Electrophysiologic Mapping of the Extraocular Motor Nuclei
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Entrapment Neuropathy of the Central Nervous System. Part II. Cranial
Entrapment neuropathy of the Cranial nerves central nervous system. Part II. Cranial nerves 1-IV, VI-VIII, XII HAROLD I. MAGOUN, D.O., F.A.A.O. Denver, Colorado This article, the second in a series, significance because of possible embarrassment considers specific examples of by adjacent structures in that area. The same entrapment neuropathy. It discusses entrapment can occur en route to their desti- nation. sources of malfunction of the olfactory nerves ranging from the The first cranial nerve relatively rare anosmia to the common The olfactory nerves (I) arise from the nasal chronic nasal drip. The frequency of mucosa and send about twenty central proces- ocular defects in the population today ses through the cribriform plate of the ethmoid bone to the inferior surface of the olfactory attests to the vulnerability of the optic bulb. They are concerned only with the sense nerves. Certain areas traversed by of smell. Many normal people have difficulty in each oculomotor nerve are pointed out identifying definite odors although they can as potential trouble spots. It is seen perceive them. This is not of real concern. The how the trochlear nerves are subject total loss of smell, or anosmia, is the significant to tension, pressure, or stress from abnormality. It may be due to a considerable variety of causes from arteriosclerosis to tu- trauma to various bony components morous growths but there is another cause of the skull. Finally, structural which is not usually considered. influences on the abducens, facial, The cribriform plate fits within the ethmoid acoustic, and hypoglossal nerves notch between the orbital plates of the frontal are explored. -

CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit
228 CHAPTER 8 Face, Scalp, Skull, Cranial Cavity, and Orbit MUSCLES OF FACIAL EXPRESSION Dural Venous Sinuses Not in the Subendocranial Occipitofrontalis Space More About the Epicranial Aponeurosis and the Cerebral Veins Subcutaneous Layer of the Scalp Emissary Veins Orbicularis Oculi CLINICAL SIGNIFICANCE OF EMISSARY VEINS Zygomaticus Major CAVERNOUS SINUS THROMBOSIS Orbicularis Oris Cranial Arachnoid and Pia Mentalis Vertebral Artery Within the Cranial Cavity Buccinator Internal Carotid Artery Within the Cranial Cavity Platysma Circle of Willis The Absence of Veins Accompanying the PAROTID GLAND Intracranial Parts of the Vertebral and Internal Carotid Arteries FACIAL ARTERY THE INTRACRANIAL PORTION OF THE TRANSVERSE FACIAL ARTERY TRIGEMINAL NERVE ( C.N. V) AND FACIAL VEIN MECKEL’S CAVE (CAVUM TRIGEMINALE) FACIAL NERVE ORBITAL CAVITY AND EYE EYELIDS Bony Orbit Conjunctival Sac Extraocular Fat and Fascia Eyelashes Anulus Tendineus and Compartmentalization of The Fibrous "Skeleton" of an Eyelid -- Composed the Superior Orbital Fissure of a Tarsus and an Orbital Septum Periorbita THE SKULL Muscles of the Oculomotor, Trochlear, and Development of the Neurocranium Abducens Somitomeres Cartilaginous Portion of the Neurocranium--the The Lateral, Superior, Inferior, and Medial Recti Cranial Base of the Eye Membranous Portion of the Neurocranium--Sides Superior Oblique and Top of the Braincase Levator Palpebrae Superioris SUTURAL FUSION, BOTH NORMAL AND OTHERWISE Inferior Oblique Development of the Face Actions and Functions of Extraocular Muscles Growth of Two Special Skull Structures--the Levator Palpebrae Superioris Mastoid Process and the Tympanic Bone Movements of the Eyeball Functions of the Recti and Obliques TEETH Ophthalmic Artery Ophthalmic Veins CRANIAL CAVITY Oculomotor Nerve – C.N. III Posterior Cranial Fossa CLINICAL CONSIDERATIONS Middle Cranial Fossa Trochlear Nerve – C.N. -

Botulinum Toxin to Improve Lower Facial Symmetry in Facial Nerve Palsy SA Sadiq Et Al 1432
Eye (2012) 26, 1431–1436 & 2012 Macmillan Publishers Limited All rights reserved 0950-222X/12 www.nature.com/eye 1;2 3 4 Botulinum toxin to SA Sadiq , S Khwaja and SR Saeed CLINICAL STUDY improve lower facial symmetry in facial nerve palsy Abstract Introduction In long-standing facial palsy, Introduction muscles on the normal side overcontract In facial palsy, paralysis of muscles on the causing difficulty in articulation, eating, affected side of the face results in loss of drinking, cosmetic embarrassment, and forehead creases, loss of the nasolabial fold, psychological effects as patients lack lagophthalmos, brow droop, and drooping of confidence in public. the corner of the mouth. In contrast, muscles on Methods We injected botulinum toxin A the unaffected side of the face no longer have (BTXA) into the normal contralateral smile opposing forces.1 This may cause difficulty in muscles to weaken them and restore symmetry 1Manchester Royal Eye articulation, eating, drinking, and is often to both active and passive movements by Hospital, Manchester, UK cosmetically unacceptable to patients because of neutralising these overacting muscles. asymmetry, especially when speaking, smiling, 2 Results A total of 14 patients received BTXA The University of and laughing. There are significant Manchester, Manchester (79% women, median age 47 years, average psychological effects as patients lack the Academic Health Science length of palsy 8 years). They were all difficult confidence to carry out many daily activities in Centre, Central Manchester cases graded between 2 and 6 (average grade 3 Foundation Trust, public, such as appearing in photographs. House–Brackmann). All 14 patients reported Manchester, UK Although management is difficult, there are a improved facial symmetry with BTXA (dose range of reanimation options available. -

Anatomy of the Periorbital Region Review Article Anatomia Da Região Periorbital
RevSurgicalV5N3Inglês_RevistaSurgical&CosmeticDermatol 21/01/14 17:54 Página 245 245 Anatomy of the periorbital region Review article Anatomia da região periorbital Authors: Eliandre Costa Palermo1 ABSTRACT A careful study of the anatomy of the orbit is very important for dermatologists, even for those who do not perform major surgical procedures. This is due to the high complexity of the structures involved in the dermatological procedures performed in this region. A 1 Dermatologist Physician, Lato sensu post- detailed knowledge of facial anatomy is what differentiates a qualified professional— graduate diploma in Dermatologic Surgery from the Faculdade de Medician whether in performing minimally invasive procedures (such as botulinum toxin and der- do ABC - Santo André (SP), Brazil mal fillings) or in conducting excisions of skin lesions—thereby avoiding complications and ensuring the best results, both aesthetically and correctively. The present review article focuses on the anatomy of the orbit and palpebral region and on the important structures related to the execution of dermatological procedures. Keywords: eyelids; anatomy; skin. RESU MO Um estudo cuidadoso da anatomia da órbita é muito importante para os dermatologistas, mesmo para os que não realizam grandes procedimentos cirúrgicos, devido à elevada complexidade de estruturas envolvidas nos procedimentos dermatológicos realizados nesta região. O conhecimento detalhado da anatomia facial é o que diferencia o profissional qualificado, seja na realização de procedimentos mini- mamente invasivos, como toxina botulínica e preenchimentos, seja nas exéreses de lesões dermatoló- Correspondence: Dr. Eliandre Costa Palermo gicas, evitando complicações e assegurando os melhores resultados, tanto estéticos quanto corretivos. Av. São Gualter, 615 Trataremos neste artigo da revisão da anatomia da região órbito-palpebral e das estruturas importan- Cep: 05455 000 Alto de Pinheiros—São tes correlacionadas à realização dos procedimentos dermatológicos. -

Double-Bellied Superior Rectus Muscle
Surgical and Radiologic Anatomy (2019) 41:713–715 https://doi.org/10.1007/s00276-019-02211-0 ANATOMIC VARIATIONS Double-bellied superior rectus muscle Satheesha B. Nayak1 · Surekha D. Shetty1 · Naveen Kumar1 · Ashwini P. Aithal1 Received: 3 September 2018 / Accepted: 23 February 2019 / Published online: 7 March 2019 © Springer-Verlag France SAS, part of Springer Nature 2019 Abstract Congenital variations of extraocular muscles are rare. We report a double-bellied superior rectus muscle, observed in an adult male cadaver aged 70 years. The superior rectus muscle had two equal-sized bellies, which took separate origins from the common tendinous ring and united to form a common belly 1 cm before the insertion. Due to the duplication, the muscle extended laterally beyond the levator palpebrae superioris. Both its bellies were supplied by oculomotor nerve. To the best of our knowledge, this is the first report on doubling of the belly of the superior rectus muscle. Keywords Extraocular · Orbit · Superior rectus muscle · Eye movement · Strabismus Introduction Case report Voluntary movements of the eyeball are performed by six During dissection classes for the first-year medical students, extraocular muscles, namely superior rectus muscle, the we observed a unique variation in the right orbit of an adult inferior rectus muscle, medial rectus muscle, lateral rectus male cadaver aged 70 years. The cadaver was donated to the muscle, superior oblique muscle, and inferior oblique mus- department for teaching and research purpose. No history of cles. Variations of these muscles can result in restrictions of strabismus or visual defects is available. The variation was movements of eyeball, causing strabismus. -

SŁOWNIK ANATOMICZNY (ANGIELSKO–Łacinsłownik Anatomiczny (Angielsko-Łacińsko-Polski)´ SKO–POLSKI)
ANATOMY WORDS (ENGLISH–LATIN–POLISH) SŁOWNIK ANATOMICZNY (ANGIELSKO–ŁACINSłownik anatomiczny (angielsko-łacińsko-polski)´ SKO–POLSKI) English – Je˛zyk angielski Latin – Łacina Polish – Je˛zyk polski Arteries – Te˛tnice accessory obturator artery arteria obturatoria accessoria tętnica zasłonowa dodatkowa acetabular branch ramus acetabularis gałąź panewkowa anterior basal segmental artery arteria segmentalis basalis anterior pulmonis tętnica segmentowa podstawna przednia (dextri et sinistri) płuca (prawego i lewego) anterior cecal artery arteria caecalis anterior tętnica kątnicza przednia anterior cerebral artery arteria cerebri anterior tętnica przednia mózgu anterior choroidal artery arteria choroidea anterior tętnica naczyniówkowa przednia anterior ciliary arteries arteriae ciliares anteriores tętnice rzęskowe przednie anterior circumflex humeral artery arteria circumflexa humeri anterior tętnica okalająca ramię przednia anterior communicating artery arteria communicans anterior tętnica łącząca przednia anterior conjunctival artery arteria conjunctivalis anterior tętnica spojówkowa przednia anterior ethmoidal artery arteria ethmoidalis anterior tętnica sitowa przednia anterior inferior cerebellar artery arteria anterior inferior cerebelli tętnica dolna przednia móżdżku anterior interosseous artery arteria interossea anterior tętnica międzykostna przednia anterior labial branches of deep external rami labiales anteriores arteriae pudendae gałęzie wargowe przednie tętnicy sromowej pudendal artery externae profundae zewnętrznej głębokiej -

A- and V-Patterns and Oblique Muscle Overaction A- and V-Patterns
18 A- and V-Patterns and Oblique Muscle Overaction A- and V-Patterns Clinical Features Etiology Management with Horizontal Rectus Muscle Offsets Inferior Oblique Overaction Etiology Clinical Features Differential Diagnosis Management Superior Oblique Overaction Etiology Clinical Features Differential Diagnosis Management Superior Oblique Weakening Procedures Complications A- and V-patterns of strabismus are changes in the horizontal deviation as the patient looks up and down. They are usually associated with oblique dysfunction, either overaction or paresis. Primary oblique muscle overaction is when an oblique muscle is too strong for its antagonist and there is no known cause. Secondary oblique overaction is caused by a paresis of the antagonist muscle. A superior oblique paresis results in inferior oblique overaction, and inferior oblique paresis results in superior oblique overaction. This chapter covers the management of A- and V- patterns and primary oblique muscle overaction. A- and V-Patterns CLINICAL FEATURES A-patterns are defined as increasing divergence in down gaze (>10 prism diopters [PD]), whereas Vpatterns are increased divergence (>15 prism diopters) in up gaze. The type of A- or V-pattern helps identify the cause. Superior oblique paresis produces a V-pattern, arrow subtype, with convergence in down gaze. The arrow pattern subtype indicates a lack of abduction in down gaze, the field of action of the superior oblique muscles. Inferior oblique overaction, on the other hand, has a V-pattern, Y subtype, with increased abduction in up gaze. The Y-pattern occurs because the field of action of the inferior oblique muscles is up gaze and they are abductors. Lambda subtype is typically associated with superior oblique overaction, with increased abduction in down gaze, because the field of action is in down gaze. -

Muscles of the Head, Neck, and Torso
MusclesMuscles ofof thethe Head,Head, Neck,Neck, andand TorsoTorso DanilDanil HHammoudi.MDammoudi.MD MuscleMuscle myofibril Fiber/NerveFiber/Nerve motor end plate TerminalTerminal sarcomere I-band A-band Z-line sarcolemma motor neuron endomysium SomeSome definitiondefinition •• aponeurosisaponeurosis -- AA sheetlikesheetlike fibrousfibrous membrane,membrane, resemblingresembling aa flattenedflattened tendon,tendon, thatthat servesserves asas aa fasciafascia toto bindbind musclesmuscles togethertogether oror asas aa meansmeans ofof connectingconnecting musclemuscle toto bobone.ne. anyany ofof thethe deeperdeeper andand thickerthicker fasciafascia thatthat attachattach musclesmuscles toto bobones;nes; resembleresemble flattenedflattened tendons,tendons, •• ffasciaascia -- aa sheetsheet oror bandband ofof fibroufibrouss connectiveconnective tissuetissue separatingseparating oror bindingbinding togethertogether musclesmuscles andand organsorgans etcetc •• Ligament:Ligament: AA ligaligamentment isis aa toughtough bandband ofof connectiveconnective tisstissueue thatthat connectsconnects variousvarious structuresstructures suchsuch asas twotwo bones.bones. "Ligament""Ligament" isis aa fittingfitting term;term; itit comescomes fromfrom thethe LatinLatin "ligare""ligare" meaningmeaning "to"to bindbind oror tie.tie. •Tendon: The tissue by which a muscle attaches to bone. A tendon is somewhat flexible, but fibrous and tough. MusclesMuscles ofof thethe headhead •• EEpicranius.:picranius.: OccipitofrontalisOccipitofrontalis TheThe epicraniusepicranius -

Differences in Extrinsic Eye Muscles and Dissection Protocols
Iowa State University Capstones, Theses and Creative Components Dissertations Spring 2020 Comparative anatomy case study: differences in extrinsic eye muscles and dissection protocols Erin Ruden Follow this and additional works at: https://lib.dr.iastate.edu/creativecomponents Part of the Animal Structures Commons, and the Body Regions Commons Recommended Citation Ruden, Erin, "Comparative anatomy case study: differences in extrinsic eye muscles and dissection protocols" (2020). Creative Components. 543. https://lib.dr.iastate.edu/creativecomponents/543 This Creative Component is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Creative Components by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. P a g e | 1 Comparative anatomy case study: differences in extrinsic eye muscles and dissection protocols Abstract: There have been notable studies comparing the eye placement between predators and prey, which can be further categorized as omnivore, carnivore, and herbivore. The purpose of this study was to determine if eye placement correlated with extrinsic eye muscle differences among the classification of animals (predator vs. prey and omnivore vs. carnivore vs. herbivore). For an omnivore, a human orbit was dissected. A cat was dissected to represent a carnivore and a goat was dissected to represent an herbivore. Dissection protocol for the cat and goat were created due to the lack of dissections of these muscles. Unfortunately, data collection was incomplete due to the social distancing policy on Iowa State University’s campus because of COVID-19. -

Anatomy and Physiology Model Guide Book
Anatomy & Physiology Model Guide Book Last Updated: August 8, 2013 ii Table of Contents Tissues ........................................................................................................................................................... 7 The Bone (Somso QS 61) ........................................................................................................................... 7 Section of Skin (Somso KS 3 & KS4) .......................................................................................................... 8 Model of the Lymphatic System in the Human Body ............................................................................. 11 Bone Structure ........................................................................................................................................ 12 Skeletal System ........................................................................................................................................... 13 The Skull .................................................................................................................................................. 13 Artificial Exploded Human Skull (Somso QS 9)........................................................................................ 14 Skull ......................................................................................................................................................... 15 Auditory Ossicles .................................................................................................................................... -
Neurological Examination
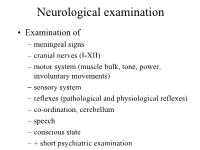
Neurological examination • Examination of – meningeal signs – cranial nerves (I-XII) – motor system (muscle bulk, tone, power, involuntary movements) – sensory system – reflexes (pathological and physiological reflexes) – co-ordination, cerebellum – speech – conscious state – + short psychiatric examination MENINGEAL SIGNS • may be caused by: – meningitis (bacterial or viral infection of meninges) – blood in the subarachnoidal space – infiltration of meninges by carcinoma cells – increased intracranial pressure – dehydration Optic nerve (II) Visual acuity Visual field Fundus - Optic disc • Retina • Optic nerve • Chiasm • Optic tract • Lateral geniculate body • Optic radiation • Visual (occipital) cortex VISUAL FIELD - LENS - reversed image 1. The lens produces reversed image 2. Fibers, originating from the upper part of the retina keeps their superior/upper position through the whole optic pathway Visual field Oculomotor (III), trochlear (IV), and abducent (VI) nerves • Oculomotor nerve (III) innervates: medial rectus, superior rectus, inferior rectus, inferior oblique muscles + superior palpebral levator muscle, ciliary muscle, pupillary constrictor muscle • Trochlear nerve (IV) innervates: superior oblique muscle • Abducent nerve (VI) innervates: lateral rectus muscle Nuclei of culomotor (III), trochlear (IV), and abducent (VI) nerves • Oculomotor nerve – Main nucleus (mesencephalon) of oculomotor nerve controls medial rectus, superior rectus, inferior rectus, inferior oblique muscles + superior palpebral levator muscle – Edinger-Westphal -

FIPAT-TA2-Part-2.Pdf
TERMINOLOGIA ANATOMICA Second Edition (2.06) International Anatomical Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TA2, PART II Contents: Systemata musculoskeletalia Musculoskeletal systems Caput II: Ossa Chapter 2: Bones Caput III: Juncturae Chapter 3: Joints Caput IV: Systema musculare Chapter 4: Muscular system Bibliographic Reference Citation: FIPAT. Terminologia Anatomica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, 2019 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Anatomica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput II: OSSA Chapter 2: BONES Latin term Latin synonym UK English US English English synonym Other 351 Systemata Musculoskeletal Musculoskeletal musculoskeletalia systems systems