General & Thoracic Simulation Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SURGICAL INSTRUMENTS Veterinarians Are the Doctors Specializing in the Health of Animals
SURGICAL INSTRUMENTS Veterinarians are the doctors specializing in the health of animals. They do the necessary surgical operations and care for the well-being of the animal creatures. The very basic thing they need in a certain operation and care are the veterinary instruments. This will serve as the main allay of every veterinarian in providing care. (1) What are surgical instruments? Surgical instruments are essentially gadgets planned in an uncommon manner to perform particular capacities amid a surgical operation to improve viability and accomplishment of the surgery. (1) 4 Basic types of surgical instruments Surgical instruments are specially designed tools that assist health care professionals car- ry out specific actions during an operation. Most instruments crafted from the early 19th century on are made from durable stainless steel. Some are designed for general use, and others for spe- cific procedures. There are many surgical instruments available for almost any specialization in medicine. There are precision instruments used in microsurgery, ophthalmology and otology. Most surgical instruments can be classified into these 4 basic types: Cutting and Dissecting – these instruments usually have sharp edges or tips to cut through skin, tissue and suture material. Surgeons need to cut and dissect tissue to explore irregular growths and to remove dangerous or damaged tissue. These instruments have single or double razor- sharp edges or blades. Nurses need to be very careful to avoid injuries, and regularly inspect these instruments before using, for re-sharpening or replacement. 11 Iris Scissors 2016 – 1 – LV01-KA202 – 022652 This project is funded by the European Union Clamping and Occluding – are used in many surgical procedures for compressing blood vessels or hollow organs, to prevent their contents from leaking. -

Surgical Instrument Catalogue
Company Profile Dixons Surgical Instruments Ltd is a leading UK manufacturer of Surgical and Orthopaedic Instruments. We specialise in the manufacture of Precision Medical Devices and can offer a full service from Design, through Prototyping and on to Full Production Runs. The company was founded in November 1948 by Frank Dixon in Caledonian Road, London before moving to Leigh-On-Sea, Essex in 1956. Frank's son, John Dixon, joined the company in 1960 and trained in all aspects of the business. On the death of his Father in 1979, John took over as Managing Director. He was joined shortly after by his wife, Joan Dixon, who became the Financial Director. The company steadily expanded over the years and in 1989 it moved from the site in Leigh-On-Sea to a purpose built factory in Wickford, Essex, approximately 30 miles (50 Km) east of London. John and Joan's son, Jay Dixon, joined the company in 1990 and carried out a 5 year apprenticeship as a Surgical Instrument Maker. He then followed in his Father’s footsteps by training in all other aspects of the business, becoming Technical Director in 2004. In 2010 Jay Dixon was appointed Managing Director, while John Dixon moved into the role of Chairman. Joan Dixon continues to be the Financial Director. Today our Surgical and Orthopaedic Instruments are manufactured at our Wickford factory using a combination of the latest CNC controlled machines, along with the manual skills of our experienced craftsmen. This approach enables us to make Surgical and Orthopaedic Instruments in the most accurate and efficient way possible whilst still retaining that finishing touch required for truly excellent instruments. -

Hybrid Video-Assisted Thoracoscopic Surgery Sleeve Lobectomy for Non-Small Cell Lung Cancer: a Case Report
6846 iMDT Corner Hybrid video-assisted thoracoscopic surgery sleeve lobectomy for non-small cell lung cancer: a case report Chenlei Zhang1, Zhanwu Yu1, Jijia Li1, Peng Zu1, Pingwen Yu1, Gebang Wang1, Takuro Miyazaki2, Ryuichi Waseda3, Raul Caso4, Giulio Maurizi5, Hongxu Liu1 1Department of Thoracic Surgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital & Institute, Shenyang, China; 2Department of Surgical Oncology, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan; 3Department of General Thoracic, Breast, and Pediatric Surgery, Fukuoka University, Fukuoka, Japan; 4Department of Surgery, MedStar Georgetown University Hospital, Washington, DC, USA; 5Department of Thoracic Surgery, Sant’Andrea Hospital, Sapienza University of Rome, Rome, Italy Correspondence to: Hongxu Liu. Department of Thoracic Surgery, Cancer Hospital of China Medical University, Liaoning Cancer Hospital & Institute, No.44 Xiaoheyan Road, Dadong District, Shenyang 110042, China. Email: [email protected]. Submitted Feb 04, 2020. Accepted for publication Oct 24, 2020. doi: 10.21037/jtd-20-2679 View this article at: http://dx.doi.org/10.21037/jtd-20-2679 Introduction procedure. Also, hybrid VATS SL is a safer approach, especially in patients with infiltration of the pulmonary Lung cancer continues to be the leading cause of cancer- artery (PA), as it makes the surgeon more comfortable related death in China and worldwide (1,2). Sleeve during the bronchial and arterial anastomoses. Literatures lobectomy (SL) and pneumonectomy are surgical options for have shown that hybrid VATS approach has advantages for the treatment of locally advanced non-small cell lung cancer select T3 chest wall lung cancers (13) and superior sulcus (NSCLC). SL was initially intended as a parenchyma- tumors (14) over conventional open surgery. -

22Nd European Conference on General Thoracic Surgery ABSTRACTS
22ND EUROPEAO N C NFERENCE ON GENERAL THORACIC SURGERY COPENHAGEN – DENMARK 2014 22 nd European Conference European onGeneral ABSTRACTS 15 –18June2014 Copenhagen www.ests.org of Thoracic of Thoracic Surgeons SocietyEuropean – Thoracic SurgeryThoracic Denmark 22nd European Conference on General Thoracic Surgery 15 – 18 June 2014 Bella Center, Copenhagen, Denmark 01 ests2014_toc.indd 1 14.05.2014 14:05:18 22nd European Conference on General Thoracic Surgery 2 01 ests2014_toc.indd 2 14.05.2014 14:05:18 Copenhagen – Denmark – 2014 TABLE OF CONTENTS TABLE OF CONTENTS Monday, 16 June 2014 Session I/ Brompton 5 Session II/ Videos 17 Session III/ Pulmonary Non Neoplastic 23 Session IV/ Young Investigators Award 32 Session V/ Pulmonary Neoplastic I 51 Session VI/ Innovative/Experimental 63 Oscar Night Videos 78 Tuesday, 17 June 2014 Session VIII/ Mixed Thoracic I 85 Session IX/ Mixed Thoracic II 97 Session X/ Pulmonary Neoplastic II 109 Session XI/ Videos II 123 Session XII/ Interesting Cases 129 Session XIII/ Oesophagus/Mediastinum 134 Session XIV/ Airway/Transplantation 146 Session XV/ Chest Wall/Diaphragm/Pleura 155 Session XVI/ MITIG – VATS RESECTIONS 166 Posters 178 Nurse Symposium-Oral 332 Nurse Symposium-Posters 342 List of Authors 361 3 01 ests2014_toc.indd 3 14.05.2014 14:05:18 22nd European Conference on General Thoracic Surgery ABSTRACTS 4 02_ests2014.indd 4 14.05.2014 14:07:30 Abstracts 001 - 006 Copenhagen – Denmark – 2014 ABSTRACTS Monday A.M. MONDAY, 16 JUNE 2014 08:30 - 10:30 SESSION I: BROMPTON B-001 ERGON – TRIAL: ERGONOMIC EVALUATION OF SINGLE-PORT ACCESS VERSUS THREE-PORT ACCESS VIDEO-ASSISTED THORACIC SURGERY Luca Bertolaccini1, A. -

The Introductory Guide/Basic Course #1 Chapter I About Sklar for 123 Years, Sklar Has Set the Standard for Surgical Instrumentation
Surgical Instruments: The Introductory Guide/Basic Course #1 Chapter I About Sklar For 123 years, Sklar has set the standard for surgical instrumentation. In 1892, German born instrument maker John Sklar, founded the company to fill a need for American made surgical instruments and the rest is history. Sklar rose to prominence during World Wars I and II and was awarded the principal contract as the surgical instrument provider for the United States military. This contract established Sklar as the industry leader and placed it on the forefront of the surgical marketplace, where it went on to receive Certificates of Merit and Achievement from the U.S. Navy and six Army Navy “E” Production Awards. During the 1930s, Sklar’s research department helped to develop a stainless steel alloy especially suited to the manufacture of surgical instruments. The company’s investment in research was justified long-term; most surgical instruments are still made of long-lasting, rust resistant, stainless steel. Today, Sklar is headquartered in West Chester, Pennsylvania where it remains the authority on the manufacture of high quality surgical instruments to medical professionals in 75 countries worldwide. Throughout its history, Sklar has collaborated with leading surgeons and medical facilities to develop thousands of unique surgical instrument patterns. In recent years, Sklar has expanded its product line to include more than 19,000 precision crafted, stainless steel instruments: the largest offering of surgical instruments in the world. Specialty practices include: OB/GYN, Orthopedic, ENT, Cardiovascular, Endoscopic, Dermatology, Podiatry, Veterinary, Dental, etc. The prevention and reduction of healthcare associated infection (HAI) is a top priority in medical facilities today. -

Medicure Instruments
MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-503 MI-502 MI-501 KOCHER’S MOSQUITO FORCEPS FORCEPS SPENCER WELLS ARTERY FORCEPS STAINLESS STEEL STRAIGHT ARTERY MI-504 MI-505 MI-506 MI-507 MI-508 KOCHER’S DISSECTING FORCEPS DISSECTING FORCEPS RUSSIAN DISSECTING FINE DISSECTING FORCEPS STAINLESS STEEL - PLAIN STAINLESS STEEL - TOOTH FORCEPS FORCEPS - PLAIN CURVED ARTERY MI-509 MI-510 MI-511 TOWEL CLIP FINE DISSECTING DENNIS BROWNE TOWEL FORCEPS CROSS-ACTION FORCEPS - TOOTH DISSECTING FORCEPS BACKHAUS GENERAL SURGERY INSTRUMENTS MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-512 MI-513 MI-513 MI-514 LISTER SINUS B.P. HANDLE NO. 3 B.P. HANDLE NO. 4 B.P. HANDLE NO. 7 MALLEBLE PROBE DRESSING FORCEPS WITH EYE MI-515 MI-5164 MI-514 BOZEMANN KILNER MI-517 MAYO HEGARS NEEDLE HOLDERS NEEDLE HOLDERS FINE DRESSING SCISSORS NEEDLE HOLDERS STRAIGHT STRAIGHT STRAIGHT (SHARP x BLUNT) STRAIGHT STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL MI-521 MI-518 MI-519 MI-520 STITCH RIBBON SCISSORS DRESSING SCISSORS IRIS SCISSORS KNAPP SCISSORS STRAIGHT STRAIGHT (SHARP x SHARP) STRAIGHT STRAIGHT STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL GENERAL SURGERY INSTRUMENTS MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-523 MI-524 MI-525 STEVENS SCISSORS MAYO SCISSORS GREEN BERG SCISSORS MI-522 STRAIGHT STRAIGHT (KILNER) METZENBAUM SCISSORS STAINLESS STEEL STRAIGHT STAINLESS STEEL STRAIGHT STAINLESS STEEL STAINLESS STEEL MI-528 MI-529 ALLIS TISSUE POTT’S ANGLED GRASPING FORCEPS MI-526 -

STILLE Surgical Instruments Kirurgisk Perfektion I Närmare 180 År Surgical Perfection for Almost 180 Years
STILLE Surgical Instruments Kirurgisk perfektion i närmare 180 år Surgical Perfection for almost 180 years I närmare 180 år har vi utvecklat och tillverkat de bästa kirurgiska For almost 180 years, we have developed and manufactured the best instrumenten till världens mest krävande kirurger. Vi vill rikta ett stort surgical instruments for the world’s most demanding surgeons. tack till alla våra trogna kunder och samtidigt välkomna våra nya kunder. We would like to extend a heartfelt thank you to all our loyal I den här katalogen presenterar vi vårt kompletta sortiment av customers and a warm welcome to our new customers. In this catalog STILLEs original instrument. we present our complete range of STILLE original surgical instruments. Precision, hållbarhet och känsla är typiska egenskaper för alla Precision, durability and feel are characteristic qualities of all STILLE STILLE-instrument. Den stora majoriteten är handgjorda av våra instruments. The vast majority are handcrafted by our highly skilled skickliga instrumentmakare Eskilstuna. Instrumentets resa från rundstål instrument makers in Eskilstuna, west of Stockholm, Sweden. The instru- till ett färdigt instrument är lång, och består av många tillverkningssteg. ments’ journey from a rod of stainless steel to a finished instrument is a STILLEs unika tillverkningsmetod och användning av enbart det bästa long one, involving multiple stages. STILLE’s unique method of crafting its materialet ger våra instrument deras unika känsla och hållbarhet. instrument materials, and its usage of only the very highest-grade steels, give our instruments their unique feel and durability. I det första kapitlet hittar du våra saxar, allt från vanliga operationssaxar till våra unika SuperCut och Diamond SuperCut-saxar. -

The Basic Surgery Kit
GLOBAL EXCLUSIVE > SURGERY > PEER REVIEWED The Basic Surgery Kit Jan Janovec, MVDr, MRCVS VRCC Veterinary Referrals Laurent Findji, DMV, MS, MRCVS, DECVS Fitzpatrick Referrals Considering the virtually limitless range of surgical instruments, it can be difficult to assemble a cost-effective basic surgery kit. Some instruments may misleadingly appear multipurpose, but their misuse may damage them, leading to unnecessary replacement costs or, worse, intraoperative accidents putting the patient’s safety at risk. Many instru- ments are available in different qualities and materials (eg, tungsten carbide instruments— more expensive but much more resistant to wear and corrosion than stainless steel) and Minimal Basic Surgery Kit varied sizes to match the purpose of their use as well as the size of the surgeon’s hand. n 1 instrument case Cutting Instruments n 1 scalpel handle Scalpel n 1 pair Mayo scissors The scalpel is an indispensible item in a surgical kit designed to make sharp incisions. Scalpel incision is the least traumatic way of dissection, but provides no hemostasis. n 1 pair Metzenbaum scissors Scalpel handles come in various sizes, each accommodating a range of disposable n 1 pair suture scissors blades (Figure 1). Entirely disposable scalpels are also available. n 1 pair Mayo-Hegar needle holder Scissors n 1 pair Brown-Adson tissue forceps Scissors are used for cutting, albeit with some crushing effect, and for blunt dissection. n 1 pair DeBakey tissue forceps Fine scissors, such as Metzenbaum scissors (Figure 2), should be reserved for cutting n 4 pairs mosquito hemostatic forceps and dissecting delicate tissues. Sturdier scissors, such as Mayo or suture scissors, are designed for use on denser tissues (eg, fascia) or inanimate objects (eg, sutures, drapes). -

Handling of Instruments
Limbs & Things TM learning online Handling of Instruments Overview If you are new to suturing, you will need to learn to recognize each of the instruments you are going to use, understand their function and practise the basic techniques of using them. 1 Scalpel A scalpel is a razor-edged blade on a handle. There are two types of surgical scalpel: reusable and disposable. Reusable scalpels consist of a blade that is replaced after every use, attached to a stainless steel handle that can be sterilised and re-used multiple times. In a hospital setting, this type is more likely to be used in order to reduce waste and to allow doctors to work with a variety of blades and handle sizes. Disposable surgical scalpels are usually single-piece with a plastic handle. This is the type provided in our Hands-on Kit for practice. Although you will use the same scalpel multiple times for practice, in a clinical setting you would dispose of the entire scalpel after a single use. 1.1 Principles A scalpel is essential for incising the skin and for sharp dissection. Held flat, it can also be useful for carefully undermining the skin edge to relieve tension. A razor edged blade engages over a flange on the scalpel handle. Several sizes of scalpel handle are available and size 3 is appropriate for most purposes. Each handle can be fitted with disposable blades of different shapes. The scalpel can be held in one of two ways: - For making large incisions e.g. laparotomy, and subcutaneous fat dissection, hold the scalpel like a table knife, with your index finger guiding the blade. -
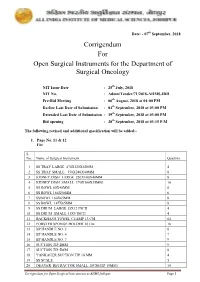
Corrigendum for Open Surgical Instruments for the Department Of
Date: - 07th September, 2018 Corrigendum For Open Surgical Instruments for the Department of Surgical Oncology NIT Issue Date : 25th July, 2018 NIT No. : Admn/Tender/71/2018-AIIMS.JDH Pre-Bid Meeting : 06th August, 2018 at 04:00 PM Earlier Last Date of Submission : 04th September, 2018 at 03:00 PM Extended Last Date of Submission : 19th September, 2018 at 03:00 PM Bid opening : 20th September, 2018 at 03:15 P.M The following revised and additional specification will be added:- 1. Page No. 11 & 12 For S. No. Name of Surgical Instrument Quantity 1 SS TRAY LARGE 470X320X50MM 4 2 SS TRAY SMALL 350X240X40MM 8 3 KIDNEY DISH LARGE 250X140X40MM 8 4 KIDNEY DISH SMALL 170X100X35MM 10 5 SS BOWL 80X40MM 6 6 SS BOWL 166X50MM 6 7 SSBOWL 160X65MM 8 8 SS BOWL 147X65MM 8 9 SS DRUM LARGE 15X12 INCH 4 10 SS DRUM SMALL 11X9 INCH 4 11 BACKHAUS TOWEL CLAMP 13 CM 64 12 FORSTER SPONGE HOLDER 18 Cm 18 13 BP HANDLE NO. 3 8 14 BP HANDLE NO. 4 7 15 BP HANDLE NO. 7 9 16 SUCTION TIP 2MM 9 17 SUCTION TIP 5MM 8 18 YANKAUER SUCTION TIP 10 MM 4 19 SS SCALE 5 20 DEAVER RETRACTOR SMALL 18CM(TIP 19MM) 14 Corrigendum for Open Surgical Instruments at AIIMS Jodhpur Page 1 21 DEAVER RETRACTOR MEDIUM 30.5CM (TIP 25 MM) 10 22 DEAVER RETRACTOR LARGE 31.5CM (TIP 50MM) 10 23 DOYEN’S RETRACTOR 4 24 MORRIS RETRACTOR 25cm ( BLADE 7x4cm) 6 25 SKIN HOOK 32 26 LANGENBECK RETRACTOR SMALL 16cm (TIP 21x 8mm) 16 27 LANGENBECK RETRACTOR MEDIUM 22cm (TIP 50x11mm) 16 28 LANGENBECK RETRACTOR LARGE 22.5cm (TIP 85x15mm) 14 29 C ZERNY RETRACTOR 17.2 cm 14 30 VEIN RETRACTOR 18 31 BALFOUR ABDOMINAL RETRACTOR 20cm 3 32 MASTOID RETRACTOR 4 33 PERIOSTEUM ELEVATOR SHARP 4 34 PERIOSTEUM ELEVATOR BLUNT 4 35 DISSECTING TOOTH FORCEPS 15 CM 16 36 DISSECTING PLAIN FORCEPS 18 CM 16 37 ARTERY FORCEPS CVD 15 CM 36 38 ARTERY FORCEPS ST. -

(12) United States Patent (10) Patent No.: US 6,652,450 B2 Neisz Et Al
USOO665245OB2 (12) United States Patent (10) Patent No.: US 6,652,450 B2 Neisz et al. (45) Date of Patent: Nov. 25, 2003 (54) IMPLANTABLE ARTICLE AND METHOD FOREIGN PATENT DOCUMENTS FOR TREATING URINARY INCONTINENCE USING MEANS FOR REPOSITONING THE RE 5, c. 33. IMPLANTABLE ARTICLE EP O470308 A1 2/1992 EP O 650 703 A1 6/1994 (75) Inventors: Johann J. Neisz, Coon Rapids, MN (US); John W. Westrum, Jr., Prior (List continued on next page.) Lake, MN (US); Christopher H. Porter, Woodinville, WA (US) OTHER PUBLICATIONS Beck, Peter R. et al., Treatment of Urinary Stress Inconti (73) ASSignee: η Mystems Inc., nence With Anterior Colporrhaphy, Obstetrics and Gynecol InnelOn Ka, ogy, vol 59 (No. 3), pp. 269-274 (Mar. 1982). (*) Notice: Subject to any disclaimer, the term of this Es ES, MD, A Modified Play t atent is extended or adjusted under 35 patient Bladder Neck Suspension System, Journal of Urol C. 154(b) by 0 days ogy, vol. 152, pp. 23.16-2320 (Dec. 1994). a -- y yS. Benderev, Theodore V., MD, Anchor Fixation and Other Modifications of Endoscopic Bladder Neck Suspension, (21) Appl. No.: 09/917,562 Urology, vol 40, No. 5, pp. 409–418 (Nov. 1992). (22) Filed: Jul. 27, 2001 Das, Sakti et al., Laparoscopic Colpo-Suspension, The O O Journal of Urology, vol. 154, pp. 1119-1121 (Sep. 1995). (65) Prior Publication Data Gilja, Ivan et al., A Modified Raz Bladder Neck Suspension US 2002/0107430 A1 Aug. 8, 2002 Operation (Transvaginal Burch), The Journal of Urology, vol. 153, pp. 1455–1457 (May 1995). -
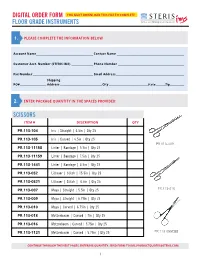
Floor Grade Instruments
DIGITAL ORDER FORM YOU MUST DOWNLOAD THIS FILE TO COMPLETE FLOOR GRADE INSTRUMENTS 1. PLEASE COMPLETE THE INFORMATION BELOW Account Name__________________________________________________ Contact Name ___________________________________________________________ Customer Acct. Number (STERIS IMS) ___________________ Phone Number __________________________________________________________ Fax Number _____________________________________________________ Email Address ____________________________________________________________ Shipping PO# _______________________ Address _____________________________________City __________________________________State ________ Zip_____________ 2. ENTER PACKAGE QUANTITY IN THE SPACES PROVIDED: SCISSORS ITEM # DESCRIPTION QTY PR.113-104 Iris | Straight | 4.5in | Qty 25 PR.113-105 Iris | Curved | 4.5in | Qty 25 PR.113-009 PR.113-11158 Lister | Bandage | 5.5in | Qty 25 PR.113-11159 Lister | Bandage | 7.5in | Qty 25 PR.113-1441 Lister | Bandage | 4.5in | Qty 25 PR.113-052 Littauer | Stitch | 15.5in | Qty 25 PR.113-0521 Littauer | Stitch | 4.5in | Qty 25 PR.113-007 Mayo | Straight | 5.5in | Qty 25 PR.113-010 PR.113-009 Mayo | Straight | 6.75in | Qty 25 PR.113-010 Mayo | Curved | 6.75in | Qty 25 PR.113-018 Metzenbaum | Curved | 7in | Qty 25 PR.113-016 Metzenbaum | Curved | 5.75in | Qty 25 PR.113-1121 Metzenbaum | Curved | 5.75in | Qty 25 PR.113-055CBB CONTINUE THROUGH THE NEXT PAGES, ENTERING QUANTITY. SEND FORM TO [email protected]. 1 SCISSORS ITEM # DESCRIPTION QTY PR.113-0063 Voper | Blunt | Straight