYSTS (10040) $530 Acorn Nebulizer $174 Activated PTT/Partial Thromboplastin Time $109 Active Wound Care > 20 cm Units $171 Active Wound Care/20 cm or < Units $171 Acupuncture with E-Stim. Each additional 15 minute $65 Acupuncture with E-Stim. -

Dexamethasone Sodium Phosphate Injection, USP)
HEXADROL® PHOSPHATE INJECTION (dexamethasone sodium phosphate injection, USP) DESCRIPTION — Hexadrol® Phosphate Injection (dexamethasone sodium phosphate injection, USP) is a water-soluble inorganic ester of dexamethasone which produces a rapid response even when injected intramuscularly. Dexamethasone Sodium Phosphate, C22H28FNa2O8P, has a molecular weight of 516.41 and chemically is Pregn-4-ene-3, 20-dione, 9-fluoro-11, 17-dihydroxy-16-methyl-21 (phosphonooxy)-, disodium salt, (11β, 16α). It occurs as a white to creamy white powder, is exceedingly hygroscopic, is soluble in water and its solutions have a pH between 7.5 and 10.5. It has the following structural formula: Hexadrol® Phosphate Injection is available in 4 mg/mL and 10 mg/mL concentrations. Each mL of Hexadrol® Phosphate Injection 4 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 4 mg dexamethasone phosphate; 1 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. 1 Reference ID: 3593917 Each mL of Hexadrol® Phosphate Injection 10 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 10 mg dexamethasone phosphate; 1.5 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. ACTIONS — Naturally occurring glucocorticoids (hydrocortisone), which also have salt- retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their potent anti-inflammatory effects in disorders of many organ systems. Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body’s immune responses to diverse stimuli. -

Vertebroplasty (Repair of Vertebrae with Bone Cement)
Patient information – Radiology Unit Tel 0118 322 7991 Vertebroplasty (repair of vertebrae with bone cement) Introduction This leaflet tells you about the procedure known as “vertebroplasty”, explains what is involved, the benefits and possible risks. It is not meant to replace informed discussion between you and your doctor but can act as a starting point for such a discussion. You should have plenty of time to discuss this procedure with the doctor who will be performing the procedure. What is vertebroplasty? Vertebroplasty is a procedure used to strengthen a collapsed spinal vertebra that has fractured and usually lost height due to osteoporosis or, less commonly, tumour infiltration or trauma. Vertebroplasty is primarily aimed at relieving the patient’s pain, to allow a rapid return to the previous level of activity, and secondarily to prevent further vertebral collapse. It is minimally invasive which means that patients suffer less disruption, face less risk and recover more quickly than with conventional open surgery. It is most effective when the fracture is relatively recent and particularly in patients who are very debilitated by the pain of the fracture or who cannot tolerate adequate quantities of painkilling medication. In some circumstances, vertebroplasty can be very effective even if the fracture is many months or even years old. Vertebroplasty is accomplished by injecting orthopaedic cement through a needle into the fractured bone; essentially forming an internal cast to stabilise the fracture similar to the principle of using plaster cast on an arm fracture. Typically, vertebroplasty is recommended if simpler treatments, such as bed rest, back bracing or pain medication have been ineffective, or if the side effects of analgesia have become problematic, such as causing stomach ulcers or drowsiness. -

Oxford® Policy Update Bulletin: December 2015 Oxford
Oxford December 2015 policy update bulletin Medical & Administrative Policy Updates UnitedHealthcare respects the expertise of the physicians, health care professionals, and their staff who participate in our network. Our goal is to support you and your patients in making the most informed decisions regarding the choice of quality and cost-effective care, and to support practice staff with a simple and predictable administrative experience. The Policy Update Bulletin was developed to share important information regarding Oxford® Medical and Administrative Policy updates.* *Where information in this bulletin conflicts with applicable state and/or federal law, Oxford® follows such applicable federal and/or state law Oxford Oxford® Medical and Administrative Policy Updates Overview This bulletin provides complete details on Oxford® Medical and Policy Update Classifications Administrative Policy updates. The appearance of a service or New procedure in this bulletin indicates only that Oxford® has recently New clinical coverage criteria and/or documentation review requirements adopted a new policy and/or updated, revised, replaced or have been adopted for a service, procedure, test, or device retired an existing policy; it does not imply that Oxford® provides Updated coverage for the service or procedure. In the event of an An existing policy has been reviewed and changes have not been made inconsistency or conflict between the information provided in this to the clinical coverage criteria or documentation review requirements; bulletin and the posted policy, the provisions of the posted policy however, items such as the clinical evidence, FDA information, and/or will prevail. Note that most benefit plan documents exclude from list(s) of applicable codes may have been updated benefit coverage health services identified as investigational or unproven/not medically necessary. -

Prescription Drugs Requiring Prior Authorization
PRESCRIPTION DRUGS REQUIRING PRIOR AUTHORIZATION Revised 10/16 As part of our drug utilization management program, members must request and receive prior authorization for certain prescription drugs in order to use their prescription drug benefits. Below is a list of drugs that currently require prior authorization. This list will be updated periodically as new drugs that require prior authorization are introduced. As benefits may vary by group and individual plans, the inclusion of a medication on this list does not imply prescription drug coverage. The Schedule of Benefits contains a list of drug categories that require prior authorization. Prior authorization requests are processed by our pharmacy benefit manager, Express Scripts, Inc. (ESI). Physicians must call ESI to obtain an authorization. (1-800-842-2015). Drug Name Generic Name Drug Classification Abstral fentanyl citrate oral tablet Controlled Dangerous Substance Accu-Chek Test Strips blood glucose test strips Blood Glucose Test Strips Actemra tocilizumab Monoclonal Antibody Acthar corticotropin Hormone Actimmune interferon gamma 1b Interferon Actiq fentanyl citrate OTFC Controlled Dangerous Substance Adcirca tadalafil Pulmonary Vasodilator Adempas riociguat Pulmonary Vasodilator Adlyxin lixisenatide Type 2 Diabetes Advocate Test Strips blood glucose test strips Blood Glucose Test Strips Aerospan** flunisolide Corticosteroids (Inhaled) Afrezza insulin Insulin (inhaled) Ampyra dalfampridine Multiple Sclerosis Agent Altoprev** lovastatin Cholesterol Alvesco** ciclesonide Corticosteroids -

Joint Injection As an Out-Patient Procedure
This leaflet is available in large print, Braille and on tape. Please contact Geoff Pennock on 0151 604 7289. Joint Injection As An Out-Patient Procedure Wirral University Teaching Hospital NHS Foundation Trust operates a No Smoking Policy. Please refrain from smoking on site. Information for Patients Orthopaedic Clinic Author: K Howard Date of Publication: June 2013 Date for Review: June 2015 Reference: Taken from the BUPA information leaflet. Having an injection into the joint. PL/00293/Surgical-Ortho/0613 Do Not Copy. For further copies contact Supplies quoting the PL number. This leaflet provides some information The risks of a joint injection In order to get maximum benefit from about joint injections. Please take Joint injections are a commonly your injection;- this home for further referral. Your performed and are generally safe consultant has prescribed this treatment procedures. Adverse reactions and • Rest the joint for a day. You may to meet your individual needs. Please side effects are rare; some patients need to take time off work, this will raise any concerns or questions you experience quite a painful reaction depend on the type of job you do – have and we will endeavour to answer after the injection lasting two-four your consultant will advise. them. days, this will normally settle. However, • You may need to take occasional if you do experience excessive pain, pain relieving medication e.g. The benefits of a joint injection swelling or you become unwell with Paracetamol, or anti- inflammatory The purpose of administering a a temperature, contact your doctor or tablets. joint injection is to reduce pain, the clinic immediately. -

CLINICAL GUIDELINES CMM-200: Epidural Steroid Injections (ESI) Version 1.0 Effective February 14, 2020
CLINICAL GUIDELINES CMM-200: Epidural Steroid Injections (ESI) Version 1.0 Effective February 14, 2020 Clinical guidelines for medical necessity review of Comprehensive Musculoskeletal Management Services. © 2019 eviCore healthcare. All rights reserved. Comprehensive Musculoskeletal Management Guidelines V1.0 CMM-200: Epidural Steroid Injections(ESI) CMM-200.1: Definitions 3 CMM-200.2: General Guidelines 4 CMM-200.3: Indications: Selective Nerve Root Block (SNRB) 5 CMM-200.4: Indications: Epidural Steroid Injections (Transforaminal, Interlaminar, or Caudal) 5 CMM-200.5: Non-Indications: SNRB 6 CMM-200.6: Non-Indications: ESI 7 CMM-200.7: Procedure (CPT®) Codes 8 CMM-200.8: References 10 ______________________________________________________________________________________________________ ©2020 eviCore healthcare. All Rights Reserved. Page 2 of 16 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Comprehensive Musculoskeletal Management Guidelines V1.0 CMM -200.1: Definitions Transforaminal epidural steroid injection (TFESI) is a therapeutic injection of contrast (absent allergy to contrast) performed at a single or multiple spinal levels, followed by the introduction of a corticosteroid and possibly a local anesthetic by inserting a needle into the neuroforamen under fluoroscopic or computed tomography (CT) guidance. Selective Nerve Root Block (SNRB) is a diagnostic injection of contrast (absent allergy to contrast) of a single nerve root to assist with surgical planning, followed by the introduction of a local anesthetic by inserting a needle into the neuroforamen under fluoroscopic or computed tomography (CT) guidance. SNRBs are erroneously referred to as transforaminal epidural steroid injection (TFESI), although technically SNRBs involve the introduction of anesthetic only and are used for diagnostic purposes. Selective nerve root blocks (SNRBs) performed for the purpose of treating pain (i.e., repeat SNRB at the same level) may be termed therapeutic selective nerve root blocks. -
Sacroiliac Joint Injection
Dr Sean White Consultant in Pain Medicine Sacroiliac joint Injection 1 Introduction Before you agree to have your sacroiliac injections, it is sensible to know all you can about it. This means knowing why you may need sacroiliac injections, what the procedure is, and what it will be like, if there are any risks, and if there are any alternatives. Even if you are not keen on the details, getting an overall picture is helpful. This leaflet is a good starting point. It does not cover everything, so do mention any particular worries you may have. Ask for more information at any time. Patients, their pain problem and treatments all vary to a degree. But the leaflet should help you make the best decision. You will need to sign a consent form. This will happen just before the procedure at the hospital. This consent form records what you have agreed to. It is flexible enough to cover the unexpected. Please make sure everything is quite clear to you. Mention anything you do not wish to have done. You can change your mind even after signing the consent form. What are sacroiliac joint injections? Sacroiliac joints are the large pair of joints that hold the pelvis onto the spinal column. They help keep the spine straight and firm to hold your body weight. At the same time they allow limited movement so that you can bend, stretch and rotate. With injury or simple ‘wear and tear’ these joints can become painful. Injections into these joints are used to treat pain in that area. -

Clinical Guidelines
CLINICAL GUIDELINES Interventional Pain Management Services Version 1.0.2019 Clinical guidelines for medical necessity review of comprehensive musculoskeletal management services. © 2019 eviCore healthcare. All rights reserved. Regence: Comprehensive Musculoskeletal Management Guidelines V1.0.2019 Interventional Pain Management CMM-200: Epidural Steroid Injections (ESI) 3 CMM-201: Facet Joint Injections/Medial Branch Blocks 17 CMM-202: Trigger Point Injections 21 CMM-203: Sacroiliac Joint Injections 32 CMM-204: Prolotherapy 37 CMM-207: Epidural Adhesiolysis 40 CMM-208: Radiofrequency Joint Ablations/Denervations 44 CMM-209: Regional Sympathetic Blocks 51 CMM 210: Implantable Intrathecal Drug Delivery Systems 57 CMM-211: Spinal Cord Stimulators 65 CMM-308: Thermal Intradiscal Procedures 66 CMM-310: Manipulation of the Spine Under Anesthesia 71 ______________________________________________________________________________________________________ © 2019 eviCore healthcare. All Rights Reserved. Page 2 of 73 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Regence: Comprehensive Musculoskeletal Management Guidelines V1.0.2019 CMM-200: Epidural Steroid Injections (ESI) CMM-200.1: Definitions 4 CMM-200.2: General Guidelines 5 CMM-200.3: Indications: Selective Nerve Root Block (SNRB) 6 CMM-200.4: Indications: Epidural Steroid Injections 7 CMM-200.5: Non-Indications: SNRB 8 CMM-200.6: Non-Indications: ESI 8 ® CMM-200.7: Procedure (CPT ) Codes 9 CMM-200.8: References 10 ______________________________________________________________________________________________________ -

How to Boost Your Bottom Line with an Office Procedure -- Family
HOW TO Boost Your Bottom Line WITH AN OFFICE PROCEDURE Adding joint and soft-tissue injection to your practice can pay off in more ways than one. William D. Martz, MD Dr. Martz is medical director s practices’ expenses of the family practice office continue to grow at the University of Arizona at a faster pace Health Sciences Center. He has facilitated lectures and than revenues, workshops on joint injection Aphysicians are under greater technique. Conflicts of interest: pressure to do more with none reported. less. While working harder and seeing increasing num- bers of patients each day is an option, finding methods to work smarter is becoming an attractive alternative. One viable strategy for your practice is to increase charges per unit of time. Performing more proce- dures is a simple and suc- cessful way to achieve this goal. category of procedures well worth your time As you are probably aware, not all pro- and effort – joint and soft-tissue injections. cedures are created equal. Some procedures Here are some of the benefits of adding (e.g., flexible sigmoidoscopy) are reimbursed joint and soft-tissue injections to your clini- very poorly considering the time they cal armamentarium: require. Other procedures (e.g., skin biopsy • Patients appreciate their primary care and excisions, colposcopy/biopsy and exer- physicians offering services that traditionally cise treadmill testing), though reimbursed require a referral to a specialist. more handsomely, may require significant • Patients avoid treatment delays. amounts of physician and nursing time, • Physicians’ satisfaction improves when significant up-front costs to the practice and a variety of procedures are integrated into extensive training. -

Intra-Articular Injections in Knee Osteoarthritis: a Review of Literature
Journal of Functional Morphology and Kinesiology Review Intra-Articular Injections in Knee Osteoarthritis: A Review of Literature Gianluca Testa , Serena Maria Chiara Giardina, Annalisa Culmone, Andrea Vescio , Matteo Turchetta, Salvatore Cannavò and Vito Pavone * Department of General Surgery and Medical Surgical Specialties, Section of Orthopaedics and Traumatology, P.O. “Policlinico Gaspare Rodolico”, University of Catania, 95123 Catania, Italy; [email protected] (G.T.); [email protected] (S.M.C.G.); [email protected] (A.C.); [email protected] (A.V.); [email protected] (M.T.); [email protected] (S.C.) * Correspondence: [email protected]; Tel.: +39-095-378-2273 Abstract: Knee osteoarthritis (OA) is a chronic, degenerative, and progressive disease of articular cartilage, producing discomfort and physical disability in older adults. Thirteen percent of elderly people complain of knee OA. Management options for knee OA could be divided into the following categories: conservative, pharmacological, procedural, and surgical. Joint replacement is the gold standard, reserved for severe grades of knee OA, due to its complications rate and increased risk of joint revision. A nonsurgical approach is the first choice in the adult population with cartilage damage and knee OA. Yearly, more than 10% of knee OA-affected patients undergo intra-articular injections of different drugs, especially within three months after OA diagnosis. Several molecules, such as corticosteroids injection, hyaluronic acid (HA), and platelet-rich plasma (PRP), are managed to reduce the symptoms of patients with knee OA. The aim of this review was to offer an overview of intra-articular injections used for the treatment of OA and report the conventional pharmacological Citation: Testa, G.; Giardina, S.M.C.; products used. -
Course Description: Focuses on Integrating Subjective and Objective Findings of the Head, Thorax and Musculoskeletal Exam Into an Assessment and Plan of Care
PAS 6100: Physical Exam and Clinical Diagnosis I Fall 20XX COURSE INFORMATION Course Description: Focuses on integrating subjective and objective findings of the head, thorax and musculoskeletal exam into an assessment and plan of care. Includes techniques for oral and written presentations, relevant procedures, and assessment of specialty populations. Credits: 3 Prerequisites: Enrollment in the Physician Assistant Master’s Program Day and Time: Location: INSTRUCTOR INFORMATION Instructor: Office: Phone: Fax: Email: Office Hours: REQUIRED MATERIALS Required Textbooks: all available on Access Medicine: http://accessmedicine.mhmedical.com/. Text #1: LeBlond, R., Brown, D., DeGowin, R. DeGowin's Diagnostic Examination. 9th ed. New York, NY: McGraw-Hill; 2009. ISBN 978-0-07-160574-8 Text #2: Fortin VI, A., Dwamena, F., Frankel, R., Smith, R. Smith's Patient-Centered Interviewing: An Evidence-Based Method. 3rd ed. New York, NY: McGraw-Hill; 2012. ISBN 978-0-07-176000-3 Text #3: Stern, S., Cifu, A., Altkorn, D. Symptom to Diagnosis: An Evidence-Based Guide. 2nd ed. New York, NY: McGraw-Hill; 2010. ISBN 978-0-07-149613-1 Text #4: Nicoll, D., Lu, C., Pignone, M., McPhee, S. Pocket Guide to Diagnostic Tests. 6th ed. New York, NY: McGraw-Hill; 2012. ISBN 978-0-07-176625-8 Text #5: Henderson, M., Tierney Jr., M., Smetana, G. The Patient History: An Evidence-Based Approach to Differential Diagnosis. 2nd ed. China, McGraw-Hill; 2012. ISBN 978-0-07-162494- 7 Required Resources: Papadakis, M. Quick Medical Diagnosis & Treatment. AccessMedicine. (2014) Available at: http://accessmedicine.mhmedical.com/. Accessed September 18, 2014. COURSE OUTCOMES At the end of this course, students will be able to: 1.