Ii. Grenada Health System: National and Regional Structures and Influences 22
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Factors That Influence the Provision of Intrapartum and Postnatal Care By
Cochrane Database of Systematic Reviews Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low- and middle- income countries: a qualitative evidence synthesis (Review) Munabi-Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H Munabi-Babigumira S, Glenton C, Lewin S, Fretheim A, Nabudere H. Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low- and middle-income countries: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews 2017, Issue 11. Art. No.: CD011558. DOI: 10.1002/14651858.CD011558.pub2. www.cochranelibrary.com Factors that influence the provision of intrapartum and postnatal care by skilled birth attendants in low- and middle-income countries: a qualitative evidence synthesis (Review) Copyright © 2018 The Authors. Cochrane Database of Systematic Reviews published by John Wiley & Sons, Ltd. on behalf of The Cochrane Collaboration. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 4 BACKGROUND .................................... 21 Figure1. ..................................... 23 OBJECTIVES ..................................... 24 METHODS ...................................... 24 RESULTS....................................... 27 Figure2. ..................................... 28 Figure3. ..................................... 31 DISCUSSION .................................... -
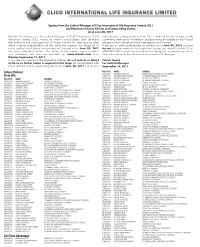
Grenada Listing
POLICY ID NAME ADDRESS POLICY ID NAME ADDRESS Update from the Judicial Manager of Clico International Life Insurance Limited (CIL) Confi rmation of Active Policies and Outstanding Claims As at June 30, 2017 Deloitte Consulting Ltd., the Judicial Manager of CLICO International Life individualised correspondence from CIL to their last known address on fi le Insurance Limited (CIL), wishes to inform policyholders and claimants confi rming their policy information and providing an update on the Phase I that further to the court approval of Phase I of the CIL restructuring plan, process and an indication of the next steps to be followed. which involves policyholders on the Barbados register, the listing of all If you are an active policyholder or claimant as at June 30, 2017 and you active policies and claims outstanding in Grenada as at June 30, 2017 do not see your name on the respective listings, you should contact CIL at has been published below. The listing of the names, policy numbers (473) 440-2632 to make an appointment to bring your original policy and or and addresses will also be available on www.clicolife.com from claim information to the offi ce on Young Street in St. Georges. Monday September 11, 2017. If you see your name on the respective listings, do not contact or attend Patrick Toppin at CIL as no further action is required at this stage. All policyholders with For Judicial Manager active policies and or outstanding claims as of June 30, 2017 will be sent September 15, 2017 POLICY ID NAME ADDRESS Inforce Policies IGJ0003065 ALEXANDER, KENRICK E GRAND BACOLET, C/O MUNICH P.O., ST.ANDREW’S Term Life IGJ0004197 ALEXANDER, KERRY ORLANDO C/O MORNE FENDUE P.O, ST.PATRICK’S GNH0056502 ALEXANDER, RONALD C. -

LMIC Databases August 2013
LMIC Databases August 2013 A collection of databases, web sites and journals relevant to Low- and Middle-Income Countries (LMICs) This list has been put together in a collaborative effort by Cochrane Groups, the WHO Library and volunteers outside the Cochrane Collaboration. Please click the navigation pane to see the list content. For information on how the list has developed, please see the history note at the bottom of this document. Any comments you might have to the list, or suggestions for additional resources, will be most welcome. Contact person: [email protected] Global Databases 3ie Database of Impact Evaluations URL http://www.3ieimpact.org/en/evidence/ Provider 3ie Region Global – low and middle income countries Description Covers impact evaluations conducted in low- and middle- income countries. Search language English Format Web Content language English Content Impact evaluation studies Draws from a wide range of sources (22 databases and 12 research web sites) including grey literature To be included, the study must meet 3ie’s quality standards. MEDLINE overlap Unclear Database size Circa 750 publications [February 2013] Journals indexed Not applicable. Individual papers included Other items indexed Unclear Update frequency Unclear Search options Basic keyword (single box) and advanced search. Search function Advanced search has options to search within title, author, country, region, sector (topic), vulnerable groups, evaluation method (eg experimental, quasi-experimental), status (eg ongoing, published) and whether or not there is a gender focus. Search tips Can search for single terms or phrases. Does not appear to support Boolean logic as yet. Search example Text words in basic search (keywords) and words in title/author boxes plus drop down boxes in advanced search (see search function). -

Workers Scream Victimisation!!!
Page 1:Page 1 10/22/19 5:39 PM Page 1 9+((/3 .7$83,*+4,(2: ! "((-/',/*2, 8,*59852,.1*?.6*-.78<2072/2,*7=+;.*4=1;8>01 27<=;>,=.-+B=1./.6*5.*02<=;*=.=8<>;;.7-.;*55 27/[email protected]<=255*=5*;0.*7-,87<2-.;.- 12< =;*?.5 -8,>6.7=< *7- ;.98;= =8 =1. *;;2*,8> *<=1.6*27<><9.,=<27=1.!,=8+.; *;6.-;8+ "852,. %=*=287 .?.;B 87-*B ).-7.<-*B *7- +.;B*==1.'&;.-2='7287+;*7,18//2,.87=1. ;2-*[email protected]=1.18>;<8/ *6*7- 96 <2<=.;2<5.8/*;;2*,8> &1. B.*;85- 6*7 1*< +..7 2-.7=2/2.- *< =1. 9852,.8//2,2*5=85-" # 7.@<9*9.; 8@7.; *7- -;2?.; 8/ =1. %>C>42 <,>-8 ?*7 =1*= 27?.<=20*=8;< 1*?. 78= +..7 *+5. =8 ,86. >9 ;.02<=;*=287 " =1*= *55.0.-5B 9;8?2-.- =;*7< @2=1 *7B=1270 98<2=2?. <27,. =1. $8B*5 ;.7*-* 98;=*=287=8=1.=@8 <><9.,=<87=1.-*B8/=1. "852,.8;,.$"98<=.-=1.?2-.826*0.<8/=1. *;6.-;8++.;B 6.7*<=1.B@.;.,*9=>;.-87=1.-*B8/=1.;8+ #>*<12.;.98;=.-5B=85-9852,.27?.<=20*=8;<=1*=1. +.;B.7=.;270*7-5.*?270=1.+>25-270 -2-78=478@=1.6.7+>=@*<12;.-+B*727-2?2->*5 .<*2-=1.9852,.1*?.78=02?.7>9189.8/.?.7 /;868?.;87=1.<2<=.;2<5.=89;8?2-.=;*7<98;=* =>*55B0.==270*5.*-=1*=,*79>==1.6;201=87=1. -

Report on Strengthening Research Capacities for Health in the Caribbean, 2007–2017 Executive Summary Iii
Executive Summary i REPORT ON STRENGTHENING RESEARCH CAPACITIES FOR HEALTH IN THE CARIBBEAN 2007-2017 ii Report on Strengthening Research Capacities for Health in the Caribbean, 2007–2017 Executive Summary iii REPORT ON STRENGTHENING RESEARCH CAPACITIES FOR HEALTH IN THE CARIBBEAN 2007-2017 Pan American Health Organization / World Health Organization (PAHO/WHO) Office of Knowledge Management, Bioethics and Research (KBR) Secretariat to the Advisory Committee on Health Research Washington, D.C. 2017 iv Report on Strengthening Research Capacities for Health in the Caribbean, 2007–2017 Report on Strengthening Research Capacities for Health in the Caribbean, 2007-2017 Document Number: PAHO/KBR/17-021 © Pan American Health Organization, 2017 All rights reserved. Publications of the Pan American Health Organization are available on the PAHO website (www.paho.org). Requests for permission to reproduce or translate PAHO Publications should be addressed to the Communications Department through the PAHO website (www.paho.org/ permissions). Suggested citation: Pan American Health Organization. Report on Strengthening Research Capacities for Health in the Caribbean, 2007-2017. Washington, D.C.: PAHO; 2017. Available at http://iris.paho. org/xmlui/handle/123456789/34342. Cataloguing-in-Publication (CIP) data: CIP data are available at http://iris.paho.org. Publications of the Pan American Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the Pan American Health Organization concerning the status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -
2.3 Latin America & the Caribbean
Regional Overview 2.3 Latin America & the Caribbean 99 2.3 LATIN AMERICA & THE CARIBBEAN ANTIGUA AND BARBUDA ARGENTINA THE BAHAMAS BOLIVIA BARBADOS BRAZIL BELIZE COLOMBIA BERMUDA COSTA RICA CUBA CHILE DOMINICA ECUADOR DOMINICAN REPUBLIC EL SALVADOR GRENADA GUATEMALA GUYANA HONDURAS HAITI MEXICO JAMAICA NICARAGUA PUERTO RICO PANAMA SAINT KITTS AND NEVIS PARAGUAY SAINT LUCIA PERU SAINT VINCENT AND THE GRENADINES URUGUAY SURINAME VENEZUELA TRINIDAD AND TOBAGO 100 Global State of Harm Reduction 2020 TABLE 2.3.1: Epidemiology of HIV and viral hepatitis, and harm reduction responses in the Latin America and the Caribbean Country/ People who HIV Hepatitis C Hepatitis B Harm reduction response territory with inject drugs prevalence (anti-HCV) (anti-HBsAg) reported injecting among prevalence prevalence Peer drug use1 people who among among distribution inject drugs people who people who NSP2 OAT3 DCRs4 of (%) inject drugs inject drugs naloxone (%) (%) Argentina 8,144[2] 3.5[3] 4.8[4] 1.6[4] x (M)[5] x x The Bahamas 0[6] nk nk nk x x x x Bolivia nk nk nk nk x x x x Brazil nk 5 9.9 [7]6 nk nk x x x x Chile nk nk nk nk x x x x Colombia 14,893[8] 5.5[9] 31.6[9] nk [10,11] (M)[10,11] x x Costa Rica nk7 nk nk nk x x x x Dominican Republic <1,359[13]8 3.2[13]9 22.8[14]10 nk 2[15] x x x Ecuador nk nk nk nk x x x x El Salvador nk nk nk nk x x x x Guatemala nk nk nk nk x x x x Guyana nk nk nk nk x x x x Haiti nk nk nk nk x x x x Honduras nk nk nk nk x x x x Jamaica nk nk nk nk x x x x Mexico 164,157[18] 11 4.4[19] 12 96[20] 13 0.2[4] [17] (M)[21] [21] x14 Nicaragua nk nk nk nk x x x x Panama 5,714[22] nk nk nk x x x x Paraguay nk nk 9.8[23] nk x x x x Peru nk nk nk nk x x x x Puerto Rico 28,000[24] 11.3[25] 15 78.4 - 89[27,28] 16 nk [29] (M,B)[29] [29] x Suriname nk[30] 17 nk nk nk x x x x Uruguay nk nk nk nk x x x x Venezuela nk nk nk nk x x x x nk = not known 1 Countries with reported injecting drug use according to Larney et al in 2017. -

CARPHA State of Public Health Inaugural Report 2013
Contents Abbreviations and Acronyms ..................................................................................................................................................... 11 ContentsExecutive Summary ............................................................................................................. ........................................................... 3 15 AbbreviationsFigures ....................................................................................................................... and Acronyms .......................................................................... 1120 ExecutiveTables ....................................................................................................................... Summary ........................................................................... 10 24 FiguresSection 1 Regional Health Overview ........................................................................................... ......................... 20 25 Tables1.1 Demographics .............................................................................................................. ............................................................. 23 27 Section 1.1.1 The1 Regional Caribbean Health Region Overview ................................................................................................... ............................................... 2527 1.1.1.1 Demographic overview of CARPHA Member States .............................................................................. -

Grenada: Blue Growth Coastal Master Plan
Report No: AUS20778 . Grenada Public Disclosure Authorized Grenada: Blue Growth Coastal Master Plan . {October 13, 2016} Public Disclosure Authorized . GEN04 LATIN AMERICA AND CARIBBEAN Public Disclosure Authorized Public Disclosure Authorized Standard Disclaimer: . This volume is a product of the staff of the International Bank for Reconstruction and Development/ The World Bank. The findings, interpretations, and conclusions expressed in this paper do not necessarily reflect the views of the Executive Directors of The World Bank or the governments they represent. The World Bank does not guarantee the accuracy of the data included in this work. The boundaries, colors, denominations, and other information shown on any map in this work do not imply any judgment on the part of The World Bank concerning the legal status of any territory or the endorsement or acceptance of such boundaries. Copyright Statement: . The material in this publication is copyrighted. Copying and/or transmitting portions or all of this work without permission may be a violation of applicable law. The International Bank for Reconstruction and Development/ The World Bank encourages dissemination of its work and will normally grant permission to reproduce portions of the work promptly. For permission to photocopy or reprint any part of this work, please send a request with complete information to the Copyright Clearance Center, Inc., 222 Rosewood Drive, Danvers, MA 01923, USA, telephone 978-750-8400, fax 978-750-4470, http://www.copyright.com/. All other queries on rights and licenses, including subsidiary rights, should be addressed to the Office of the Publisher, The World Bank, 1818 H Street NW, Washington, DC 20433, USA, fax 202-522-2422, e-mail [email protected]. -

Economic Survey of Latin America and the Caribbean 2019
2019 Economic Survey of Latin America and the Caribbean The new global financial context: effects and transmission mechanisms in the region Thank you for your interest in this ECLAC publication ECLAC Publications Please register if you would like to receive information on our editorial products and activities. When you register, you may specify your particular areas of interest and you will gain access to our products in other formats. www.cepal.org/en/publications ublicaciones www.cepal.org/apps 2019 Economic Survey of Latin America and the Caribbean The new global financial context: effects and transmission mechanisms in the region 2 Executive summary Economic Commission for Latin America and the Caribbean (ECLAC) Alicia Bárcena Executive Secretary Mario Cimoli Deputy Executive Secretary Raúl García-Buchaca Deputy Executive Secretary for Management and Programme Analysis Daniel Titelman Chief, Economic Development Division Ricardo Pérez Chief, Publications and Web Services Division The Economic Survey of Latin America and the Caribbean is issued annually by the Economic Development Division of the Economic Commission for Latin America and the Caribbean (ECLAC). The 2019 edition was prepared under the leadership of Daniel Titelman, Chief of the Division, and coordinated by Ramón Pineda Salazar and Daniel Titelman. In the preparation of this edition, the Economic Development Division was assisted by the Statistics Division, the Division of International Trade and Integration, the ECLAC subregional headquarters in Mexico City and Port of Spain, and the Commission’s country offices in Bogotá, Brasilia, Buenos Aires, Montevideo and Washington, D.C. Part I, entitled, “The economic situation and outlook for 2019”, was prepared with input from the following experts: Alejandra Acevedo, Claudio Aravena, Pablo Carvallo, Claudia de Camino, Ivonne González, Michael Hanni, Juan Pablo Jiménez, Noel Pérez, Esteban Pérez Caldentey, Ramón Pineda Salazar, José Antonio Sánchez, Cecilia Vera and Jürgen Weller. -
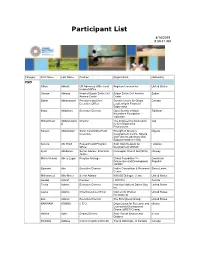
Participant List
Participant List 4/14/2019 8:59:41 AM Category First Name Last Name Position Organization Nationality CSO Jillian Abballe UN Advocacy Officer and Anglican Communion United States Head of Office Osman Abbass Head of Sudan Sickle Cell Sudan Sickle Cell Anemia Sudan Anemia Center Center Babak Abbaszadeh President and Chief Toronto Centre for Global Canada Executive Officer Leadership in Financial Supervision Ilhom Abdulloev Executive Director Open Society Institute Tajikistan Assistance Foundation - Tajikistan Mohammed Abdulmawjoo Director The Engineering Association Iraq d for Development & Environment Kassim Abdulsalam Zonal Coordinator/Field Strength in Diversity Nigeria Executive Development Centre, Nigeria and Farmers Advocacy and Support Initiative in Nig Serena Abi Khalil Research and Program Arab NGO Network for Lebanon Officer Development (ANND) Kjetil Abildsnes Senior Adviser, Economic Norwegian Church Aid (NCA) Norway Justice Maria Victoria Abreu Lugar Program Manager Global Foundation for Dominican Democracy and Development Republic (GFDD) Edmond Abu Executive Director Native Consortium & Research Sierra Leone Center Mohammed Abu-Nimer Senior Advisor KAICIID Dialogue Centre United States Aouadi Achraf Founder I WATCH Tunisia Terica Adams Executive Director Hamilton National Dance Day United States Inc. Laurel Adams Chief Executive Officer Women for Women United States International Zoë Adams Executive Director The Strongheart Group United States BAKINAM ADAMU C E O Organization for Research and Ghana Community Development Ghana -

Company List
COMPANY_CODE COMPANY_NAME ADDRESS 256455 ATTACH A LEG GRENADA MT.MORITZST.GEORGE ID623249GD TESSIL MODESTE-LEWIS GOUYAVEST. JOHN 0000001494 GRENADA CAR RENTALS [C.D.F ENTERPRISES LIMITED]GRAND ANSEST.GEORGE 0000001914 GRENLAS MANAGEMENT GRENADA POINT SALINESP.O. BOX386 0000001955 S & N SUPERMARKET SETON BROWN STREETGREMVILLEST. ANDREWS 00000040000001 DONAVON,CONSTANCE CROSS STREETST. GEORGE'SST. GEORGE 0000004494 GRENADA CAR RENTALS [C.D.F ENTERPRISES LIMITED]GRAND ANSEST.GEORGE 00000050000002 COBB-SIMON,JOAN A ST. PAUL'SST. GEORGE'SST. GEORGE 00000060000101 AUGUSTINE,BENEDICT MARIANST. GEORGE 00000070000007 ANTOINE,TREVOR MT. GAYST. GEORGE 00000090000008 ALEXIS,MARY HARVEY VALECARRIACOU 00000130000011 ALFRED,MAUDLYN MELVILLE STREETST. GEORGE'SST. GEORGE 00000140000013 ALEXANDER,RENWICK ST. GEORGE'SST. GEORGE 00000150000090 CORION,GARVEY O L'ESTERREST. ANDREW 00000180000015 ANDALL,PETER RIVER ROADST. GEORGE 00000180001951 ANDALL,PETER ST. PAULSST. GEORGE 00000180001952 ANDALL,PETER RIVER ROADST. GEORGE 00000180001953 ANDALL,PETER ST. JOHNSST. ANDREW 00000180001954 ANDALL,PETER GRENVILLEST. ANDREW 00000180002419 ANDALL,PETER SPRINGSST. GEORGE 00000200000019 ADAMS,SHEREE-ANN LANCE AUX EPINESST. GEORGE'SST. GEORGE 00000220000094 CONNAUGHT,SHEILA J VICTORIA STREETVICTORIAST. MARK 00000230000005 DUNCAN,MARY LAGOON ROADST. GEORGE'SST. GEORGE 00000240000006 ARNOLD,NORBERT ARCHIBALD AVENUEST. GEORGE 00000250000010 DRAGON,FABIAN E. GRENVILLE STREETST. GEORGE'SST. GEORGE 00000260000012 CLYNE,MICHAEL O WESTERHALLWESTERHALLST. DAVID 00000270000014 -

T: Final Country Report: Grenada Grenada
FINAL COUNTRY REPORT: FINAL COUNTRY REPORT: GRENADA GRENADA December 2009 December 2009 仮 201 Grenada Grenada Country Profile Country Profile Geographic coordinates 12o 07’ N, 61o 40’ W (This is the location of the centre of the Island) Geographic coordinates 12o 07’ N, 61o 40’ W (This is the location of the centre of the Island) Total area 344 sq km Total area 344 sq km Land area 344 sq km Land area 344 sq km Water area 0 sq km (Marine boundaries not yet delimited) Water area 0 sq km (Marine boundaries not yet delimited) Length of Coastline 251 km Length of Coastline 251 km Shelf Area 629 sq km Shelf Area 629 sq km Territorial Sea 4,504 sq km Territorial Sea 4,504 sq km Claimed EEZ 20.285 sq km Claimed EEZ 20.285 sq km Highest point (m) 840 (Mount Saint Catherine) Highest point (m) 840 (Mount Saint Catherine) Climate tropical; tempered by northeast trade winds. Climate tropical; tempered by northeast trade winds. Natural hazards lies on edge of hurricane belt; hurricane season lasts from June to Natural hazards lies on edge of hurricane belt; hurricane season lasts from June to November. November. Population 90,739 (July 2009 est.) Population 90,739 (July 2009 est.) Annual Population Growth 0.468% (2009 est.) Annual Population Growth 0.468% (2009 est.) Rate Rate Life Expectancy at birth total population: 65.95 years Life Expectancy at birth total population: 65.95 years Languages English (official), some vestigial French patois Languages English (official), some vestigial French patois Ethnic Mix black 82%, mixed black and European 13%,