Intralesional Corticosteroid Injection As an Effective Treatment Method for Oral Lesions: a Meta-Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Lumps and Swellings
Clinical Oral medicine for the general practitioner: lumps and swellings Crispian Scully 1 his series of five papers summarises some of the most important oral medicine problems likely to be Tencountered by practitioners. Some are common, others rare. The practitioner cannot be expected to diagnose all, but has been trained to recognise oral health and disease, and should be competent to recognise normal variants, and common orofacial disorders. In any case of doubt, the practitioner is advised to seek a second opinion from a colleague. The series is not intended to be comprehensive in coverage either of the conditions encountered, or all aspects of Figure 1: Torus mandibularis. diagnosis or treatment: further details are available in standard texts, in the further reading section, or from the internet. The present article discusses aspects of lumps through fear, perhaps after hearing of someone with and swellings. ‘mouth cancer’. Thus some individuals discover and worry about normal anatomical features such as tori, the parotid Lumps and swellings papilla, foliate papillae on the tongue, or the pterygoid Lumps and swellings in the mouth are common, but of hamulus. The tongue often detects even a very small diverse aetiologies (Table 1), and some represent swelling, or the patient may first notice it because it is sore malignant neoplasms. Therefore, this article will discuss (Figure 1). In contrast, many oral cancers are diagnosed far lumps and swellings in general terms, but later focus on too late, often after being present several months, usually the particular problems of oral cancer and of orofacial because the patient ignores the swelling. -
NOTE: the Following Are Shirley Ryan Abilitylab's Standard Charges As of Jan. 1, 2019. These Standard Charges Often Do Not
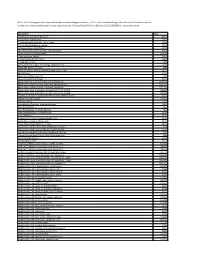
NOTE: The following are Shirley Ryan AbilityLab's standard charges as of Jan. 1, 2019. These standard charges often do not reflect what a patient or their insurance company/payer may be required to pay. Contact Patient Financial Services at 312-238-6039 for more information. Description Price 11-Deoxycortisol, Urine Random $531 12 Lead Ekg, Tracing Only $245 17 Hydroxycorticosteroids, Urine Timed $363 17 Hydroxyprogesterone, Serum $172 17 Ketosteroids, Urine Timed $273 17-Ketosteroids with Creatinine, Urine Random $273 2D Gait Analysis Charge(95999) $2,174 5' Nucleotidase, Serum $269 5.5 PDC PEDS CUFFED TRACH $226 5-HIAA-24 Hr Urine $99 A4566 Shoulder sling or vest design, abduction res $226 A4595 FES Electrode, each $38 A6545 Gradient Compression Wrap, Non-Elastic, Belo $171 ABO Rh Type $106 Above Knee Nylon Hose PR $83 Above Knee Suction Sheath $131 Above knee, for proximal femoral focal deficiency, $14,344 Above knee, molded socket, open end, SACH foot, en $10,751 Above knee, molded socket, single axis constant fr $10,935 Above knee, short prosthesis, no knee joint (""stu_L5210 $8,682 Above knee, short prosthesis, no knee joint (""stu_L5220 $7,429 ACAPELLA DH GREEN VIBRATORY PEP W/MOUTHPIECE DEVIC $181 Acetabuloplasty (27120) $4,493 Acetone, Serum $27 Acetylcholine Receptor Binding Antibody $405 Acid Phosphatase $66 Acid Phosphatase, Prostatic fraction $66 ACNE SURGERY MILIA CYSTS (10040) $530 Acorn Nebulizer $174 Activated PTT/Partial Thromboplastin Time $109 Active Wound Care > 20 cm Units $171 Active Wound Care/20 cm or < Units $171 Acupuncture with E-Stim. Each additional 15 minute $65 Acupuncture with E-Stim. -

Dexamethasone Sodium Phosphate Injection, USP)
HEXADROL® PHOSPHATE INJECTION (dexamethasone sodium phosphate injection, USP) DESCRIPTION — Hexadrol® Phosphate Injection (dexamethasone sodium phosphate injection, USP) is a water-soluble inorganic ester of dexamethasone which produces a rapid response even when injected intramuscularly. Dexamethasone Sodium Phosphate, C22H28FNa2O8P, has a molecular weight of 516.41 and chemically is Pregn-4-ene-3, 20-dione, 9-fluoro-11, 17-dihydroxy-16-methyl-21 (phosphonooxy)-, disodium salt, (11β, 16α). It occurs as a white to creamy white powder, is exceedingly hygroscopic, is soluble in water and its solutions have a pH between 7.5 and 10.5. It has the following structural formula: Hexadrol® Phosphate Injection is available in 4 mg/mL and 10 mg/mL concentrations. Each mL of Hexadrol® Phosphate Injection 4 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 4 mg dexamethasone phosphate; 1 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. 1 Reference ID: 3593917 Each mL of Hexadrol® Phosphate Injection 10 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 10 mg dexamethasone phosphate; 1.5 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. ACTIONS — Naturally occurring glucocorticoids (hydrocortisone), which also have salt- retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their potent anti-inflammatory effects in disorders of many organ systems. Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body’s immune responses to diverse stimuli. -

Vertebroplasty (Repair of Vertebrae with Bone Cement)
Patient information – Radiology Unit Tel 0118 322 7991 Vertebroplasty (repair of vertebrae with bone cement) Introduction This leaflet tells you about the procedure known as “vertebroplasty”, explains what is involved, the benefits and possible risks. It is not meant to replace informed discussion between you and your doctor but can act as a starting point for such a discussion. You should have plenty of time to discuss this procedure with the doctor who will be performing the procedure. What is vertebroplasty? Vertebroplasty is a procedure used to strengthen a collapsed spinal vertebra that has fractured and usually lost height due to osteoporosis or, less commonly, tumour infiltration or trauma. Vertebroplasty is primarily aimed at relieving the patient’s pain, to allow a rapid return to the previous level of activity, and secondarily to prevent further vertebral collapse. It is minimally invasive which means that patients suffer less disruption, face less risk and recover more quickly than with conventional open surgery. It is most effective when the fracture is relatively recent and particularly in patients who are very debilitated by the pain of the fracture or who cannot tolerate adequate quantities of painkilling medication. In some circumstances, vertebroplasty can be very effective even if the fracture is many months or even years old. Vertebroplasty is accomplished by injecting orthopaedic cement through a needle into the fractured bone; essentially forming an internal cast to stabilise the fracture similar to the principle of using plaster cast on an arm fracture. Typically, vertebroplasty is recommended if simpler treatments, such as bed rest, back bracing or pain medication have been ineffective, or if the side effects of analgesia have become problematic, such as causing stomach ulcers or drowsiness. -

ROLE of MAST CELL in ORAL PATHOLOGY Supriya Kheur Deepali Patekar Neeta Bagul Meena Kulkarni Samapika Routray 1 Varsha Dhas Department of Oral Pathology,Dr
320 ROLE OF MAST CELL IN ORAL PATHOLOGY Supriya Kheur Deepali Patekar Neeta Bagul Meena Kulkarni Samapika Routray 1 Varsha Dhas Department of Oral Pathology,Dr. D.Y.Patil Dental College and Hospital, Pimpri, Pune-18, India 1Department of Oral Pathology, GITAM Dental College, Vishakhapattanam, India Corresponding Author: Supriya Kheur, Department of Oral Pathology,Dr. D.Y.Patil Dental College and Hospital, Pimpri, Pune-18, India. Ph -09970150760, Email : [email protected] Abstract Mast cells in oral tissues releases various pro-inflammatory cytokine tumor necrosis factor alpha (TNF-Ü) which promotes leukocyte infiltration in various inflammatory condition of oral cavity such as oral lichen planus (OLP), periapical lesions, gingivitis & periodontitis. T lymphocyte derived cytokines influences mast cell migration & mediator release. Mast cell secreted proteases, activates matrix-metalloprotinases-9 (MMP-9) which may contribute to alteration in basement membrane in inflammatory condition such as Lichen Planus. Hence by understanding the role of mast cells in the pathogenesis of various diseases; therapies should be targeted to enhance the prognosis of the diseases. Key Words: Mast cells, Degranulation, Cytokines, Tryptase, Chymase. Introduction chemotactins, cell activating & cell growth Mast cells (MC) are large spherical or factor. Tissue mast cells are not homogenous elliptical mononuclear cells found in a variety for eg. enzymes within granules of mucosal & of tissues including skin, submucosa or connective tissue mast cells are different from connective tissue of various organs & each other. The ranges of mast cell activity is (1) specialized for their anatomic location, as the mucosal epithelial tissues & also in dental granules are different for mucosal and pulp. -

ISSN: 2320-5407 Int. J. Adv. Res. 7(10), 979-1021
ISSN: 2320-5407 Int. J. Adv. Res. 7(10), 979-1021 Journal Homepage: - www.journalijar.com Article DOI: 10.21474/IJAR01/9916 DOI URL: http://dx.doi.org/10.21474/IJAR01/9916 RESEARCH ARTICLE MINOR ORAL SURGICAL PROCEDURES. Harsha S K., Rani Somani and Shipra Jaidka. 1. Postgraduate Student, Department of Pediatric and Preventive Dentistry, Divya Jyoti college of Dental Sciences & Research, Modinagar, UP, India. 2. Professor and Head of the Department, Department of Pediatric and Preventive Dentistry, Divya Jyoti College of Dental Sciences & Research, Modinagar, UP, India. 3. Professor, Department of Pediatric and Preventive Dentistry, Divya Jyoti College of Dental Sciences & Research, Modinagar, UP, India. ……………………………………………………………………………………………………………………….... Manuscript Info Abstract ……………………. ……………………………………………………………… Manuscript History Minor oral surgery includes removal of retained or burried roots, Received: 16 August 2019 broken teeth, wisdom teeth and cysts of the upper and lower jaw. It also Final Accepted: 18 September 2019 includes apical surgery and removal of small soft tissue lesions like Published: October 2019 mucocele, ranula, high labial or lingual frenum etc in the mouth. These procedures are carried out under local anesthesia with or without iv Key words:- Gamba grass, accessions, yield, crude sedation and have relatively short recovery period. protein, mineral contents, Benin. Copy Right, IJAR, 2019,. All rights reserved. …………………………………………………………………………………………………….... Introduction:- Children are life‟s greatest gifts. The joy, curiosity and energy all wrapped up in tiny humans. This curiosity and lesser motor coordination usually leads to increased incidence of falls in children which leads to traumatic dental injuries. Trauma to the oral region may damage teeth, lips, cheeks, tongue, and temporomandibular joints. These traumatic injuries are the second most important issue in dentistry, after the tooth decay. -

Oxford® Policy Update Bulletin: December 2015 Oxford
Oxford December 2015 policy update bulletin Medical & Administrative Policy Updates UnitedHealthcare respects the expertise of the physicians, health care professionals, and their staff who participate in our network. Our goal is to support you and your patients in making the most informed decisions regarding the choice of quality and cost-effective care, and to support practice staff with a simple and predictable administrative experience. The Policy Update Bulletin was developed to share important information regarding Oxford® Medical and Administrative Policy updates.* *Where information in this bulletin conflicts with applicable state and/or federal law, Oxford® follows such applicable federal and/or state law Oxford Oxford® Medical and Administrative Policy Updates Overview This bulletin provides complete details on Oxford® Medical and Policy Update Classifications Administrative Policy updates. The appearance of a service or New procedure in this bulletin indicates only that Oxford® has recently New clinical coverage criteria and/or documentation review requirements adopted a new policy and/or updated, revised, replaced or have been adopted for a service, procedure, test, or device retired an existing policy; it does not imply that Oxford® provides Updated coverage for the service or procedure. In the event of an An existing policy has been reviewed and changes have not been made inconsistency or conflict between the information provided in this to the clinical coverage criteria or documentation review requirements; bulletin and the posted policy, the provisions of the posted policy however, items such as the clinical evidence, FDA information, and/or will prevail. Note that most benefit plan documents exclude from list(s) of applicable codes may have been updated benefit coverage health services identified as investigational or unproven/not medically necessary. -

A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated Through 445 Nm Diode Laser
healthcare Case Report A Single Case Report of Granular Cell Tumor of the Tongue Successfully Treated through 445 nm Diode Laser Maria Vittoria Viani 1,*, Luigi Corcione 1, Chiara Di Blasio 2, Ronell Bologna-Molina 3 , Paolo Vescovi 1 and Marco Meleti 1 1 Department of Medicine and Surgery, University of Parma, 43126 Parma, Italy; [email protected] (L.C.); [email protected] (P.V.); [email protected] (M.M.) 2 Private practice, Centro Medico Di Blasio, 43121 Parma; Italy; [email protected] 3 Faculty of Dentistry, University of the Republic, 14600 Montevideo, Uruguay; [email protected] * Correspondence: [email protected] Received: 10 June 2020; Accepted: 11 August 2020; Published: 13 August 2020 Abstract: Oral granular cell tumor (GCT) is a relatively rare, benign lesion that can easily be misdiagnosed. Particularly, the presence of pseudoepitheliomatous hyperplasia might, in some cases, lead to the hypothesis of squamous cell carcinoma. Surgical excision is the treatment of choice. Recurrence has been reported in up to 15% of cases treated with conventional surgery. Here, we reported a case of GCT of the tongue in a young female patient, which was successfully treated through 445 nm diode laser excision. Laser surgery might reduce bleeding and postoperative pain and may be associated with more rapid healing. Particularly, the vaporization effect on remnant tissues could eliminate GCT cells on the surgical bed, thus hypothetically leading to a lower rate of recurrence. In the present case, complete healing occurred in 1 week, and no recurrence was observed after 6 months. Laser surgery also allows the possibility to obtain second intention healing. -

Oral Mucocele – Diagnosis and Management
Journal of Dentistry, Medicine and Medical Sciences Vol. 2(2) pp. 26-30, November 2012 Available online http://www.interesjournals.org/JDMMS Copyright ©2012 International Research Journals Review Oral Mucocele – Diagnosis and Management Prasanna Kumar Rao 1, Divya Hegde 2, Shishir Ram Shetty 3, Laxmikanth Chatra 4 and Prashanth Shenai 5 1Associate Professor, Department of Oral Medicine and Radiology, Yenepoya Dental College, Yenepoya University, Deralakatte, Nithyanandanagar Post, Mangalore, Karnataka, India. 2Assistant Professor, Department of Obstetrics and Gynecology, AJ Institute of Medical Sciences, Mangalore, Karnataka, India. 3Reader, Department of Oral Medicine and Radiology, AB Shetty Memorial Institute of Dental Sciences, Nitte University, Mangalore, Karnataka, India. 4Senior Professor and Head, Department of Oral Medicine and Radiology, Yenepoya Dental College, Yenepoya University, Deralakatte, Nithyanandanagar Post, Mangalore, Karnataka, India. 5Senior Professor, Department of Oral Medicine and Radiology, Yenepoya Dental College, Yenepoya University, Deralakatte, Nithyanandanagar Post, Mangalore, Karnataka, India. ABSTRACT Mucocele are common salivary gland disorder which can be present in the oral cavity, appendix, gall bladder, paranasal sinuses or lacrimal sac. Common location for these lesions in oral cavity is lower lip however it also presents on other locations like tongue, buccal mucosa, soft palate, retromolar pad and lower labial mucosa. Trauma and lip biting habits are the main cause for these types of lesions. These are painless lesions which can be diagnosed clinically. In this review, a method used for searching data includes various internet sources and relevant electronic journals from the Pub Med and Medline. Keywords: Mucocels, Lower lip, Retention cyst. INTRODUCTION Mucocele is defined as a mucus filled cyst that can Types appear in the oral cavity, appendix, gall bladder, paranasal sinuses or lacrimal sac (Baurmash, 2003; Clinically there are two types, extravasation and retention Ozturk et al., 2005). -

Prescription Drugs Requiring Prior Authorization
PRESCRIPTION DRUGS REQUIRING PRIOR AUTHORIZATION Revised 10/16 As part of our drug utilization management program, members must request and receive prior authorization for certain prescription drugs in order to use their prescription drug benefits. Below is a list of drugs that currently require prior authorization. This list will be updated periodically as new drugs that require prior authorization are introduced. As benefits may vary by group and individual plans, the inclusion of a medication on this list does not imply prescription drug coverage. The Schedule of Benefits contains a list of drug categories that require prior authorization. Prior authorization requests are processed by our pharmacy benefit manager, Express Scripts, Inc. (ESI). Physicians must call ESI to obtain an authorization. (1-800-842-2015). Drug Name Generic Name Drug Classification Abstral fentanyl citrate oral tablet Controlled Dangerous Substance Accu-Chek Test Strips blood glucose test strips Blood Glucose Test Strips Actemra tocilizumab Monoclonal Antibody Acthar corticotropin Hormone Actimmune interferon gamma 1b Interferon Actiq fentanyl citrate OTFC Controlled Dangerous Substance Adcirca tadalafil Pulmonary Vasodilator Adempas riociguat Pulmonary Vasodilator Adlyxin lixisenatide Type 2 Diabetes Advocate Test Strips blood glucose test strips Blood Glucose Test Strips Aerospan** flunisolide Corticosteroids (Inhaled) Afrezza insulin Insulin (inhaled) Ampyra dalfampridine Multiple Sclerosis Agent Altoprev** lovastatin Cholesterol Alvesco** ciclesonide Corticosteroids -

Download Download
628 Indian Journal of Forensic Medicine & Toxicology, July-September 2021, Vol. 15, No. 3 Tongue Lesions - A Review N.Anitha1, Dharini Jayachandran2 1Reader, Department of Oral Pathology and Microbiology,2Undergraduate Student, Sree Balaji Dental College and Hospital, Bharath Institute of Higher Education and Research Abstract Tongue is a vital organ within the oral cavity that has varied function,and it may act as an index for the underlying systemic diseases.The investigation of the tongue diseases may begin with mere clinical examination .This review is to highlight the signs and symptoms of the various lesions that affects the tongue and especially to talk in brief about the benign and malignant tumours that affect the tongue along with other inherited and congenital abnormalities.Tongue lesions are categorized as tumours,infections, reactionary,congenital,developmental,acquired,autoimmune and potentially malignant disorders for easy understanding and to arrive at appropriate diagnosis.Tongue playing an important role in maintaining the harmony in the oral environment,it should be treated from diseases. Keywords: Tongue lesions,benign tumours,malignant tumours,diseases of tongue. CLASSIFICATION OF LESIONS ● Pyogenic granuloma AFFECTING THE TONGUE. ● Frictional keratosis BENIGN TUMOURS OF THE TONGUE INFECTIOUS LESIONS OF TONGUE ● Capillary hemangioma ● Oral squamous papilloma ● Fibroma ● Oral hairy leukoplakia ● Cavernous hemangioma ● Candidiasiis ● Giant cell granuloma ● Median rhomboid glossitis ● Lipoma ● Sublingual abcess ● Lymphangioma INHERITED,CONGENITAL,DEVELOPMENT ● Schwannoma AND ACQUIRED ABNORMALITIES OF TONGUE MALIGNANT TUMOURS OF TONGUE ● White sponge nevus ● Squamous cell carcinoma ● Foliate papillitis ● Veruccous carcinoma ● Angina bullosa hemorrhagica ● Non-Hodgkin’s lymphoma ● Geographic tongue TRAUMATIC/REACTIONARY LESIONS OF ● Fissured tongue THE TONGUE ● Median rhomboid glossitis ● Fibrous reactive hyperplasia ● Bifurcated/tetrafurcated tongue ● Traumatic ulcer Indian Journal of Forensic Medicine & Toxicology, July-September 2021, Vol. -

Orofacial Granulomatosis
Al-Hamad, A; Porter, S; Fedele, S; (2015) Orofacial Granulomatosis. Dermatol Clin , 33 (3) pp. 433- 446. 10.1016/j.det.2015.03.008. Downloaded from UCL Discovery: http://discovery.ucl.ac.uk/1470143 ARTICLE Oro-facial Granulomatosis Arwa Al-Hamad1, 2, Stephen Porter1, Stefano Fedele1, 3 1 University College London, UCL Eastman Dental Institute, Oral Medicine Unit, 256 Gray’s Inn Road, WC1X 8LD, London UK. 2 Dental Services, King Abdulaziz Medical City-Riyadh, Ministry of National Guard, Riyadh, Saudi Arabia. 3 NIHR University College London Hospitals Biomedical Research Centre, London, UK. Acknowledgments: Part of this work was undertaken at University College London/University College London Hospital, which received a proportion of funding from the Department of Health’s National Institute for Health Research Biomedical Research Centre funding scheme. Conflicts of Interest: The authors declare that they have no affiliation with any organization with a financial interest, direct or indirect, in the subject matter or materials discussed in the manuscript that may affect the conduct or reporting of the work submitted. Authorship: all authors named above meet the following criteria of the International Committee of Medical Journal Editors: 1) Substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; 2) Drafting the article or revising it critically for important intellectual content; 3) Final approval of the version to be published. Corresponding author: Dr. Stefano Fedele DDS, PhD