Family Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proper Preop Makes for Easier Toenail Surgery
April 15, 2007 • www.familypracticenews.com Skin Disorders 25 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS sia using a digital block or a distal approach to take ef- Senior Writer fect. Premedication with NSAIDs, codeine, or dextro- propoxyphene also may be appropriate, he said. WASHINGTON — Proper early management of in- To cut away the offending section of nail, an English grown toenails may help to decrease the risk of recur- anvil nail splitter is inserted under the nail plate and the rence whether or not surgery is necessary, Dr. C. Ralph cut is made all the way to the proximal nail fold. The hy- Daniel III said at the annual meeting of the American pertrophic, granulated tissue should be cut away as well. Academy of Dermatology. Many ingrown toenails are recurrent, so Dr. Daniel per- “An ingrown nail is primarily acting as a foreign-body forms a chemical matricectomy in nearly all patients after reaction. That rigid spicule penetrates soft surrounding tis- making sure that the surgical field is dry and bloodless. sue” and produces swelling, granulation tissue, and some- The proximal nail fold can be flared back to expose more times a secondary infection, said Dr. Daniel of the de- of the proximal matrix if necessary. Dr. Daniel inserts a Cal- partments of dermatology at the University of Mississippi, giswab coated with 88% phenol or 10% sodium hydroxide Jackson, and the University of Alabama, Birmingham. and applies the chemical for 30 seconds to the portion of For the early management of stage I ingrown toenails the nail matrix that needs to be destroyed. -

Nail Problems
Nail Problems Components of the Nail Congenital Disorders Racket nails, characterized by a broad short thumb nail, is the commonest congenital nail defect, dominantly inherited and seen in 1% of the population. The basic abnormality is shortness of the underlying terminal phalanx. In the yellow nail syndrome, the nail changes begin in adult life, against a background of hypoplasia of the lymphatic system. Peripheral edema is usually present and pleural effusions may occur. The nails grow very slowly and become thickened and greenish-yellow; their surface is smooth but they are over curved from side to side. Acquired Nail Changes Beau's Lines Transverse lines or grooves in nail. Causes include any severe systemic illness or medications (chemotherapy), which affects growth of the nail matrix. Clinically: The grooves or lines move distally; the distance from the nail fold lets one assess the time of trauma. Onycholysis Separation of nail from nail bed. Causes include psoriasis, dermatitis, fungal infections; medications (photo-onycholysis from tetracyclines or psoralens), thyroid disease; rarely inherited. Idiopathic onycholysis is most common among women; painless separation of nail without apparent cause. Typically, the distal third separates and underlying nail bed becomes darker and thickened. Therapy: Cut nail very short to reduce leverage encouraging separation, apply antifungal solution. Usually self-limited process. Ingrown Nail Penetration of nail plate into tissue of lateral nail fold. Almost always involves great toes. Causes include congenital malformation of nail (pincer nail), improper trimming, and tightly fitting shoes. Clinically: Distorted nail with swelling, pain, and granulation tissue along the lateral nail fold. Therapy: Mild cases: Eliminate pressure, trim nail; topical antiseptics as foot soaks or on small piece of cotton wool pushed under affected nail. -

Proper Preop Makes for Easier Toenail Surgery
20 Dermatologic Surgery S KIN & ALLERGY N EWS • April 2007 Proper Preop Makes for Easier Toenail Surgery BY JEFF EVANS produces swelling, granulation tissue, and tor or a 1- to 2-mm curette. has served as a speaker, consultant, and in- Senior Writer sometimes a secondary infection, said Dr. He also uses a technique for early-stage vestigator for the company. Daniel of the departments of dermatol- ingrown toenails in which dental floss is in- A procedure that uses an acrylic-affixed WASHINGTON — Proper early man- ogy at the University of Mississippi, Jack- serted under the ingrown nail corner with- gutter splint has been reported to be suc- agement of ingrown toenails may help to son, and the University of Alabama, Birm- out anesthesia and is kept there to separate cessful for avoiding surgery, Dr. Daniel decrease the risk of recurrence whether or ingham. the nail edge from adjacent soft tissue (J. said. A plastic gutter tube is set under the not surgery is necessary, Dr. C. Ralph For the early management of stage I in- Am. Acad. Dermatol. 2004;50:939-40). ingrown part of the nail and acrylic is Daniel III said at the annual meeting of the grown toenails in which some granula- Dr. Daniel formerly was on the board of sculpted and allowed to polymerize American Academy of Dermatology. tion tissue but no infection is present, Dr. directors for Doak Dermatologics, a sub- around the ingrown part of the nail and “An ingrown nail is primarily acting as Daniel has trained his nurse to push wisps sidiary of Bradley Pharmaceuticals Inc., hold the gutter tube in place. -

Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition
Ingrown Nail/Paronychia Referral Guide: Podiatry Referral Page 1 of 1 Diagnosis/Definition: Redness, warmth, tenderness and exudate coming from the areas adjacent to the nail plate. Initial Diagnosis and Management: History and physical examination. In chronic infection appropriate radiographic (foot or toe series to rule out distal phalanx osteomyelitis) and laboratory evaluation (CBC and ESR). Ongoing Management and Objectives: Primary care should consist of Epsom salt soaks, or soapy water, and antibiotics for ten days. If Epsom salt soaks and antibiotics are ineffective, the primary care provider has the following options: Reevaluate and refer to podiatry. Perform temporary avulsion/I&D. Perform permanent avulsion followed by chemical cautery (89% Phenol or 10% NaOH application – 3 applications maintained for 30 second intervals, alcohol dilution between each application). Aftercare for all of the above is continued soaks, daily tip cleaning and bandage application. Indications for Specialty Care Referral: After the reevaluation at the end of the antibiotic period the primary care provider can refer the patient to Podiatry for avulsion/ surgical care if they do not feel comfortable performing the procedure themselves. The patient should be given a prescription for antibiotics renewal and orders to continue soaks until avulsion can be performed. Test(s) to Prepare for Consult: Test(s) Consultant May Need To Do: Criteria for Return to Primary Care: After completion of the surgical procedure, patients will be returned to the primary care provider for follow-up. Revision History: Created Revised Disclaimer: Adherence to these guidelines will not ensure successful treatment in every situation. Further, these guidelines should not be considered inclusive of all accepted methods of care or exclusive of other methods of care reasonably directed to obtaining the same results. -

Also Called Androgenetic Alopecia) Is a Common Type of Hereditary Hair Thinning
750 West Broadway Suite 905 - Vancouver BC V5Z 1H8 Phone: 604.283.9299 Fax: 604.648.9003 Email: [email protected] Web: www.donovanmedical.com Female Pattern Hair Loss Female pattern hair loss (also called androgenetic alopecia) is a common type of hereditary hair thinning. Although hair may become quite thin, women do not become bald as in men. Hair thinning starts as early as the teenage years, but usually in the twenties and thirties and is usually fully expressed by the age of 40. How can one recognize female pattern hair loss? § Typically, a female in her teens, twenties or thirties gradually becomes aware that she has less hair on the top of her head than previously. § She may notice that her scalp has become slightly visible now and it takes more effort to style the hair to hide the thinning. § The size of the ponytail becomes smaller in diameter. § While all this is happening, she may also notice that her hair becomes greasy and stringy more quickly and she shampoos more often to keep the hair looking fuller volume. § One of the earliest signs of androgenetic alopecia is widening of the ‘central part’ (down the middle of the scalp). The spacing between hairs gradually increases. The thinning gradually becomes diffuse and may be present all over the scalp but is usually most pronounced over the top and sides of the head. § There is much variation in the diameter and length of hairs – some and thick and long while others are fine and short. This variation in size represents the gradual miniaturization of hair follicles- they become smaller and smaller. -

Ingrown Toenails
POST-OP NAIL CARE The day following the procedure, remove the bandage and begin soaking the toe for 10-15 minutes at least once daily. If the bandage does not come off easily, soak in warm water with one (1) tablespoon Epson Salts. As you soak, use a cotton tipped applicator (Q-tip) to clean the nail groove. Also, gently pull the skin edges back from the area where the nail was removed to be sure that any draining is released. After drying the toes, apply a light amount of triple antibiotic ointment (Neosporin) or other topical anesthetic, and light gauze or a bandage (Band-aid). Gauze is best to absorb INGROWN drainage. After a few days, the toe may be Brian Gardner, D.P.M. TOENAILS overly moist and need to dry. Use less triple antibiotic, continue soaking, Podiatrist and dress with light gauze or a Dr. Brian Gardner specializes in bandage (Band-aid). As drying foot and ankle surgery, wound care, occurs, tenderness will usually biomechanics, sports medicine, decrease. Continue soaks until the diabetic foot care, area is no longer draining (usually and general foot care. several weeks, if the nail root was treated with a chemical). facebook.com/UintahBasinHealthcare www.ubh.org 435.725.2025, Roosevelt 435.781.2030, Vernal 250 W 300 N Clinic #2 Suite 203 (Level 2), Roosevelt, Utah 379 N 500 W, Vernal, Utah Nails grow from a root beneath the skin TREATMENT IMPORTANT called the “matrix.” This growth center TREATMENT INFORMATION can vary in size and shape. It may Initially, your doctor may be able to produce a nail which is flat, curved, trim the ingrown toenail. -

Customizable Wallet Cards
reason, we’ll refund your cost. your refund we’ll reason, cost. your refund we’ll reason, cost. your refund we’ll reason, cost. your refund we’ll reason, If you aren’t satisfied, for any any for satisfied, aren’t you If any for satisfied, aren’t you If any for satisfied, aren’t you If any for satisfied, aren’t you If waiting. No waiting. No waiting. No waiting. No apps to download. download. to apps No download. to apps No download. to apps No download. to apps No video required. required. video No required. deo vi No required. deo vi No required. deo vi No ne. li on t bu ne. li on t bu ne. li on t bu ne. li on t bu isit – – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik – isit v s doctor’ a e Lik Fold line Fold Your 24/7 Your 24/7 Your 24/7 Your 24/7 online clinic online clinic online clinic online clinic A visit is just $45.* Insurance is accepted and Insurance is accepted and Insurance is accepted and Insurance is accepted and Insurance is accepted. applies to your deductible. appInsurancelies to your is accepted.deductible. appInsurancelies to your is deductible.accepted. appInsurancelies to your is deductible.accepted. *No*No cost cost if we can’tcan't treat trea you.t you. *No*No cost cost ifif we can’tcan't treat trea tyou. you. *No*No costcost if wewe can’tcan't treat treat you. -

Procedural Review of Toenail Excision Scott Klosterman, DO, Candace Prince, OSM 4
Osteopathic Family Physician (2012) 4, 18-23 Procedural review of toenail excision Scott Klosterman, DO, Candace Prince, OSM 4 From Spartanburg Regional Family Medicine Residency Program, Spartanburg, SC KEYWORDS: Toenail removal is a common procedure that family physicians routinely perform in the office. This article Toenail removal; highlights the acute and chronic indications for toenail removal and its contraindications, potential compli- Paronychia; cations, and procedural details including digital block anesthesia. A sample consent form and patient Onychomycrosis; educational handout are provided as well as the current diagnostic International Classification of Diseases, Ingrown toenail; 9th revision, and current procedural terminology codes for the clinician to use. Matrixectomy © 2012 Elsevier Inc. All rights reserved. Family physicians are often the primary health care con- a partial or complete matrixectomy (permanent nail removal) tact for patients with toenail problems. Toenail complaints may be necessary for these chronic conditions, and with on- ranging from paronychia to onychomycosis affect every age ychocryptosis because of its high rate of recurrence.2,4,11 Fi- group, and surgical excision of the nail may be an appro- nally, in cases of growths or discoloration beneath the nail, nail priate treatment option. Our purpose is to review the indi- plate removal with biopsy may be needed to rule out malignant cations and procedural details for toenail removal, provide a neoplasms, although biopsy techniques of the nail and nail bed concise patient consent form and educational handout for are outside the scope of this review.2,3 postprocedural care, and review the current International Classification of Diseases, 9th revision (ICD-9) and current procedural terminology (CPT) coding for such procedures. -

A New Classification of Pattern Hair Loss That Is Universal for Men And
A new classification of pattern hair loss that is universal for men and women: Basic and specific (BASP) classification Won-Soo Lee, MD, PhD,a Byung In Ro, MD, PhD,b Seung Phil Hong, MD,a Hana Bak, MD,c Woo-Young Sim, MD, PhD,d Do Won Kim, MD, PhD,e Jang Kyu Park, MD, PhD,f Chull-Wan Ihm, MD, PhD,g Hee Chul Eun, MD, PhD,h Oh Sang Kwon, MD, PhD,h Gwang Seong Choi, MD, PhD,i Young Chul Kye, MD, PhD,j Tae Young Yoon, MD, PhD,k Seong-Jin Kim, MD, PhD,l Hyung Ok Kim, MD, PhD,m Hoon Kang, MD, PhD,m Jawoong Goo, MD,a Seok-Yong Ahn, MD,a Minjeong Kim, MD,a Soo Young Jeon, MD,a and Tak Heon Oh, MDa Wonju, Seoul, Daegu, Daejeon, Jeonju, Incheon, Choengju, and Gwangju, Korea Background: Pattern hair loss (PHL) can be classified into several patterns. Currently, the Hamiltone Norwood classification system for men and the Ludwig grade system for women are commonly used to describe patterns of hair loss. However, these pre-existing classifications have some limitations. Objective: To establish an acceptable, universal, and accurate standard of both male and female pattern hair loss and to report its use in determining the incidence of PHL. Methods: We developed a new classification system (BASP classification) and then applied this system to classify the types of PHL. The BASP classification was based on observed patterns of hair loss. The basic (BA) types represent the shape of the anterior hairline, and the specific types (SP) represent the density of hair on distinct areas (frontal and vertex). -

Dermatology Update
12/6/19 Dermatology Update Lindy P. Fox, MD Professor of Clinical Dermatology Director, Hospital Consultation Service Department of Dermatology University of California, San Francisco [email protected] I have no conflicts of interest to disclose I may be discussing off-label use of medications 1 1 Outline • Principles of topical therapy • Chronic Urticaria • Alopecia • Acne in the adult • Perioral dermatitis • Sunscreens 2 2 1 12/6/19 Principles of Dermatologic Therapy Moisturizers and Gentle Skin Care • Moisturizers – Contain oil to seal the surface of the skin and replace the damaged water barrier – Petrolatum (Vaseline) is the premier and “gold standard” moisturizer – Additions: water, glycerin, mineral oil, lanolin – Some try to mimic naturally occurring ceramides (E.g. CeraVe) • Thick creams more moisturizing than pump lotions 3 Principles of Dermatologic Therapy Moisturizers and Gentle Skin Care • Emolliate skin – All dry skin itches • Gentle skin care – Soap to armpits, groin, scalp only – Short cool showers or tub soak for 15-20 minutes – Apply medications and moisturizer within 3 minutes of bathing or swimming 4 2 12/6/19 Principles of Dermatologic Therapy Topical Medications • The efficacy of any topical medication is related to: 1. The concentration of the medication 2. The vehicle 3. The active ingredient (inherent strength) 4. Anatomic location 5 Vehicles • Ointment (like Vaseline): – Greasy, moisturizing, messy, most effective. • Creams (vanish when rubbed in): – Less greasy, can sting, more likely to cause allergy (preservatives/fragrances). -
Ingrown Toenails: Digging out the Facts
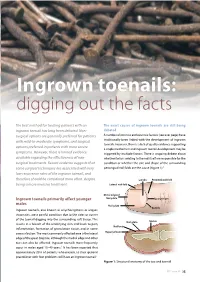
Ingrown toenails: digging out the facts The best method for treating patients with an The exact causes of ingrown toenails are still being ingrown toenail has long been debated. Non- debated surgical options are generally preferred for patients A number of intrinsic and extrinsic factors (see over page) have with mild-to-moderate symptoms, and surgical traditionally been linked with the development of ingrown toenails. However, there is a lack of quality evidence supporting options preferred in patients with more severe a single mechanism and ingrown toenail development may be symptoms. However, there is limited evidence triggered by multiple factors. There is ongoing debate about available regarding the effectiveness of non- whether factors relating to the nail itself are responsible for the surgical treatments. Recent evidence suggests that condition or whether the size and shape of the surrounding some surgical techniques are associated with very periungual nail folds are the cause (Figure 1).3 low recurrence rates of the ingrown toenail, and therefore should be considered more often, despite Lunula Proximal nail fold being a more invasive treatment. Lateral nail fold Distal edge of Ingrown toenails primarily affect younger Nail plate Eponychium males Nail plate The Foot Series Cuticle Ingrown toenails, also known as onychocryptosis or unguis incarnates, are a painful condition due to the sides or corner of the toenail digging into the surrounding soft tissue. This Nail plate Matrix results in a breach of the underlying skin and leads to pain, Nail bed inflammation, formation of granulation tissue, and in some cases infection. The most commonly affected area is the lateral Hyponychium edge of the great (big) toe, although the medial edge and other toes can also be affected. -

Female Pattern Hair Loss and Androgen Excess: a Report
REPORTS AND RECOMMENDATIONS Female Pattern Hair Loss and Androgen Excess: A Report From the Multidisciplinary Androgen Excess and Downloaded from https://academic.oup.com/jcem/article-abstract/104/7/2875/5342938 by Endocrine Society Member Access 2 user on 24 June 2019 PCOS Committee Enrico Carmina,1 Ricardo Azziz,2 Wilma Bergfeld,3,4 Héctor F. Escobar-Morreale,5,6,7 Walter Futterweit,8 Heather Huddleston,9 Rogerio Lobo,10 and Elise Olsen11,12 1Department of Health Sciences and Mother and Child Care, University of Palermo, 90121 Palermo, Italy; 2Department of Health Policy, Management, and Behavior, School of Public Health, University at Albany, State University of New York, Albany, New York 12144; 3Department of Dermatology, Cleveland Clinic, Cleveland, Ohio 44195; 4Department of Pathology, Cleveland Clinic, Cleveland, Ohio 44195; 5Department of Endocrinology and Nutrition, Hospital Universitario Ramon ´ y Cajal, Universidad de Alcala, ´ 28801 Madrid, Spain; 6Centro de Investigacion ´ Biomedica ´ en Red Diabetes y Enfermedades Metabolicas ´ Asociadas, 28029 Madrid Spain; 7Instituto Ramon ´ y Cajal de Investigacion ´ Sanitaria, 28034 Madrid, Spain; 8Mount Sinai School of Medicine, New York, New York 10029; 9Department of Obstetrics and Gynecology, University of California at San Francisco, San Francisco, California 94143; 10Department of Obstetrics and Gynecology, Columbia University, New York, New York 10032; 11Department of Dermatology, Duke University Medical Center, Durham, North Carolina 27710; and 12Department of Medicine, Duke University Medical Center, Durham, North Carolina 27710 ORCiD numbers: 0000-0001-7336-7610 (E. Carmina); 0000-0002-6890-1644 (H. F. Escobar-Morreale). Objective: To determine the current state of knowledge and provide evidence-based recommendations that could be valid for all specialists taking care of female pattern hair loss (FPHL), a common form of hair loss in women that is characterized by the reduction of hair density in the central area of the scalp, whereas the frontal hairline is generally well conserved.