2014 HHC Report to the Community
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IMG-Friendly Hospitals” in the United States of America
List of “IMG-friendly hospitals” in the United States of America. The authors do not guarantee complete accuracy as this is a moving target. The list serves the purpose of giving you an idea of the programs that have historically been IMG- friendly. As outlined in the book “The International Medical Graduate’s Best Hope”, the authors do not advocate complete reliance on lists but rather encourage a one-on-one search of residency programs according to individual characteristics. STATE PROGRAM H-1B J1 GC ALABAMA Carraway Methodist Medical Center NO NO YES University of Alabama Medical Center ? ? YES Population: Time Zone: Weather: Cost of living: STATE PROGRAM H-1B J1 GC ARKANSAS University of Arkansas for Medical Sciences YES YES YES Population: Time Zone: Weather: Cost of living: STATE PROGRAM H-1B J1 GC ARIZONA Maricopa Medical Center NO NO YES Mayo Clinic Scottsdale NO YES YES University of Arizona & Affiliated Hospitals NO YES YES Population Time Zone Weather Cost of living STATE PROGRAM H-1B J1 GC CALIFORNIA Alameda County Medical Ctr/Highland NO NO YES Hospital Cedars-Sinai Medical Center NO YES YES Kaiser Permanente Med. Ctr., San Francisco NO NO YES Kaiser Permanente Med. Ctr., Santa Clara NO NO YES Kaiser Permanente Medical Center, Oakland NO YES YES Stanford University NO YES YES University of California at Los Angeles Med. NO YES YES Ctr. University of California at Los Angeles Med. NO YES YES Ctr. University of California at San Diego NO YES YES University of Southern California NO YES YES Population Time Zone Weather Cost of living STATE PROGRAM H-1B J1 GC COLORADO Exempla St. -

New York City Health and Hospitals Corporation New York City Health and Hospitals Corporation
NEW YORK CITY HEALTH AND HOSPITALS CORPORATION NEW YORK CITY HEALTH AND HOSPITALS CORPORATION Bronx Kings County Hospital Center Metropolitan Hospital Center Jacobi Medical Center 451 Clarkson Avenue 1901 First Avenue 1400 Pelham Parkway South Brooklyn, New York 11203 New York, New York 10029 Bronx, New York 10461 718-245-3131 212-423-6262 212-918-5000 Woodhull Medical and Mental Renaissance Health Care Lincoln Medical and Mental Health Center Network Diagnostic Health Center 760 Broadway & Treatment Center 234 East 149th Street Brooklyn, New York 11206 215 West 125th Street Bronx, New York 10451 718-963-8000 New York, New York 10027 718-579-5000 212-932-6500 Manhattan Morrisania Diagnostic Bellevue Hospital Center Queens & Treatment Center 462 First Avenue Elmhurst Hospital Center 1228 Gerard Avenue New York, New York 10016 79-01 Broadway Bronx, New York 10452 212-562-4141 Elmhurst, New York 11373 718-960-2777 Coler Goldwater Specialty 718-334-4000 North Central Bronx Hospital Hospital Queens Hospital Center 3424 Kossuth Avenue Roosevelt Island 82-70 164th Street Bronx, New York 10467 New York, New York 10044 Jamaica, New York 11432 718-519-5000 212-848-6000 718-883-3000 Segundo Ruiz Belvis Diagnostic Gouverneur Healthcare Services & Treatment Center 227 Madison Street Staten Island 545 East 142nd Street New York, New York 10002 Sea View Hospital Bronx, New York 10454 212-238-7000 Rehabilitation Center & Home 718-579-4000 460 Brielle Avenue Harlem Hospital Center Staten Island, New York 10314 506 Lenox Avenue Brooklyn 718-317-3000 New York, New York 10037 Coney Island Hospital 212-939-1000 2601 Ocean Parkway Brooklyn, New York 11235 718-616-30000 Cumberland Diagnostic & Treatment Center 100 North Portland Avenue Brooklyn, New York 11205 718-260-7500 Dr. -
NYU Hospitals Center Request for Expansion of Existing Ambulance Service
NYU Hospitals Center Request for Expansion of Existing Ambulance Service PREPARED FOR: New York State Department of Health The Regional EMS Council of New York City PREPARED BY: NYU Hospitals Center Emergency Medical Services March 7th, 2016 Table of Contents Application Part I (Narrative) Introduction Section 1 - Selwices and Staffing - Existent and Proposed Section 2 - Population Demographics Section 3 - Description of Calls Section 4 - Response Times Section 5- Quality of Service Section 6 - Mutual Aid Section 7 - Member Qualifications and Sldli Retention Section 8 - Communications Section 9 - Fiscal Stability Section 10 - Organization and Administration Section 11 - Cost-Benefit Ratio Section 12 - Community and Government Support Section 13 - Reallocation of Existing Resources Section 14- Statement from Service Medical Director & ALS Level of Service Documentation Attachments Application Part II (State Forms and Competency and Fitness) Section 1 - Application for Expansion of EMS Selwice (DOH-BEMS 3777) Section 2 - Affirmation of Competency and Fitness (DOH-BEMS 3778) Section 3 - Resumes for Individuals Providing Affirmations of Competency and Fitness Application Part III (Letters of Endorsement) Section 1 - Sample Letter of Endorsement Section 2 - List of Individuals/Agencies to which Sample Letter of Endorsement was sent Section 3 - Letters of Endorsement Section 4 - Mail Receipts Application Part I (Narrative) Introduction NYU Hospitals Center ("NYUHC") is seeking to permanently expand its current operating territory of southwest Brooklyn (New York City 68 and 72 Police Precincts) to all of Brooklyn and Manhattan (the "Proposed Service Area"). Temporary expansion [for all five boroughs] was approved on March 4th, 2016 by the NYS Department of Health (see Attachment A). -

Network Review | SUMMER/FALL 2008 Edition SUMMER/FALL 2008 Edition | Network Review
NNetworketwork ReviewReview Building for Success SUMMER/FALL 2008 Edition Harlem Hospital Center Lincoln Medical and Mental Health Center Metropolitan Hospital Center Morrisania Neighborhood Family Health Center Renaissance Health Care Network Segundo Ruiz Belvis Neighborhood Family Health Center 4BSBI+POFT "OJUB4POJ .% -JODPMO)PTQJUBM.FEJDBM%JSFDUPS3JDIBSE,4UPOF .% .FUSPQPMJUBO)PTQJUBM.FEJDBM%JSFDUPS.FSZM 8FJOCFSH .FUSPQPMJUBO)PTQJUBM&YFDVUJWF%JSFDUPS'SPOUSPX%S"ZNBO&M.PIBOEFT LFZOPUFTQFBLFS4S7JDF Sarah Jones’ performance brought the 1SFTJEFOU +PTn34gODIF[ ))$1SFTJEFOU"MBO%"WJMFTBOE$IBSMZOO(PJOT $IBJSQFSTPO ))$#PBSEPG%JSFDUPST audience to a standing ovation. 5)"//6"-63#"/ )&"-5)$0/'&3&/$& 4)08$"4&%.0%&-40'*/5&37&/5*0/ continues on pg. 11 453"5&(*&4"/%#&4513"$5*$&4 1BSUOFSTIJQT As racial and ethnic disparities in workshops with participants from New CAB/Auxiliary Network Annual Dinner healthcare outcomes continue to make York, Texas and California and focused headlines both locally and nationally, on specific health disciplines that have the 7th Annual Conference on Urban garnered measurable successes in Health brought together healthcare treatment modalities. professionals and other stakeholders to share innovative strategies aimed The clinical expertise of our Network at eliminating such inequalities in hospitals and Neighborhood Family health. The forum, held on June 12th Health Centers was prominently and 13th at the Helmsley Park Lane showcased during the workshops. continues on pg. 12 Hotel in Manhattan, featured clinical continues on pg. 11 Network Review | SUMMER/FALL 2008 Edition SUMMER/FALL 2008 Edition | Network Review &NCSBDJOH$IBOHF Welcome to the 2008 Summer/Fall Please join me in wishing Metropolitan of 15,000 square feet including 37 exam Edition of our Network Newsletter. This the best in their future endeavors. -

Careconnect Facilities
CareConnect Facilities Manhattan Hospitals Yale-New Haven Northern Harlem Westchester Bridgeport Metropolitan Lenox Hill Manhattan Eye, Ear & Throat Phelps Memorial Lenox Health Greenwich Greenwich Montefiore White Plains Village Medical Bellevue Centers Peconic Bay Medical Center North Central Bronx Jacobi Huntington Glen Cove Lincoln Syosset North Shore University Zucker Hillside Plainview Elmhurst LIJ Medical Center Cohen Children’s LIJ Forest Nassau University Hills Queens Medical Center Southside Woodhull Wyckoff Heights South Oaks Kings County LIJ Valley Stream Staten Island Maimonides University (North) Coney Island Staten Island University (South) For a searchable list of CareConnect’s providers, visit CareConnect.com/providersearch Hospitals • Bellevue Hospital Center, 462 First Avenue, New York, NY 10016, P: 212-562-4141 • Bridgeport Hospital, 267 Grant St, Bridgeport, CT 06610, P: 203-688-8412 • Coney Island Hospital, 2601 Ocean Parkway, Brooklyn, NY 11235, P: 718 616-3000 • Elmhurst Hospital Center, 79-01 Broadway, Elmhurst, NY, 11373, P: 718-334-4000 • Glen Cove Hospital, 101 St. Andrews Lane, Glen Cove, NY 11542, P: 516-674-7540 • Greenwich Hospital, 5 Perryridge Road, Greenwich, CT 06 830, P: 203-688-8412 • Harlem Hospital Center, 506 Lenox Avenue, New York, NY 10037, P: 212-939-1000 • Huntington Hospital, 270 Park Avenue, Huntington, NY 11743, P: 631-351-2000 • Jacobi Medical Center, 1400 Pelham Parkway South, Bronx, NY 10461, P: 718-918-5000 • Kings County Hospital Center, 451 Clarkson Avenue, Brooklyn, NY 11203, P: 718-245-3131 -

Rheumatology
NYU Langone Medical Center 550 First Avenue, New York, NY 10016 nyulmc.org RHEUMATOLOGY 2014 YEAR IN REVIEW CONTENTS 1 Letter from the Chairs 2 Facts & Figures 1 Message from the Director 4 New & Noteworthy 2 Facts & Figures 6 Section 4 New & Noteworthy 42 Research 10 Clinical Care and Research 44 Education 11 Lupus and Neonatal Lupus 13 Behçet’s Syndrome 48 Publications 14 Rheumatology and Osteoporosis 5164 LoPsoriaticcations Arthritis 18 Rheumatoid Arthritis and Osteoarthritis 55 Leadership 20 Education & Training 56 NYU Langone Medical Center Facts & Figures 24 Professional Activities 57 NYU Langone Medical Center Leadership Design: Ideas On Purpose, www.ideasonpurpose.com 27 Leadership, Locations Produced by: Office of Communications and Marketing, NYU Langone Medical Center NYU LANGONE MEDICAL CENTER / RHEUMATOLOGY / 2014 PAGE 1 MESSAGE FROM THE DIRECTOR Dear Colleagues and Friends, The tripartite mission of our division is clear: Deliver comprehensive state-of-the-art clinical care, translate and integrate medicine and science, and increase the knowledge base of our trainees. I’m proud to report that in 2014, with the dedication of all faculty members, we have made significant strides in all three areas, as evidenced in the following pages. Under the guidance of our previous division director, Steven B. Abramson, MD, now chair of the Department of Medicine, the Judith and Stewart Colton Center for Autoimmunity was established. The center aims to advance discoveries about the microbiome and its relationship to autoimmune disease, and to leverage this new knowledge to develop strategies for prevention and JILL P. BUYON, MD treatment. Our vision of a comprehensive, multidisciplinary Psoriatic Arthritis Center dedicated to the bench-to-bedside integration of dermatology and Director, Division of Rheumatology, rheumatology has now been realized, and a strong laboratory research base will Department of Medicine stand behind this center to further our understanding of psoriatic arthritis and NYU Langone Medical Center develop novel therapies. -
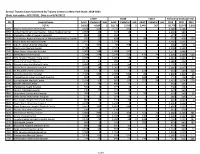
Annual Trauma Cases Submitted by Trauma Centers in New York State
Annual Trauma Cases Submitted by Trauma Centers in New York State: 2018-2021 (Date last update: 8/17/2021, Data as of 8/3/2021) Y2019 Y2020 Y2021 TOTALS by Discharge Year PFI Hospital Name Adult Pediatric Unk Adult Pediatric Unk Adult Pediatric Unk 2019 2020 2021 TOTAL 54,562 4,209 1 50,176 3,793 3 5,443 367 - 58,772 53,972 5,810 0001 Albany Medical Center Hospital 3,168 320 . 3,772 392 . 3,488 4,164 - 0058 United Health Services Hospital - Wilson Medical Center 1,067 23 . 934 13 . 1,090 947 - 0135 Champlain Valley Physicians Hospital 465 12 . 314 2 . 477 316 - 0180 Mid Hudson Regional Hospital of Westchester Medical Center 745 22 . 428 . 98 2 767 428 100 0181 Vassar Brothers Medical Center 1,141 15 . 1,029 2 . 1,156 1,031 - 0208 John R. Oishei Children's Hospital 64 335 . 68 258 2 4 399 326 6 0210 Erie County Medical Center 2,598 1 . 2,525 . 2,599 2,525 - 0245 Stony Brook University Hospital 2,003 168 . 1,686 162 . 2,171 1,848 - 0413 Strong Memorial Hospital 2,244 254 . 2,246 223 470 74 2,498 2,469 544 0511 NYU Langone Hospital-Long Island 1,288 77 . 1,305 56 26 8 1,365 1,361 34 0527 Mount Sinai South Nassau 1,171 17 . 989 4 . 1,188 993 - 0528 Nassau University Medical Center 1,384 34 . 1,187 25 . 1,418 1,212 - 0541 North Shore University Hospital 2,150 16 . 1,907 10 . -
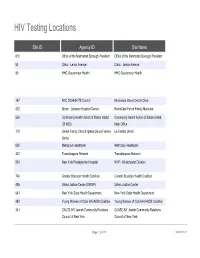
HIV Testing Locations
HIV Testing Locations Site ID Agency ID Site Name 810 Office of the Manhattan Borough President Office of the Manhattan Borough President 53 Clinic - Lenox Avenue Clinic - Lenox Avenue 90 HHC Gouverneur Health HHC Gouverneur Health 167 NYC DOHMH TB Control Morrisania Chest Center Clinic 822 Bronx - Lebanon Hospital Center BronxCare Fulton Family Medicine 524 Community Health Action of Staten Island Community Health Action of Staten Island- (CHASI) Main Office 119 United Family Church-Iglesia De La Familia La Familia Unida Unida 605 Metroplus Healthplan Metroplus Healthplan 442 Transdiaspora Network Transdiaspora Network 542 New York Presbyterian Hospital NYP - Westchester Division 746 Greater Brooklyn Health Coalition Greater Brooklyn Health Coalition 495 Urban Justice Center (SWOP) Urban Justice Center 641 New York State Health Department New York State Health Department 452 Young Women of Color HIV/AIDS Coalition Young Women of Color HIV/AIDS Coalition 341 CAUSE-NY Jewish Community Relations CAUSE-NY Jewish Community Relations Council of New York Council of New York Page 1 of 533 09/30/2021 HIV Testing Locations Hours Monday Hours Tuesday 11:00 AM - 7:00 PM 9:00 AM - 5:00 PM 8:00 AM - 8:00 PM 8:00 AM - 8:00 PM CLOSED CLOSED 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM Page 2 of 533 09/30/2021 HIV Testing Locations Hours Wednesday Hours Thursday 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM 8:30 AM - 5:00 PM 8:00 AM - 8:00 PM 8:30 AM - 5:00 PM 8:30 AM - 5:00 PM 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM Page 3 of 533 09/30/2021 HIV Testing Locations Hours Friday -
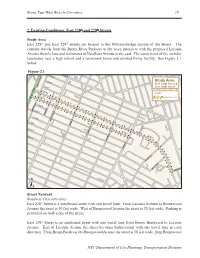
Bronx East-West Bicycle Corridors: Existing Conditions: East 228Th And
Bronx East-West Bicycle Corridors 19 2. Existing Conditions: East 228th and 229th Streets Study Area East 228th and East 229th streets are located in the Williamsbridge section of the Bronx. The corridor travels from the Bronx River Parkway at the west, intersects with the proposed Laconia Avenue bicycle lane and terminates at Needham Avenue to the east. The eastern end of the corridor terminates near a high school and a retirement home and assisted living facility. See Figure 2.1 below. Figure 2.1 E. 232 ST E. 233 ST E. 231 ST Study Area East 228th Street & E. 230 ST BRONX BOULEVARD East 229th Street E. 229 ST LEGEND E. 228 ST Study Corridors E. 227 ST E. 226 ST CARPENTER AV LOWERRE PL E. 225ST WHITE PLAINS RD E. 224 ST BARNES AV E. 223 ST E. 229 RD E. 228 ST BRONXWOOD AV E. 229 ST E. 222 ST PAULDING AV LACONIA AV SCHIEFFELIN AV SCHIEFFELIN PL NEEDHAM AV ± Street Network Roadway Characteristics East 228th Street is a westbound street with one travel lane. From Laconia Avenue to Bronxwood Avenue the street is 30 feet wide. West of Bronxwood Avenue the street is 25 feet wide. Parking is permitted on both sides of the street. East 229th Street is an eastbound street with one travel lane from Bronx Boulevard to Laconia Avenue. East of Laconia Avenue the street becomes bidirectional with one travel lane in each direction. From Bronx Boulevard to Bronxwood Avenue the street is 30 feet wide, from Bronxwood NYC Department of City Planning, Transportation Division 20 Bronx East-West Bicycle Corridors Avenue to Laconia Avenue the street is 33 feet wide, and from Laconia Avenue to Needham Avenue the street is 50 feet wide. -

August 9, 2021 RELIEF RESOURCES and SUPPORTIVE
September 24, 2021 RELIEF RESOURCES AND SUPPORTIVE INFORMATION1 • Health & Wellness • Housing • Workplace Support • Human Rights • Education • Bilingual and Culturally Competent Material • Beware of Scams • Volunteering • Utilities • Legal Assistance • City and State Services • Burial • Transportation • New York Forward/Reopening Guidance • Events HEALTH & WELLNESS • Financial Assistance and Coaching o COVID-19 Recovery Center : The City Comptroller has launched an online, multilingual, comprehensive guide to help New Yorkers navigate the many federal, state and city relief programs that you may qualify for. Whether you’re a tenant, homeowner, parent, small business owner, or excluded worker, this online guide offers information about a range of services and financial support. o New York City will be extending free tax assistance to help families claim their new federal child tax credit. As an investment in the long-term recovery from the pandemic, the federal American Rescue Plan made changes to the Child Tax Credit so families get half of the fully refundable credit—worth up to $3,600 per child—as monthly payments in 2021 and the other half as a part of their refund in 1 Compiled from multiple public sources 2022. Most families will automatically receive the advance payments, but 250,000+ New York City families with more than 400,000 children need to sign up with the IRS to receive the Credit. The Advance Child Tax Credits payments began on July 15, 2021 and most New Yorkers will receive their payments automatically. However, New Yorkers who have not submitted information to the IRS need to either file their taxes or enter their information with the IRS’ Child Tax Credit Non-Filer Sign-Up Tool For more information about the Advance Child Tax Credit including access to Multilingual flyer and poster—and NYC Free Tax Prep, visit nyc.gov/TaxPrep or call 311. -

HAVAA Invitation
RD AWA XILIAN AN EMENT L AU D VOLUNTEER ACHIEV ITA SP HO D AR AW T EN EM V IE H C A R E E T N U The United Hospital Fund is dedicated to creating the health care system all of us want for ourselves, our families, and our neighbors. Please consider honoring one of today’s extraordinary volunteers or auxilians, and supporting the work of the Fund, by becoming a Patron or Sponsor. This unique awards program brings public attention to the invaluable contributions of our honorees, and the other 50,000 committed volunteers in our city, who make such an important difference to patients and their families and extend the ability of New York’s hospitals to provide the best care possible. Patrons and Sponsors will be recognized in the event’s Program and all gifts will be gratefully acknowledged. Please use the enclosed reply card to indicate your level of support. Please join us for tea at the Waldorf as the United Hospital Fund honors the 2009 recipients of the # HOSPITAL AUXILIAN and VOLUNTEER ACHIEVE#MENT AWARD Friday, March 6, 2009 1:00 p.m. to 3:00 p.m The Grand Ballroom of The Waldorf-Astoria Park Avenue at 50th Street, New York City Special Guest Sade Baderinwa Co-anchor,WABC-TV Eyewitness News at 5:00 RSVP by February 10, 2009 on the enclosed card Generously underwritten by TD Bank United Hospital Fund The United Hospital Fund is a health services research and J. Barclay Collins II philanthropic organization whose Chairman mission is to shape positive change James R. -

Edition of the Norwood News
Proudly Serving Bronx Communities Since 1988 3URXGO\6HUYLQJ%URQ[&RPPXQLWLHV6LQFHFREE 3URXGO\6HUYLQJ%URQ[&RPPXQLWLHV6LQFHFREE 0UQ\YLK*VUZ[Y\J[PVU>VYRLYZ - 5.875” wideORWOOD by 7.0568”Q high EWSQ 3/4 Page NVol. 27, No. 8 PUBLISHED BY MOSHOLU PRESERVATION CORPORATION N April 17–30, 2014 ORWOODQ EWSQ Vol 33, No 3 • PUBLISHED BY MOSHOLU PRESERVATION CORPORATION • JANUARY 30-FEBRUARY 12, 2020 NVol. 27, No. 8 PUBLISHED BY MOSHOLU PRESERVATION CORPORATION N April 17–30, 2014 FREE HSSV[OLY(JJPKLU[=PJ[PTZ We Fight for the Money You Deserve COHEN:Regardless EXPAND of Your Immigration RIGHT Status *VUZ[Y\J[PVU >VYRWSHJL(JJPKLU[Z*HY ;Y\JR(JJPKLU[Z ,SL]H[VY,ZJHSH[VY(JJPKLU[Z5LNSPNLU[)\PSKPUN:LJ\YP[`:SPW;YPW -HSSZ More rentersTO facing4LKPJHS4HSWYHJ[PJL5\YZPUN/VTL5LNSPNLUJL COUNSELeviction could be given representation LAW in Housing Court 7VSPJL)Y\[HSP[`*P]PS9PNO[Z=PVSH[PVUZ Our GUARANTEEBP Diaz Jr. Bows Out Of Mayor’s Race 1/2 Page - 5.875” wide by 4.6875”7KHUHLV1 high O FEE 8QOHVV:H:LQ1/4 Pagepg 2 - Vertical 2XU¿UPKDVUHFRYHUHGRYHU2.8542” wide by 4.6875” high One Hundred Million Dollars LQYHUGLFWVDQGVHWWOHPHQWV IRURXUVDWLV¿HGFOLHQWVNYPD Releases 52nd Precinct-Involved FREE CONSULTATIONShooting Video | pg 6 &DOO+RXUVD'D\'D\VD:HHN Photo by José A. Giralt COUNCILMAN ANDREW COHEN (pictured) speaks Recentat a town hall meetingRecoveries organized by the for Community Clients Action for Safe Apartments (CASA), NorthwestConstruction Bronx Clergy and Coalition Accident (NWBCCC), and Right to Counsel (RTCNYC) in theTruck Mt. Eden sectionAccident of the Bronx on Jan. 15. The event seeks to build support for bills Intro 1529 and Intro 1104 which expand the rights of tenants to receive free legal representation in eviction proceedings.Police Misconduct Elevator Accident 1/8 Page 1/4 ByPage JOSÉ A.