22Nd European Conference on General Thoracic Surgery ABSTRACTS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Instrument Catalogue
Company Profile Dixons Surgical Instruments Ltd is a leading UK manufacturer of Surgical and Orthopaedic Instruments. We specialise in the manufacture of Precision Medical Devices and can offer a full service from Design, through Prototyping and on to Full Production Runs. The company was founded in November 1948 by Frank Dixon in Caledonian Road, London before moving to Leigh-On-Sea, Essex in 1956. Frank's son, John Dixon, joined the company in 1960 and trained in all aspects of the business. On the death of his Father in 1979, John took over as Managing Director. He was joined shortly after by his wife, Joan Dixon, who became the Financial Director. The company steadily expanded over the years and in 1989 it moved from the site in Leigh-On-Sea to a purpose built factory in Wickford, Essex, approximately 30 miles (50 Km) east of London. John and Joan's son, Jay Dixon, joined the company in 1990 and carried out a 5 year apprenticeship as a Surgical Instrument Maker. He then followed in his Father’s footsteps by training in all other aspects of the business, becoming Technical Director in 2004. In 2010 Jay Dixon was appointed Managing Director, while John Dixon moved into the role of Chairman. Joan Dixon continues to be the Financial Director. Today our Surgical and Orthopaedic Instruments are manufactured at our Wickford factory using a combination of the latest CNC controlled machines, along with the manual skills of our experienced craftsmen. This approach enables us to make Surgical and Orthopaedic Instruments in the most accurate and efficient way possible whilst still retaining that finishing touch required for truly excellent instruments. -

Hybrid Video-Assisted Thoracoscopic Surgery Sleeve Lobectomy for Non-Small Cell Lung Cancer: a Case Report
6846 iMDT Corner Hybrid video-assisted thoracoscopic surgery sleeve lobectomy for non-small cell lung cancer: a case report Chenlei Zhang1, Zhanwu Yu1, Jijia Li1, Peng Zu1, Pingwen Yu1, Gebang Wang1, Takuro Miyazaki2, Ryuichi Waseda3, Raul Caso4, Giulio Maurizi5, Hongxu Liu1 1Department of Thoracic Surgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital & Institute, Shenyang, China; 2Department of Surgical Oncology, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan; 3Department of General Thoracic, Breast, and Pediatric Surgery, Fukuoka University, Fukuoka, Japan; 4Department of Surgery, MedStar Georgetown University Hospital, Washington, DC, USA; 5Department of Thoracic Surgery, Sant’Andrea Hospital, Sapienza University of Rome, Rome, Italy Correspondence to: Hongxu Liu. Department of Thoracic Surgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital & Institute, No.44 Xiaoheyan Road, Dadong District, Shenyang 110042, China. Email: [email protected]. Submitted Feb 04, 2020. Accepted for publication Oct 24, 2020. doi: 10.21037/jtd-20-2679 View this article at: http://dx.doi.org/10.21037/jtd-20-2679 Introduction procedure. Also, hybrid VATS SL is a safer approach, especially in patients with infiltration of the pulmonary Lung cancer continues to be the leading cause of cancer- artery (PA), as it makes the surgeon more comfortable related death in China and worldwide (1,2). Sleeve during the bronchial and arterial anastomoses. Literatures lobectomy (SL) and pneumonectomy are surgical options for have shown that hybrid VATS approach has advantages for the treatment of locally advanced non-small cell lung cancer select T3 chest wall lung cancers (13) and superior sulcus (NSCLC). SL was initially intended as a parenchyma- tumors (14) over conventional open surgery. -

Medicure Instruments
MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-503 MI-502 MI-501 KOCHER’S MOSQUITO FORCEPS FORCEPS SPENCER WELLS ARTERY FORCEPS STAINLESS STEEL STRAIGHT ARTERY MI-504 MI-505 MI-506 MI-507 MI-508 KOCHER’S DISSECTING FORCEPS DISSECTING FORCEPS RUSSIAN DISSECTING FINE DISSECTING FORCEPS STAINLESS STEEL - PLAIN STAINLESS STEEL - TOOTH FORCEPS FORCEPS - PLAIN CURVED ARTERY MI-509 MI-510 MI-511 TOWEL CLIP FINE DISSECTING DENNIS BROWNE TOWEL FORCEPS CROSS-ACTION FORCEPS - TOOTH DISSECTING FORCEPS BACKHAUS GENERAL SURGERY INSTRUMENTS MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-512 MI-513 MI-513 MI-514 LISTER SINUS B.P. HANDLE NO. 3 B.P. HANDLE NO. 4 B.P. HANDLE NO. 7 MALLEBLE PROBE DRESSING FORCEPS WITH EYE MI-515 MI-5164 MI-514 BOZEMANN KILNER MI-517 MAYO HEGARS NEEDLE HOLDERS NEEDLE HOLDERS FINE DRESSING SCISSORS NEEDLE HOLDERS STRAIGHT STRAIGHT STRAIGHT (SHARP x BLUNT) STRAIGHT STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL MI-521 MI-518 MI-519 MI-520 STITCH RIBBON SCISSORS DRESSING SCISSORS IRIS SCISSORS KNAPP SCISSORS STRAIGHT STRAIGHT (SHARP x SHARP) STRAIGHT STRAIGHT STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL GENERAL SURGERY INSTRUMENTS MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-523 MI-524 MI-525 STEVENS SCISSORS MAYO SCISSORS GREEN BERG SCISSORS MI-522 STRAIGHT STRAIGHT (KILNER) METZENBAUM SCISSORS STAINLESS STEEL STRAIGHT STAINLESS STEEL STRAIGHT STAINLESS STEEL STAINLESS STEEL MI-528 MI-529 ALLIS TISSUE POTT’S ANGLED GRASPING FORCEPS MI-526 -

STILLE Surgical Instruments Kirurgisk Perfektion I Närmare 180 År Surgical Perfection for Almost 180 Years
STILLE Surgical Instruments Kirurgisk perfektion i närmare 180 år Surgical Perfection for almost 180 years I närmare 180 år har vi utvecklat och tillverkat de bästa kirurgiska For almost 180 years, we have developed and manufactured the best instrumenten till världens mest krävande kirurger. Vi vill rikta ett stort surgical instruments for the world’s most demanding surgeons. tack till alla våra trogna kunder och samtidigt välkomna våra nya kunder. We would like to extend a heartfelt thank you to all our loyal I den här katalogen presenterar vi vårt kompletta sortiment av customers and a warm welcome to our new customers. In this catalog STILLEs original instrument. we present our complete range of STILLE original surgical instruments. Precision, hållbarhet och känsla är typiska egenskaper för alla Precision, durability and feel are characteristic qualities of all STILLE STILLE-instrument. Den stora majoriteten är handgjorda av våra instruments. The vast majority are handcrafted by our highly skilled skickliga instrumentmakare Eskilstuna. Instrumentets resa från rundstål instrument makers in Eskilstuna, west of Stockholm, Sweden. The instru- till ett färdigt instrument är lång, och består av många tillverkningssteg. ments’ journey from a rod of stainless steel to a finished instrument is a STILLEs unika tillverkningsmetod och användning av enbart det bästa long one, involving multiple stages. STILLE’s unique method of crafting its materialet ger våra instrument deras unika känsla och hållbarhet. instrument materials, and its usage of only the very highest-grade steels, give our instruments their unique feel and durability. I det första kapitlet hittar du våra saxar, allt från vanliga operationssaxar till våra unika SuperCut och Diamond SuperCut-saxar. -
Preliminary Programme VERSION 3 MAY 2017
PRELIMINARY PROGRAMME VERSION 3 MAY 2017 You can register online now CLICK HERE OPPortUNITIES AND CHALLENGES ANNUAL SCIENTIFIC MEETING 28 – 30 June 2017 ICC BIRMINGHAM PLATINUM SPONSOR British Association of Oral and Maxillofacial Surgeons The Royal College Surgeons, 35-43 Lincoln’s Inn Fields, London WC2A 3PE Email: [email protected] Website: www.baoms.org.uk Plan ahead Contact us at: [email protected] +44 1635 262 400 BAOMS Flyer.1.indd 3 3/21/17 2:33 PM BIRMINGHAM 2017 PRELIMINARY PROGRAMME 3 CONTINUING ProFESSIONAL DEVELOPMENT (CPD) CONTENTS This scientific meeting aims to provide attendees with the opportunity to gain up to date knowledge on the latest developments in research, audit, education, surgical techniques, INtroDUCTION clinical patient management and outcomes in the field of oral and maxillofacial surgery. from ThE BAOMS PRESIDEnT This is delivered through seminars led by experts in their field, masterclasses and short papers presenting the latest research and developments. Participants should verify their own attendance record out of the maximum hours 4 available, which have been calculated as follows: Wednesday 28 June CPD hours 5.25 BAOMS COunCIL 2017 Thursday 29 June CPD hours 6.25 Friday 30 June CPD hours 6.25 4 CERTIFicaTES OF ATTENdaNCE Certificates of attendance indicating the CPD hours for the elements of the meeting ExhIBITIOn PLAn & LISTIngS booked by the attendee will be sent by email after the conference. SIGNING THE ATTENdaNCE REGISTER 5 In order to meet the requirements of verifiable CPD attendees should sign in at the Registration Desk on each day that they attend the conference. -

ANNSURG-D-20-01577 Proofs.Pdf
CE: R.R.; ANNSURG-D-20-01577; Total nos of Pages: 8; ANNSURG-D-20-01577 REVIEW PAPER Electrocautery, Diathermy, and Surgical Energy Devices Are Surgical Teams at Risk During the COVID-19 Pandemic? à à à AQ2 Kimberley Zakka, Simon Erridge, MBBS, BSc, Swathikan Chidambaram, Michael Kynoch,y à à AQ3 James Kinross, and Sanjay Purkayastha Y, on behalf of the PanSurg collaborative group coronavirus disease-19 (COVID-19) pandemic there are understand- Objective: The aim of the study was to provide a rapid synthesis of available able concerns amongst the surgical community as to the risk of viral data to identify the risk posed by utilizing surgical energy devices intra- transmission within such surgical plumes. operatively due to the generation of surgical smoke, an aerosol. Secondarily it To date, live SARS-CoV2 has been detected in lower respira- aims to summarize methods to minimize potential risk to operating room staff. tory tract samples, saliva, feces, bile, and blood specimens.2,3 As Summary Background Data: Continuing operative practice during the such, during the perioperative process, precautions should be con- coronavirus disease-19 (COVID-19) pandemic places the health of operating sidered to minimize potential risk to the clinical team. Similar to the theatre staff at potential risk. SARS-CoV2 is transmitted through inhaled severe acute respiratory syndrome (SARS) and Middle East respira- droplets and aerosol particles, thus posing an inhalation threat even at tory syndrome outbreaks, there is a paucity of data on the potential of considerable distance. Surgical energy devices generate an aerosol of biolog- transmission of the virus intraoperatively. -

EACMFS16 Scientific Programme Monday, September 12, 2016
EACMFS16 Scientific programme Monday, September 12, 2016 TRAINEE DAY: AOCMF LECTURE - ADVANCES IN COMPUTER-ASSISTED MICROVASCULAR CRANIOMAXILLOFACIAL RECONSTRUCTION 08:00 - 10:00 MOUNTBATTEN 08:00 AOCMF LECTURE - ADVANCES IN COMPUTER-ASSISTED MICROVASCULAR CRANIOMAXILLOFACIAL RECONSTRUCTION TRAINEE DAY: HANDS-ON WORKSHOP I: COMPUTER ASSISTED MICROVASCULAR CRANIO MAXILLO-FACIAL 10:00 - 12:00 CAMBRIDGE 10:00 HANDS-ON WORKSHOP I: COMPUTER ASSISTED MICROVASCULAR CRANIO MAXILLO-FACIAL Chair: Majeed Rana (Germany) TRAINEE DAY: HANDS-ON WORKSHOP II: MECTRON PIEZOSURGERY 10:00 - 12:00 WINDSOR 10:00 HANDS-ON WORKSHOP II: MECTRON PIEZOSURGERY Chair: Manlio Galiè (Italy) Break: LUNCH BREAK IN THE CAMBRIDGE HALL 12:00 - 13:00 CAMBRIDGE TRAINEE DAY: JOHN LOWRY TRAINEE STUDY DAY – FROM THEN UNTIL NOW – MILESTONES OF CRANIOMAXILLOFACIAL SURGERY & RECONSTRUCTION 13:00 - 19:30 MOUNTBATTEN 13:00 WELCOME ADDRESS, INTRODUCTION OF FACULTY, COURSE OBJECTIVES 13:00 Manlio Galiè (Italy) 13:00 Majeed Rana (Germany) 13:00 Ian Martin (United Kingdom) 13:00 Ash Gulati () 13:15 ACADEMIC WRITING Jörg Wiltfang (Germany) 13:45 INTRODUCTION TO CRANIOFACIAL SURGERY: BASIC CONCEPTS AND PRINCIPLES Luigi Clauser (Italy) 13:45 INTRODUCTION TO CRANIOFACIAL SURGERY: BASIC CONCEPTS AND PRINCIPLES Manlio Galiè (Italy) 14:15 PRIMARY ORBITAL RECONSTRUCTION Majeed Rana (Germany) 14:45 SECONDARY ORBITAL RECONSTRUCTION Michael Grant (USA) 15:15 ORTHOGNATIC SURGERY AND DISTRACTION OSTEOGENESIS Manlio Galiè (Italy) 15:45 MILESTONE IN 3D VIRTUAL PLANNING OF ORTHOGNATHIC SURGERY Gwen Swennen (Belgium) 16:15 CRANIOMAXILLOFACIAL RECONSTRUCTION IN CONGENITAL AND ACQUIRED DEFORMATIES Nils-Claudius Gellrich (Germany) 16:45 DISCUSSION AND COFFEE BREAK 17:15 EUROPEAN TRAINEE BUSINESS MEETING 17:15 Majeed Rana (Germany) 17:15 M. Billa (Belgium) 17:45 PERSPECTIVES AND CHALLENGES IN RECONSTRUCTION AFTER ABLATIVE SURGERY Moni Abraham Kuriakose (USA) 18:15 RECONSTRUCTION WITH MYOCUTANEOUS MICROVASCULAR FLAPS Klaus D. -

Sansescofet-Dissertation
Copyright by Marta Sans Escofet 2020 The Dissertation Committee for Marta Sans Escofet Certifies that this is the approved version of the following Dissertation: Advancements in Ambient Ionization Mass Spectrometry Towards Improved Ovarian Cancer Research and Diagnosis Committee: Livia Schiavinato Eberlin, Supervisor Jennifer S. Brodbelt Richard M. Crooks Robert Tibshirani Advancements in Ambient Ionization Mass Spectrometry Towards Improved Ovarian Cancer Research and Diagnosis by Marta Sans Escofet Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin May 2020 Dedication To my parents, Ramon and Joana Acknowledgements I am extremely grateful for all the opportunities and support I have received during graduate school. It has been a truly exciting and enlightening experience, and I owe that to everyone who has been with me throughout this journey. First of all, I would like to thank my parents, Ramon and Joana, and my sister Mireia for always being my number one fans. Mom and dad, staying close to you despite being 5,000 miles apart has been a source of strength for me every day. Thank you for always being there during my good and bad moments and for your advice and words of encouragement. Your relationship inspires me, I admire everything you have accomplished together for our family with all your hard work. Thank you for teaching me the importance of enjoying everything you do and to live life at the fullest. Love you and miss you very much. -

Official Proceedings
Scientific Session Awards Abstracts presented at the Society’s annual meeting will be considered for the following awards: • The George Peters Award recognizes the best presentation by a breast fellow. In addition to a plaque, the winner receives $1,000. The winner is selected by the Society’s Publications Committee. The award was established in 2004 by the Society to honor Dr. George N. Peters, who was instrumental in bringing together the Susan G. Komen Breast Cancer Foundation, The American Society of Breast Surgeons, the American Society of Breast Disease, and the Society of Surgical Oncology to develop educational objectives for breast fellowships. The educational objectives were first used to award Komen Interdisciplinary Breast Fellowships. Subsequently the curriculum was used for the breast fellowship credentialing process that has led to the development of a nationwide matching program for breast fellowships. • The Scientific Presentation Award recognizes an outstanding presentation by a resident, fellow, or trainee. The winner of this award is also determined by the Publications Committee. In addition to a plaque, the winner receives $500. • All presenters are eligible for the Scientific Impact Award. The recipient of the award, selected by audience vote, is honored with a plaque. All awards are supported by The American Society of Breast Surgeons Foundation. The American Society of Breast Surgeons 2 2017 Official Proceedings Publications Committee Chair Judy C. Boughey, MD Members Charles Balch, MD Sarah Blair, MD Katherina Zabicki Calvillo, MD Suzanne Brooks Coopey, MD Emilia Diego, MD Jill Dietz, MD Mahmoud El-Tamer, MD Mehra Golshan, MD E. Shelley Hwang, MD Susan Kesmodel, MD Brigid Killelea, MD Michael Koretz, MD Henry Kuerer, MD, PhD Swati A. -
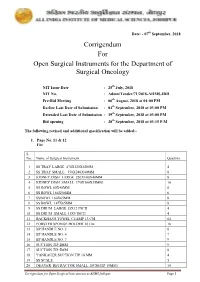
Corrigendum for Open Surgical Instruments for the Department Of
Date: - 07th September, 2018 Corrigendum For Open Surgical Instruments for the Department of Surgical Oncology NIT Issue Date : 25th July, 2018 NIT No. : Admn/Tender/71/2018-AIIMS.JDH Pre-Bid Meeting : 06th August, 2018 at 04:00 PM Earlier Last Date of Submission : 04th September, 2018 at 03:00 PM Extended Last Date of Submission : 19th September, 2018 at 03:00 PM Bid opening : 20th September, 2018 at 03:15 P.M The following revised and additional specification will be added:- 1. Page No. 11 & 12 For S. No. Name of Surgical Instrument Quantity 1 SS TRAY LARGE 470X320X50MM 4 2 SS TRAY SMALL 350X240X40MM 8 3 KIDNEY DISH LARGE 250X140X40MM 8 4 KIDNEY DISH SMALL 170X100X35MM 10 5 SS BOWL 80X40MM 6 6 SS BOWL 166X50MM 6 7 SSBOWL 160X65MM 8 8 SS BOWL 147X65MM 8 9 SS DRUM LARGE 15X12 INCH 4 10 SS DRUM SMALL 11X9 INCH 4 11 BACKHAUS TOWEL CLAMP 13 CM 64 12 FORSTER SPONGE HOLDER 18 Cm 18 13 BP HANDLE NO. 3 8 14 BP HANDLE NO. 4 7 15 BP HANDLE NO. 7 9 16 SUCTION TIP 2MM 9 17 SUCTION TIP 5MM 8 18 YANKAUER SUCTION TIP 10 MM 4 19 SS SCALE 5 20 DEAVER RETRACTOR SMALL 18CM(TIP 19MM) 14 Corrigendum for Open Surgical Instruments at AIIMS Jodhpur Page 1 21 DEAVER RETRACTOR MEDIUM 30.5CM (TIP 25 MM) 10 22 DEAVER RETRACTOR LARGE 31.5CM (TIP 50MM) 10 23 DOYEN’S RETRACTOR 4 24 MORRIS RETRACTOR 25cm ( BLADE 7x4cm) 6 25 SKIN HOOK 32 26 LANGENBECK RETRACTOR SMALL 16cm (TIP 21x 8mm) 16 27 LANGENBECK RETRACTOR MEDIUM 22cm (TIP 50x11mm) 16 28 LANGENBECK RETRACTOR LARGE 22.5cm (TIP 85x15mm) 14 29 C ZERNY RETRACTOR 17.2 cm 14 30 VEIN RETRACTOR 18 31 BALFOUR ABDOMINAL RETRACTOR 20cm 3 32 MASTOID RETRACTOR 4 33 PERIOSTEUM ELEVATOR SHARP 4 34 PERIOSTEUM ELEVATOR BLUNT 4 35 DISSECTING TOOTH FORCEPS 15 CM 16 36 DISSECTING PLAIN FORCEPS 18 CM 16 37 ARTERY FORCEPS CVD 15 CM 36 38 ARTERY FORCEPS ST. -
EG-Konformitätserklärung EC Declaration of Conformity Geister
EG-Konformitätserklärung EC Declaration of Conformity Anbieter: Name: Geister Medizintechnik GmbH Anschrift: Föhrenstrasse 2 Address: 78532 Tuttlingen / Germany Produkte: Chirurgische Instrumente Klasse IIa Producte: Medical devices Class IIa Artikel: Siehe Produktliste im Anhang Article: See Product List in the Annex Wir erklären in alleiniger Verantwortung, dass die oben aufgeführten Medizinprodukte den einschlägigen Bestimmungen der Richtlinie 93/42/EWG entsprechen. We declare on our own responsibility that the medical devices specified above, meets all the provisions of the Directive 93/42/EEC which apply for him. Die Erklärung gilt für alle Produkte des angegebenen Typs bis zum 31.12.2019. This declaration concerns all denoted medical devices until the date 31.12.2019. Angewandtes Konformitätsbewertungsverfahren nach Richtlinie 93/42/EWG: Conformity assessment procedure according Directive 93/42/EEC: Ausgabe/ Dokument-Nr. Titel Ausgabedatum Document No Title Date of issue Richtlinie 93/42/EWG des Rates über Medizinprodukte 93/42/EWG Directive 93/42/EEC for Medical Devices 14.06.1993 93/42/EEC Annex II.3 , Annex V , Annex VII Benannte Stelle / Notified Body: TÜV SÜD Product Service GmbH, Zertifizierstelle, Ridlerstrasse 65, 80339 München / Germany Kennnummer / Reg.-No: 0123 Tuttlingen, 02.01.2015 Carsten Geister, General Manager (Name, Funktion) (Unterschrift) (Name and Function) (Sign) Filename with change level: Created / Changed at: Edited by: Page DoC Cl IIa J_Product List 02.01.15 jw 1 to 24 Item Article designation Class 01-1550 -

Picosecond Infrared Laser Desorption Mass Spectrometry Identifies Medulloblastoma Subgroups on Intrasurgical Timescales
Author Manuscript Published OnlineFirst on March 19, 2019; DOI: 10.1158/0008-5472.CAN-18-3411 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Picosecond infrared laser desorption mass spectrometry identifies medulloblastoma subgroups on intrasurgical timescales Michael Woolmana,b,*, Claudia M. Kuzan-Fischerc,h,i,*, Isabelle Ferryc,h,i,*, Taira Kiyotad, Betty Luuc,h,i, Megan Wuc,h,i, David G. Munozf, Sunit Das c,e,f, Ahmed Amand , Michael D. Taylorb,c,e,h,i, James T. Rutkac,e,h,, Howard J. Ginsberga,e,f,g and Arash Zarrine-Afsar a,b,e,f ,** a Techna Institute for the Advancement of Technology for Health, University Health Network, 100 College Street, Toronto, ON, M5G 1P5, Canada b Department of Medical Biophysics, University of Toronto, 101 College Street, Toronto, ON, M5G 1L7, Canada c Peter Gilgan Centre for Research and Learning, Hospital for Sick Children, 686 Bay Street, Toronto, ON, M5G 0A4, Canada d Drug Discovery Program, Ontario Institute for Cancer Research, 661 University Avenue, Toronto, ON M5G 0A3, Canada e Department of Surgery, University of Toronto, 149 College Street, Toronto, ON, M5T 1P5, Canada f Keenan Research Center for Biomedical Science & the Li Ka Shing Knowledge Institute, St. Michael's Hospital, 30 Bond Street, Toronto, ON, M5B 1W8, Canada g Institute of Biomaterials and Biomedical Engineering, University of Toronto, 164 College Street, Toronto, ON, M5S 3G9, Canada h Arthur and Sonia Labatt Brain Tumor Research Centre, The Hospital for Sick Children, Toronto,