OSTEOARTHRITIS – an OVERVIEW Richard A. Sweet M.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
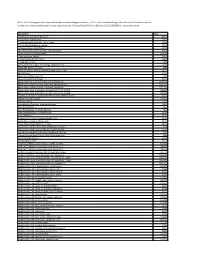
NOTE: the Following Are Shirley Ryan Abilitylab's Standard Charges As of Jan. 1, 2019. These Standard Charges Often Do Not
NOTE: The following are Shirley Ryan AbilityLab's standard charges as of Jan. 1, 2019. These standard charges often do not reflect what a patient or their insurance company/payer may be required to pay. Contact Patient Financial Services at 312-238-6039 for more information. Description Price 11-Deoxycortisol, Urine Random $531 12 Lead Ekg, Tracing Only $245 17 Hydroxycorticosteroids, Urine Timed $363 17 Hydroxyprogesterone, Serum $172 17 Ketosteroids, Urine Timed $273 17-Ketosteroids with Creatinine, Urine Random $273 2D Gait Analysis Charge(95999) $2,174 5' Nucleotidase, Serum $269 5.5 PDC PEDS CUFFED TRACH $226 5-HIAA-24 Hr Urine $99 A4566 Shoulder sling or vest design, abduction res $226 A4595 FES Electrode, each $38 A6545 Gradient Compression Wrap, Non-Elastic, Belo $171 ABO Rh Type $106 Above Knee Nylon Hose PR $83 Above Knee Suction Sheath $131 Above knee, for proximal femoral focal deficiency, $14,344 Above knee, molded socket, open end, SACH foot, en $10,751 Above knee, molded socket, single axis constant fr $10,935 Above knee, short prosthesis, no knee joint (""stu_L5210 $8,682 Above knee, short prosthesis, no knee joint (""stu_L5220 $7,429 ACAPELLA DH GREEN VIBRATORY PEP W/MOUTHPIECE DEVIC $181 Acetabuloplasty (27120) $4,493 Acetone, Serum $27 Acetylcholine Receptor Binding Antibody $405 Acid Phosphatase $66 Acid Phosphatase, Prostatic fraction $66 ACNE SURGERY MILIA CYSTS (10040) $530 Acorn Nebulizer $174 Activated PTT/Partial Thromboplastin Time $109 Active Wound Care > 20 cm Units $171 Active Wound Care/20 cm or < Units $171 Acupuncture with E-Stim. Each additional 15 minute $65 Acupuncture with E-Stim. -

Dexamethasone Sodium Phosphate Injection, USP)
HEXADROL® PHOSPHATE INJECTION (dexamethasone sodium phosphate injection, USP) DESCRIPTION — Hexadrol® Phosphate Injection (dexamethasone sodium phosphate injection, USP) is a water-soluble inorganic ester of dexamethasone which produces a rapid response even when injected intramuscularly. Dexamethasone Sodium Phosphate, C22H28FNa2O8P, has a molecular weight of 516.41 and chemically is Pregn-4-ene-3, 20-dione, 9-fluoro-11, 17-dihydroxy-16-methyl-21 (phosphonooxy)-, disodium salt, (11β, 16α). It occurs as a white to creamy white powder, is exceedingly hygroscopic, is soluble in water and its solutions have a pH between 7.5 and 10.5. It has the following structural formula: Hexadrol® Phosphate Injection is available in 4 mg/mL and 10 mg/mL concentrations. Each mL of Hexadrol® Phosphate Injection 4 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 4 mg dexamethasone phosphate; 1 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. 1 Reference ID: 3593917 Each mL of Hexadrol® Phosphate Injection 10 mg/mL, contains dexamethasone sodium phosphate, USP equivalent to 10 mg dexamethasone phosphate; 1.5 mg sodium sulfite; 10 mg benzyl alcohol (preservative). Made isotonic with sodium citrate. pH adjusted with citric acid or sodium hydroxide. ACTIONS — Naturally occurring glucocorticoids (hydrocortisone), which also have salt- retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs are primarily used for their potent anti-inflammatory effects in disorders of many organ systems. Glucocorticoids cause profound and varied metabolic effects. In addition, they modify the body’s immune responses to diverse stimuli. -

Vertebroplasty (Repair of Vertebrae with Bone Cement)
Patient information – Radiology Unit Tel 0118 322 7991 Vertebroplasty (repair of vertebrae with bone cement) Introduction This leaflet tells you about the procedure known as “vertebroplasty”, explains what is involved, the benefits and possible risks. It is not meant to replace informed discussion between you and your doctor but can act as a starting point for such a discussion. You should have plenty of time to discuss this procedure with the doctor who will be performing the procedure. What is vertebroplasty? Vertebroplasty is a procedure used to strengthen a collapsed spinal vertebra that has fractured and usually lost height due to osteoporosis or, less commonly, tumour infiltration or trauma. Vertebroplasty is primarily aimed at relieving the patient’s pain, to allow a rapid return to the previous level of activity, and secondarily to prevent further vertebral collapse. It is minimally invasive which means that patients suffer less disruption, face less risk and recover more quickly than with conventional open surgery. It is most effective when the fracture is relatively recent and particularly in patients who are very debilitated by the pain of the fracture or who cannot tolerate adequate quantities of painkilling medication. In some circumstances, vertebroplasty can be very effective even if the fracture is many months or even years old. Vertebroplasty is accomplished by injecting orthopaedic cement through a needle into the fractured bone; essentially forming an internal cast to stabilise the fracture similar to the principle of using plaster cast on an arm fracture. Typically, vertebroplasty is recommended if simpler treatments, such as bed rest, back bracing or pain medication have been ineffective, or if the side effects of analgesia have become problematic, such as causing stomach ulcers or drowsiness. -

Oxford® Policy Update Bulletin: December 2015 Oxford
Oxford December 2015 policy update bulletin Medical & Administrative Policy Updates UnitedHealthcare respects the expertise of the physicians, health care professionals, and their staff who participate in our network. Our goal is to support you and your patients in making the most informed decisions regarding the choice of quality and cost-effective care, and to support practice staff with a simple and predictable administrative experience. The Policy Update Bulletin was developed to share important information regarding Oxford® Medical and Administrative Policy updates.* *Where information in this bulletin conflicts with applicable state and/or federal law, Oxford® follows such applicable federal and/or state law Oxford Oxford® Medical and Administrative Policy Updates Overview This bulletin provides complete details on Oxford® Medical and Policy Update Classifications Administrative Policy updates. The appearance of a service or New procedure in this bulletin indicates only that Oxford® has recently New clinical coverage criteria and/or documentation review requirements adopted a new policy and/or updated, revised, replaced or have been adopted for a service, procedure, test, or device retired an existing policy; it does not imply that Oxford® provides Updated coverage for the service or procedure. In the event of an An existing policy has been reviewed and changes have not been made inconsistency or conflict between the information provided in this to the clinical coverage criteria or documentation review requirements; bulletin and the posted policy, the provisions of the posted policy however, items such as the clinical evidence, FDA information, and/or will prevail. Note that most benefit plan documents exclude from list(s) of applicable codes may have been updated benefit coverage health services identified as investigational or unproven/not medically necessary. -

Septic Arthritis of the Sternoclavicular Joint
J Am Board Fam Med: first published as 10.3122/jabfm.2012.06.110196 on 7 November 2012. Downloaded from BRIEF REPORT Septic Arthritis of the Sternoclavicular Joint Jason Womack, MD Septic arthritis is a medical emergency that requires immediate action to prevent significant morbidity and mortality. The sternoclavicular joint may have a more insidious onset than septic arthritis at other sites. A high index of suspicion and judicious use of laboratory and radiologic evaluation can help so- lidify this diagnosis. The sternoclavicular joint is likely to become infected in the immunocompromised patient or the patient who uses intravenous drugs, but sternoclavicular joint arthritis in the former is uncommon. This case series describes the course of 2 immunocompetent patients who were treated conservatively for septic arthritis of the sternoclavicular joint. (J Am Board Fam Med 2012;25: 908–912.) Keywords: Case Reports, Septic Arthritis, Sternoclavicular Joint Case 1 of admission, he continued to complain of left cla- A 50-year-old man presented to his primary care vicular pain, and the course of prednisone failed to physician with a 1-week history of nausea, vomit- provide any pain relief. The patient denied any ing, and diarrhea. His medical history was signifi- current fevers or chills. He was afebrile, and exam- cant for 1 episode of pseudo-gout. He had no ination revealed a swollen and tender left sterno- chronic medical illnesses. He was noted to have a clavicular (SC) joint. The prostate was normal in heart rate of 60 beats per minute and a blood size and texture and was not tender during palpa- pressure of 94/58 mm Hg. -

Adult Still's Disease
44 y/o male who reports severe knee pain with daily fevers and rash. High ESR, CRP add negative RF and ANA on labs. Edward Gillis, DO ? Adult Still’s Disease Frontal view of the hands shows severe radiocarpal and intercarpal joint space narrowing without significant bony productive changes. Joint space narrowing also present at the CMC, MCP and PIP joint spaces. Diffuse osteopenia is also evident. Spot views of the hands after Tc99m-MDP injection correlate with radiographs, showing significantly increased radiotracer uptake in the wrists, CMC, PIP, and to a lesser extent, the DIP joints bilaterally. Tc99m-MDP bone scan shows increased uptake in the right greater than left shoulders, as well as bilaterally symmetric increased radiotracer uptake in the elbows, hands, knees, ankles, and first MTP joints. Note the absence of radiotracer uptake in the hips. Patient had bilateral total hip arthroplasties. Not clearly evident are bilateral shoulder hemiarthroplasties. The increased periprosthetic uptake could signify prosthesis loosening. Adult Stills Disease Imaging Features • Radiographs – Distinctive pattern of diffuse radiocarpal, intercarpal, and carpometacarpal joint space narrowing without productive bony changes. Osseous ankylosis in the wrists common late in the disease. – Joint space narrowing is uniform – May see bony erosions. • Tc99m-MDP Bone Scan – Bilaterally symmetric increased uptake in the small and large joints of the axial and appendicular skeleton. Adult Still’s Disease General Features • Rare systemic inflammatory disease of unknown etiology • 75% have onset between 16 and 35 years • No gender, race, or ethnic predominance • Considered adult continuum of JIA • Triad of high spiking daily fevers with a skin rash and polyarthralgia • Prodromal sore throat is common • Negative RF and ANA Adult Still’s Disease General Features • Most commonly involved joint is the knee • Wrist involved in 74% of cases • In the hands, interphalangeal joints are more commonly affected than the MCP joints. -

Prescription Drugs Requiring Prior Authorization
PRESCRIPTION DRUGS REQUIRING PRIOR AUTHORIZATION Revised 10/16 As part of our drug utilization management program, members must request and receive prior authorization for certain prescription drugs in order to use their prescription drug benefits. Below is a list of drugs that currently require prior authorization. This list will be updated periodically as new drugs that require prior authorization are introduced. As benefits may vary by group and individual plans, the inclusion of a medication on this list does not imply prescription drug coverage. The Schedule of Benefits contains a list of drug categories that require prior authorization. Prior authorization requests are processed by our pharmacy benefit manager, Express Scripts, Inc. (ESI). Physicians must call ESI to obtain an authorization. (1-800-842-2015). Drug Name Generic Name Drug Classification Abstral fentanyl citrate oral tablet Controlled Dangerous Substance Accu-Chek Test Strips blood glucose test strips Blood Glucose Test Strips Actemra tocilizumab Monoclonal Antibody Acthar corticotropin Hormone Actimmune interferon gamma 1b Interferon Actiq fentanyl citrate OTFC Controlled Dangerous Substance Adcirca tadalafil Pulmonary Vasodilator Adempas riociguat Pulmonary Vasodilator Adlyxin lixisenatide Type 2 Diabetes Advocate Test Strips blood glucose test strips Blood Glucose Test Strips Aerospan** flunisolide Corticosteroids (Inhaled) Afrezza insulin Insulin (inhaled) Ampyra dalfampridine Multiple Sclerosis Agent Altoprev** lovastatin Cholesterol Alvesco** ciclesonide Corticosteroids -

Joint Pain Or Joint Disease
ARTHRITIS BY THE NUMBERS Book of Trusted Facts & Figures 2020 TABLE OF CONTENTS Introduction ............................................4 Medical/Cost Burden .................................... 26 What the Numbers Mean – SECTION 1: GENERAL ARTHRITIS FACTS ....5 Craig’s Story: Words of Wisdom What is Arthritis? ...............................5 About Living With Gout & OA ........................ 27 Prevalence ................................................... 5 • Age and Gender ................................................................ 5 SECTION 4: • Change Over Time ............................................................ 7 • Factors to Consider ............................................................ 7 AUTOIMMUNE ARTHRITIS ..................28 Pain and Other Health Burdens ..................... 8 A Related Group of Employment Impact and Medical Cost Burden ... 9 Rheumatoid Diseases .........................28 New Research Contributes to Osteoporosis .....................................9 Understanding Why Someone Develops Autoimmune Disease ..................... 28 Who’s Affected? ........................................... 10 • Genetic and Epigenetic Implications ................................ 29 Prevalence ................................................... 10 • Microbiome Implications ................................................... 29 Health Burdens ............................................. 11 • Stress Implications .............................................................. 29 Economic Burdens ........................................ -

Joint Injection As an Out-Patient Procedure
This leaflet is available in large print, Braille and on tape. Please contact Geoff Pennock on 0151 604 7289. Joint Injection As An Out-Patient Procedure Wirral University Teaching Hospital NHS Foundation Trust operates a No Smoking Policy. Please refrain from smoking on site. Information for Patients Orthopaedic Clinic Author: K Howard Date of Publication: June 2013 Date for Review: June 2015 Reference: Taken from the BUPA information leaflet. Having an injection into the joint. PL/00293/Surgical-Ortho/0613 Do Not Copy. For further copies contact Supplies quoting the PL number. This leaflet provides some information The risks of a joint injection In order to get maximum benefit from about joint injections. Please take Joint injections are a commonly your injection;- this home for further referral. Your performed and are generally safe consultant has prescribed this treatment procedures. Adverse reactions and • Rest the joint for a day. You may to meet your individual needs. Please side effects are rare; some patients need to take time off work, this will raise any concerns or questions you experience quite a painful reaction depend on the type of job you do – have and we will endeavour to answer after the injection lasting two-four your consultant will advise. them. days, this will normally settle. However, • You may need to take occasional if you do experience excessive pain, pain relieving medication e.g. The benefits of a joint injection swelling or you become unwell with Paracetamol, or anti- inflammatory The purpose of administering a a temperature, contact your doctor or tablets. joint injection is to reduce pain, the clinic immediately. -

Approach to Polyarthritis for the Primary Care Physician
24 Osteopathic Family Physician (2018) 24 - 31 Osteopathic Family Physician | Volume 10, No. 5 | September / October, 2018 REVIEW ARTICLE Approach to Polyarthritis for the Primary Care Physician Arielle Freilich, DO, PGY2 & Helaine Larsen, DO Good Samaritan Hospital Medical Center, West Islip, New York KEYWORDS: Complaints of joint pain are commonly seen in clinical practice. Primary care physicians are frequently the frst practitioners to work up these complaints. Polyarthritis can be seen in a multitude of diseases. It Polyarthritis can be a challenging diagnostic process. In this article, we review the approach to diagnosing polyarthritis Synovitis joint pain in the primary care setting. Starting with history and physical, we outline the defning characteristics of various causes of arthralgia. We discuss the use of certain laboratory studies including Joint Pain sedimentation rate, antinuclear antibody, and rheumatoid factor. Aspiration of synovial fuid is often required for diagnosis, and we discuss the interpretation of possible results. Primary care physicians can Rheumatic Disease initiate the evaluation of polyarthralgia, and this article outlines a diagnostic approach. Rheumatology INTRODUCTION PATIENT HISTORY Polyarticular joint pain is a common complaint seen Although laboratory studies can shed much light on a possible diagnosis, a in primary care practices. The diferential diagnosis detailed history and physical examination remain crucial in the evaluation is extensive, thus making the diagnostic process of polyarticular symptoms. The vast diferential for polyarticular pain can difcult. A comprehensive history and physical exam be greatly narrowed using a thorough history. can help point towards the more likely etiology of the complaint. The physician must frst ensure that there are no symptoms pointing towards a more serious Emergencies diagnosis, which may require urgent management or During the initial evaluation, the physician must frst exclude any life- referral. -

Arthritis and Joint Pain
Fact Sheet News from the IBD Help Center ARTHRITIS AND JOINT PAIN Arthritis, or inflammation (pain with swelling) of the joints, is the most common extraintestinal complication of IBD. It may affect as many as 30% of people with Crohn’s disease or ulcerative colitis. Although arthritis is typically associated with advancing age, in IBD it often strikes younger patients as well. In addition to joint pain, arthritis also causes swelling of the joints and a reduction in flexibility. It is important to point out that people with arthritis may experience arthralgia, but many people with arthralgia may not have arthritis. Types of Arthritis • Peripheral Arthritis. Peripheral arthritis usually affects the large joints of the arms and legs, including the elbows, wrists, knees, and ankles. The discomfort may be “migratory,” moving from one joint to another. If left untreated, the pain may last from a few days to several weeks. Peripheral arthritis tends to be more common among people who have ulcerative colitis or Crohn’s disease of the colon. The level of inflammation in the joints generally mirrors the extent of inflammation in the colon. Although no specific test can make an absolute diagnosis, various diagnostic methods—including analysis of joint fluid, blood tests, and X-rays—are used to rule out other causes of joint pain. Fortunately, IBD-related peripheral arthritis usually does not cause any lasting damage and treatment of the underlying IBD typically results in improvement in the joint discomfort. • Axial Arthritis. Also known as spondylitis or spondyloarthropathy, axial arthritis produces pain and stiffness in the lower spine and sacroiliac joints (at the bottom of the back). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists.