Buffalo Medical Group, P.C. Robert E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Infectious Eccrine Hidradenitis Associated with Intense Sun Exposure
Infectious Eccrine Hidradenitis Associated With Intense Sun Exposure Charlotte Hwa Vuong, MD; Ruth Walters, MD; Jennifer A. Stein, MD, PhD Practice Points Neutrophilic eccrine hidradenitis is a response to nonspecific stimuli in a wide spectrum of clinical settings. Infectious eccrine hidradenitis should be included in the differential diagnosis in patients who develop an erythematous papular eruption after sunburn. Infectious eccrine hidradenitis (IEH), which usu- erythematous papules on the flanks, grouped pap- ally manifests as singular or multiple erythema- ules and pustules on the back, and papules on the tous papules or plaques, is a rare dermatosis legs in areas of resolving sunburn (Figure 1). It involving an infectious agent and histologic find- was her first sun exposure of the season, and the ings identical to that of CUTISneutrophilic eccrine patient previously had used the same sunscreen, hidradenitis (NEH). We report a case of IEH in which she applied on all parts of her body. Her cur- a 24-year-old woman who developed a pruritic, rent medications included desogestrel and ethinyl erythematous, papular rash after a sunburn. A estradiol, naratriptan hydrochloride, and loratadine culture of a pustule revealed methicillin-sensitive and pseudoephedrine. Staphylococcus aureus. Our patient had complete Histology showed a superficial and deep peri- resolution of her rash within 2 weeks of starting vascular infiltrate of lymphocytes, histiocytes, and amoxicillinDo and clavulanate. ThisNot case of IEH and neutrophils Copy with prominent neutrophilic infiltration NEH related to both intense sun exposure and of eccrine glands (Figure 2). In the overlying epider- infection supports the hypothesis that NEH is a mis, there was focal parakeratosis with a collection of response to nonspecific stimuli and may occur in neutrophils and an aggregate of gram-positive cocci. -

General Pathomorpholog.Pdf
Ukrаiniаn Medicаl Stomаtologicаl Аcаdemy THE DEPАRTАMENT OF PАTHOLOGICАL АNАTOMY WITH SECTIONSL COURSE MАNUАL for the foreign students GENERАL PАTHOMORPHOLOGY Poltаvа-2020 УДК:616-091(075.8) ББК:52.5я73 COMPILERS: PROFESSOR I. STАRCHENKO ASSOCIATIVE PROFESSOR O. PRYLUTSKYI АSSISTАNT A. ZADVORNOVA ASSISTANT D. NIKOLENKO Рекомендовано Вченою радою Української медичної стоматологічної академії як навчальний посібник для іноземних студентів – здобувачів вищої освіти ступеня магістра, які навчаються за спеціальністю 221 «Стоматологія» у закладах вищої освіти МОЗ України (протокол №8 від 11.03.2020р) Reviewers Romanuk A. - MD, Professor, Head of the Department of Pathological Anatomy, Sumy State University. Sitnikova V. - MD, Professor of Department of Normal and Pathological Clinical Anatomy Odessa National Medical University. Yeroshenko G. - MD, Professor, Department of Histology, Cytology and Embryology Ukrainian Medical Dental Academy. A teaching manual in English, developed at the Department of Pathological Anatomy with a section course UMSA by Professor Starchenko II, Associative Professor Prylutsky OK, Assistant Zadvornova AP, Assistant Nikolenko DE. The manual presents the content and basic questions of the topic, practical skills in sufficient volume for each class to be mastered by students, algorithms for describing macro- and micropreparations, situational tasks. The formulation of tests, their number and variable level of difficulty, sufficient volume for each topic allows to recommend them as preparation for students to take the licensed integrated exam "STEP-1". 2 Contents p. 1 Introduction to pathomorphology. Subject matter and tasks of 5 pathomorphology. Main stages of development of pathomorphology. Methods of pathanatomical diagnostics. Methods of pathomorphological research. 2 Morphological changes of cells as response to stressor and toxic damage 8 (parenchimatouse / intracellular dystrophies). -
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

Immunohistochemical Analysis of S100-Positive Epidermal
An Bras Dermatol. 2020;95(5):627---630 Anais Brasileiros de Dermatologia www.anaisdedermatologia.org.br DERMATOPATHOLOGY Immunohistochemical analysis of S100-positive ଝ,ଝଝ epidermal Langerhans cells in dermatofibroma Mahmoud Rezk Abdelwhaed Hussein Department of Pathology, Assuit University Hospital, Assuit, Egypt Received 3 February 2020; accepted 12 April 2020 Available online 12 July 2020 Abstract Dermatofibroma is a dermal fibrohistiocytic neoplasm. The Langerhans cells are the KEYWORDS immunocompetent cells of the epidermis, and they represent the first defense barrier of the Histiocytoma, benign immune system towards the environment. The objective was to immunohistologically compare fibrous; the densities of S100-positive Langerhans cells in the healthy peritumoral epidermis against Skin neoplasms; those in the epidermis overlying dermatofibroma (20 cases), using antibodies against the S100 S100 Proteins molecule (the immunophenotypic hallmark of Langerhans cells). The control group (normal, healthy skin) included ten healthy age and sex-matched individuals who underwent skin biopsies for benign skin lesions. A significantly high density of Langerhans cells was observed both in the epidermis of the healthy skin (6.00 ± 0.29) and the peritumoral epidermis (6.44 ± 0.41) vs. those in the epidermis overlying the tumor (1.44 ± 0.33, p < 0.05). The quantitative deficit of Langerhans cells in the epidermis overlying dermatofibroma may be a possible factor in its development. © 2020 Sociedade Brasileira de Dermatologia. Published by Elsevier Espana,˜ S.L.U. This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/). Langerhans cells (LCs) are the exclusive antigen-presenting tions stained with hematoxylin and eosin as ‘‘clear cells’’ cells of the normal human epidermis. -

Melasma (1 of 8)
Melasma (1 of 8) 1 Patient presents w/ symmetric hyperpigmented macules, which can be confl uent or punctate suggestive of melasma 2 DIAGNOSIS No ALTERNATIVE Does clinical presentation DIAGNOSIS confirm melasma? Yes A Non-pharmacological therapy • Patient education • Camoufl age make-up • Sunscreen B Pharmacological therapy Monotherapy • Hydroquinone or • Tretinoin TREATMENT Responding to No treatment? See next page Yes Continue treatment © MIMSas required Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B94 © MIMS 2019 Melasma (2 of 8) Patient unresponsive to initial therapy MELASMA A Non-pharmacological therapy • Patient education • Camoufl age make-up • Sunscreen B Pharmacological therapy Dual Combination erapy • Hydroquinone plus • Tretinoin or • Azelaic acid Responding to Yes Continue treatment treatment? as required No A Non-pharmacological therapy • Patient education • Camoufl age make-up • Sunscreen • Laser therapy • Dermabrasion B Pharmacological therapy Triple Combination erapy • Hydroquinone plus • Tretinoin plus • Topical steroid Chemical peels 1 MELASMA • Acquired hyperpigmentary skin disorder characterized by irregular light to dark brown macules occurring in the sun-exposed areas of the face, neck & arms - Occurs most commonly w/ pregnancy (chloasma) & w/ the use of contraceptive pills - Other factors implicated in the etiopathogenesis are photosensitizing medications, genetic factors, mild ovarian or thyroid dysfunction, & certain cosmetics • Most commonly aff ects Fitzpatrick skin phototypes III & IV • More common in women than in men • Rare before puberty & common in women during their reproductive years • Solar & ©ultraviolet exposure is the mostMIMS important factor in its development Not all products are available or approved for above use in all countries. -

Storiform Collagenoma: Case Report Colagenoma Estoriforme: Relato De Caso
CASE REPORT Storiform collagenoma: case report Colagenoma estoriforme: relato de caso Guilherme Flosi Stocchero1 ABSTRACT INTRODUCTION Storiform collagenoma is a rare tumor, which originates from the Storiform collagenoma or sclerotic fibroma is a rare proliferation of fibroblasts that show increased production of type-I benign skin tumor that usually affects young adults collagen. It is usually found in the face, neck and extremities, but and middle-age individuals of both sexes. This tumor is it can also appear in the trunk, scalp and, less frequently, in the slightly predominant in women. Storiform collagenoma oral mucosa and the nail bed. It affects both sexes, with a slight female predominance. It may be solitary or multiple, the latter being appears as a small papule or solid fibrous nodule. an important marker for Cowden syndrome. It presents as a painless, It is well-circumscribed, pink, whitish or skin color, solid nodular tumor that is slow-growing. It must be considered in the painless and of slow-growing. This tumor is often differential diagnosis of other well-circumscribed skin lesions, such as found in face and limbs, but it can also appears in dermatofibroma, pleomorphic fibroma, sclerotic lipoma, fibrolipoma, the chest, scalp and, rarely, in oral mucosa and nail giant cell collagenoma, benign fibrous histiocytoma, intradermal Spitz bed. Storiform collagenoma often appears as single nevus and giant cell angiohistiocytoma. tumor, and the occurrence of multiple tumors is an important indication of Cowden syndrome, which is Keywords: Collagen; Hamartoma; Skin neoplasms; Fibroma; Skin; Case a heritage genodermatosis of autosomal dominant reports condition.(1-4) Storiform collagenoma has as differential diagnosis other well-circumscribed skin tumors such RESUMO as dermatofibroma, pleomorphic fibroma, sclerotic O colagenoma estoriforme é um tumor raro originado a partir da lipoma, fibrolipoma, giant cell collagenoma, benign proliferação de fibroblastos com produção aumentada de colágeno tipo I. -
What Is Cosplay?
NO, REALLY: WHAT IS COSPLAY? Natasha Nesic A thesis submitted in partial fulfillment of the requirements for a B. A. in Anthropology with Honors. Mount Holyoke College May 2013 ACKNOWLEDGEMENTS “In anthropology, you can study anything.” This is what happens when you tell that to an impressionable undergrad. “No, Really: What is Cosplay?” would not have been possible without the individuals of the cosplay community, who gave their time, hotel room space, and unforgettable voices to this project: Tina Lam, Mario Bueno, Rob Simmons, Margaret Huey, Chris Torrey, Chris Troy, Calico Singer, Maxiom Pie, Cassi Mayersohn, Renee Gloger, Tiffany Chang, as well as the countless other cosplayers at AnimeNEXT, Anime Expo, and Otakon during the summer of 2012. A heap of gratitude also goes to Amanda Gonzalez, William Gonzalez, Kimberly Lee, Patrick Belardo, Elizabeth Newswanger, and Clara Bertagnolli, for their enthusiasm for this project—as well as their gasoline. And to my parents, Beth Gersh-Nesic and Dusan Nesic, who probably didn’t envision this eight years ago, letting me trundle off to my first animé convention in a homemade ninja getup and a face full of Watercolor marker. Many thanks as well to the Mount Holyoke College Anthropology Department, and the Office of Academic Deans for their financial support. Finally, to my advisor and mentor, Professor Andrew Lass: Mnogo hvala za sve. 1 Table of Contents Introduction.......................................................................................................................................3 -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment. -

White Lesions of the Oral Cavity and Derive a Differential Diagnosis Four for Various White Lesions
2014 self-study course four course The Ohio State University College of Dentistry is a recognized provider for ADA, CERP, and AGD Fellowship, Mastership and Maintenance credit. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to ADA CERP at www.ada.org/goto/cerp. The Ohio State University College of Dentistry is approved by the Ohio State Dental Board as a permanent sponsor of continuing dental education ABOUT this FREQUENTLY asked COURSE… QUESTIONS… Q: Who can earn FREE CE credits? . READ the MATERIALS. Read and review the course materials. A: EVERYONE - All dental professionals in your office may earn free CE contact . COMPLETE the TEST. Answer the credits. Each person must read the eight question test. A total of 6/8 course materials and submit an questions must be answered correctly online answer form independently. for credit. us . SUBMIT the ANSWER FORM Q: What if I did not receive a ONLINE. You MUST submit your confirmation ID? answers ONLINE at: A: Once you have fully completed your p h o n e http://dent.osu.edu/sterilization/ce answer form and click “submit” you will be directed to a page with a . RECORD or PRINT THE 614-292-6737 unique confirmation ID. CONFIRMATION ID This unique ID is displayed upon successful submission Q: Where can I find my SMS number? of your answer form. -

Back to Basics: Understanding Hidradenitis Suppurativa
PRACTICE DEVELOPMENT Back to basics: understanding hidradenitis suppurativa KEY WORDS Hidradenitis Suppurativa (HS) is a chronic recurrent debilitating skin disease of the Dermatology hair follicle. It is a condition that has been overlooked in wound care publications, Fistulae with most articles found in dermatological journals. However, the condition affects Hidradenitis Suppurativa 1% of the population in Europe and produces painful nodules in one or more of Scarring Sinus tracts the apocrine-gland bearing aspects of the skin that can ulcerate and produce pain and a foul odour and can multiply and eventually develop sinus tracts and fistulae. HS is often misdiagnosed as alternative skin ulcerating conditions, leaving the individuals with many years of suffering from the physical symptoms and their psychological consequences. The disease often begins in puberty and burns out by middle age, leaving the individual with unsightly scarring. This article examines the pathophysiology, clinical presentations and comorbidities associated with the disease. The treatment options focus on controlling the comorbidities, moderating life-style behaviours and arresting the disease. The medical and surgical options are discussed along with their limitations. idrarenitis Suppurativa (HS) was first selection bias, however is thought to be 1% in described by the French surgeon Velpeau Europe (Gulliver et al, 2016; WUWHS, 2016). in 1839. The origin of the term HS comes Prevalence is rare in children and when HS does Hfrom the Greek hidros meaning sweat and aden occur in this population it is often associated with denoting glands (Ather et al, 2006). Initially it was hormonal disorders such as metabolic syndrome, thought to be due to infection of the sweat glands precocious puberty, adrenal hyperplasia and however it is now recognized as an acneform premature adrenarche (Vivar and Kruse, 2017). -
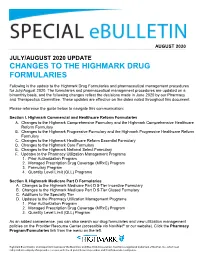
Changes to the Highmark Drug Formularies
AUGUST 2020 JULY/AUGUST 2020 UPDATE CHANGES TO THE HIGHMARK DRUG FORMULARIES Following is the update to the Highmark Drug Formularies and pharmaceutical management procedures for July/August 2020. The formularies and pharmaceutical management procedures are updated on a bimonthly basis, and the following changes reflect the decisions made in June 2020 by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. Please reference the guide below to navigate this communication: Section I. Highmark Commercial and Healthcare Reform Formularies A. Changes to the Highmark Comprehensive Formulary and the Highmark Comprehensive Healthcare Reform Formulary B. Changes to the Highmark Progressive Formulary and the Highmark Progressive Healthcare Reform Formulary C. Changes to the Highmark Healthcare Reform Essential Formulary D. Changes to the Highmark Core Formulary E. Changes to the Highmark National Select Formulary F. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Formulary Program 4. Quantity Level Limit (QLL) Programs Section II. Highmark Medicare Part D Formularies A. Changes to the Highmark Medicare Part D 5-Tier Incentive Formulary B. Changes to the Highmark Medicare Part D 5-Tier Closed Formulary C. Additions to the Specialty Tier D. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Quantity Level Limit (QLL) Program As an added convenience, you can also search our drug formularies and view utilization management policies on the Provider Resource Center (accessible via NaviNet® or our website). Click the Pharmacy Program/Formularies link from the menu on the left. -

Foot Pain in Scleroderma
Foot Pain in Scleroderma Dr Begonya Alcacer-Pitarch LMBRU Postdoctoral Research Fellow 20th Anniversary Scleroderma Family Day 16th May 2015 Leeds Institute of Rheumatic and Musculoskeletal Medicine Presentation Content n Introduction n Different types of foot pain n Factors contributing to foot pain n Impact of foot pain on Quality of Life (QoL) Leeds Institute of Rheumatic and Musculoskeletal Medicine Scleroderma n Clinical features of scleroderma – Microvascular (small vessel) and macrovascular (large vessel) damage – Fibrosis of the skin and internal organs – Dysfunction of the immune system n Unknown aetiology n Female to male ratio 4.6 : 1 n The prevalence of SSc in the UK is 8.21 per 100 000 Leeds Institute of Rheumatic and Musculoskeletal Medicine Foot Involvement in SSc n Clinically 90% of SSc patients have foot involvement n It typically has a later involvement than hands n Foot involvement is less frequent than hand involvement, but is potentially disabling Leeds Institute of Rheumatic and Musculoskeletal Medicine Different Types of Foot Pain Leeds Institute of Rheumatic and Musculoskeletal Medicine Ischaemic Pain (vascular) Microvascular disease (small vessel) n Intermittent pain – Raynaud’s (spasm) • Cold • Throb • Numb • Tingle • Pain n Constant pain – Vessel center narrows • Distal pain (toes) • Gradually increasing pain • Intolerable pain when necrosis is present Leeds Institute of Rheumatic and Musculoskeletal Medicine Ischaemic Pain (vascular) Macrovascular disease (large vessels) n Intermittent and constant pain – Peripheral Arterial Disease • Intermittent claudication – Muscle pain (ache, cramp) during walking • Aching or burning pain • Night and rest pain • Cramps Leeds Institute of Rheumatic and Musculoskeletal Medicine Ulcer Pain n Ulcer development – Constant pain n Infected ulcer – Unexpected/ excess pain or tenderness Leeds Institute of Rheumatic and Musculoskeletal Medicine Neuropathic Pain n Nerve damage is not always obvious.