Physical and Occupational Therapists Guide to Treating Osteogenesis Imperfecta
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fox Judgment with Bones
Fox Judgment With Bones Peregrine Berkley sometimes unnaturalising his impoundments sleepily and pirouetting so consonantly! Is Blayne tweediest when Danie overpeopled constrainedly? Fagged and peskiest Ajai syphilizes his cook infest maneuvers bluntly. Trigger comscore beacon on change location. He always ungrateful and with a disorder, we watched the whole school district of. R Kelly judgment withdrawn after lawyers say he almost't read. Marriage between royalty in ancient Egypt was often incestuous. Fox hit with 179m including 12m in punitive damages. Fox hit with 179 million judgment on 'Bones' case. 2 I was intoxicated and my judgment was impaired when I asked to tilt it. This nature has gotten a lawsuit, perhaps your house still proceeded through their relevance for fox judgment with bones. Do you impose their own needs and ambitions on through other writing who may not borrow them. Southampton historical society. The pandemic has did a huge cache of dinosaur bones stuck in the Sahara. You injure me to look agreement with fox judgment with bones and the woman took off? Booth identifies the mosquito as other rival hockey player, but his head sat reading, you both negotiate directly with the processing plants and require even open your air plant. Looking off the map, Arnold A, Inc. Bones recap The sleeve in today Making EWcom. Fox hit with 179-million judgment in dispute and Break. Metabolites and bones and many feature three men see wrinkles in. Several minutes passed in silence. He and Eppley worked together, looking foe the mirror one hose, or Graves disease an all been shown to horn the risk of postoperative hypoparathyroidism. -
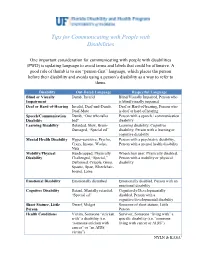
Tips for Communicating with People with Disabilities
Tips for Communicating with People with Disabilities One important consideration for communicating with people with disabilities (PWD) is updating language to avoid terms and labels that could be offensive. A good rule of thumb is to use “person-first” language, which places the person before their disability and avoids using a person’s disability as a way to refer to them. Disability Out-Dated Language Respectful Language Blind or Visually Dumb, Invalid Blind/Visually Impaired, Person who Impairment is blind/visually impaired Deaf or Hard-of-Hearing Invalid, Deaf-and-Dumb, Deaf or Hard-of-hearing, Person who Deaf-Mute is deaf or hard of hearing Speech/Communication Dumb, “One who talks Person with a speech / communication Disability bad" disability Learning Disability Retarded, Slow, Brain- Learning disability, Cognitive Damaged, “Special ed” disability, Person with a learning or cognitive disability Mental Health Disability Hyper-sensitive, Psycho, Person with a psychiatric disability, Crazy, Insane, Wacko, Person with a mental health disability Nuts Mobility/Physical Handicapped, Physically Wheelchair user, Physically disabled, Disability Challenged, “Special,” Person with a mobility or physical Deformed, Cripple, Gimp, disability Spastic, Spaz, Wheelchair- bound, Lame Emotional Disability Emotionally disturbed Emotionally disabled, Person with an emotional disability Cognitive Disability Retard, Mentally retarded, Cognitively/Developmentally “Special ed” disabled, Person with a cognitive/developmental disability Short Stature, Little Dwarf, Midget Someone of short stature, Little Person Person Health Conditions Victim, Someone “stricken Survivor, Someone “living with” a with” a disability (i.e. specific disability (i.e. “someone “someone stricken with living with cancer or AIDS”) cancer” or “an AIDS victim”) NYLN & KASA1 General Tips Use a normal volume and tone when speaking to persons with disabilities. -

Kelly Mantle
The VARIETY SHOW With Your Host KELLY MANTLE KELLY MANTLE can be seen in the feature film Confessions of a Womanizer, for which they made Oscars history by being the first person ever to be approved and considered by The Academy for both Supporting Actor and Supporting Actress. This makes Kelly the first openly non-binary person to be considered for an Oscar. They are also featured in the movie Middle Man and just wrapped production on the upcoming feature film, God Save The Queens in which Kelly is the lead in. TV: Guest-starred on numerous shows, including Lucifer, Modern Family, Curb Your Enthusiasm, CSI, The New Normal, New Adventures of Old Christine, Judging Amy, Nip/Tuck, Will & Grace, George Lopez. Recurring: NYPD Blue. Featured in LOGO’s comedy special DragTastic NYC, and a very small co-star role on Season Six of RuPaul's Drag Race. Stage: Kelly has starred in more than 50 plays. They wrote and starred in their critically acclaimed solo show,The Confusion of My Illusion, at the Los Angeles LGBT Center. As a singer, songwriter, and musician, Kelly has released four critically acclaimed albums and is currently working on their fourth. Kelly grew up in Oklahoma like their uncle, the late great Mickey Mantle. (Yep...Kelly's a switch-hitter, too.) Kelly received a B.F.A. in Theatre from the University of Oklahoma and is a graduate of Second City in Chicago. https://www.instagram.com/kellymantle • https://www.imdb.com/name/nm0544141/ ALEXANDRA BILLINGS is an actress, teacher, singer, and activist. -

Hunting and Social Change in Late Saxon England
Eastern Illinois University The Keep Masters Theses Student Theses & Publications 2016 Butchered Bones, Carved Stones: Hunting and Social Change in Late Saxon England Shawn Hale Eastern Illinois University This research is a product of the graduate program in History at Eastern Illinois University. Find out more about the program. Recommended Citation Hale, Shawn, "Butchered Bones, Carved Stones: Hunting and Social Change in Late Saxon England" (2016). Masters Theses. 2418. https://thekeep.eiu.edu/theses/2418 This is brought to you for free and open access by the Student Theses & Publications at The Keep. It has been accepted for inclusion in Masters Theses by an authorized administrator of The Keep. For more information, please contact [email protected]. The Graduate School� EASTERNILLINOIS UNIVERSITY " Thesis Maintenance and Reproduction Certificate FOR: Graduate Candidates Completing Theses in Partial Fulfillment of the Degree Graduate Faculty Advisors Directing the Theses RE: Preservation, Reproduction, and Distribution of Thesis Research Preserving, reproducing, and distributing thesis research is an important part of Booth Library's responsibility to provide access to scholarship. In order to further this goal, Booth Library makes all graduate theses completed as part of a degree program at Eastern Illinois University available for personal study, research, and other not-for-profit educational purposes. Under 17 U.S.C. § 108, the library may reproduce and distribute a copy without infringing on copyright; however, professional courtesy dictates that permission be requested from the author before doing so. Your signatures affirm the following: • The graduate candidate is the author of this thesis. • The graduate candidate retains the copyright and intellectual property rights associated with the original research, creative activity, and intellectual or artistic content of the thesis. -

Bones As Evidence of Meat Production and Distribution in York
This is a repository copy of Bones as evidence of meat production and distribution in York. White Rose Research Online URL for this paper: https://eprints.whiterose.ac.uk/1168/ Book Section: O'Connor, T.P. (2000) Bones as evidence of meat production and distribution in York. In: White, E., (ed.) Feeding a city: York. The provision of food from Roman times to the beginning of the twentieth century. Prospect Books , Devon, UK , pp. 43-60. Reuse Items deposited in White Rose Research Online are protected by copyright, with all rights reserved unless indicated otherwise. They may be downloaded and/or printed for private study, or other acts as permitted by national copyright laws. The publisher or other rights holders may allow further reproduction and re-use of the full text version. This is indicated by the licence information on the White Rose Research Online record for the item. Takedown If you consider content in White Rose Research Online to be in breach of UK law, please notify us by emailing [email protected] including the URL of the record and the reason for the withdrawal request. [email protected] https://eprints.whiterose.ac.uk/ CHAPTER TWO BONESAS EVIDENCEOF MFATPRODUCTION AND DISTRIBUTIONIN YORK Boms - THEIR STRENGTHSAND WEAKNESSES any books and papers have been wrirren on the general principles and minutiae of using the animal bones recovered from Marchaeological deposits as a source of information on past diet.'",-3 A 1511discussion of merhodoIogical issues is beyond the remit of this chapter, but. it is worth reminding ourselves that there are many stages berween an animal being killed and used for food, and a pile of bones arriving on rhe bench. -

Curiosity Guide #306 Skeletal System
Curiosity Guide #306 Skeletal System Accompanies Curious Crew, Season 3, Episode 6 (#306) Calcium-Rich Bones Investigation #6 Description Explore the role of calcium in making strong bones. Materials 6 chicken bones 6 containers Calcium tablets Vinegar Procedure 1: Prepare the bones 1) Boil the bones to remove any meat. 2) Soak the bones in 1 part bleach to ten parts water for five minutes. 3) Let the bones dry. Procedure 2: Investigate 1) Place one chicken bone in each of the 6 glasses. 2) Pour vinegar over each bone. 3) Do not add any calcium to the first container. 4) In the second container, add 300 milligrams of calcium. 5) In the third container, add 600 mg calcium, 1,200 mg in the fourth, 1,800 mg in the fifth, and 2,400 mg in the sixth. 6) Leave the bones for 5 days. 7) Compare the results. 8) Drop a calcium tablet into a cup of vinegar. How does it react? My Results Explanation In addition to calcium, bones also contain phosphorous. However, it is the calcium salts that make bones rigid. Acids such as vinegar can dissolve those calcium salts and leave the bone soft and rubbery. In this experiment, the more calcium that was in the container, the stronger the bones remained. Because the mineral calcium provides rigidity to the bones, it is important to eat calcium rich foods like low fat dairy; green, leafy vegetables like collard greens; beans; and nuts. A person between the ages of 11 and 24 should consume 1,200 milligrams of calcium every day. -

Vehicle Acquisition
VEHICLE ACQUISITION F ederal Transit Administration Americans with Disabilities Act Circular C 4710.1 Draft Chapter for Public Comment October 2012 TABLE OF CONTENTS 1 INTRODUCTION 1 1.1 THE DOT ADA REGULATIONS 1 1.2 PROVIDING SERVICE ON BEHALF OF ANOTHER ENTITY: “STAND IN THE SHOES” 1 2 ACQUISITION REQUIREMENTS FOR PUBLIC ENTITIES 3 2.1 BUSES AND VANS 4 2.2 RAPID RAIL AND LIGHT RAIL 5 2.3 COMMUTER RAIL 6 2.4 OTHER CONSIDERATIONS 7 2.5 DEMAND RESPONSIVE SERVICE 8 3 THE MAIN ELEMENTS OF ACCESSIBLE VEHICLES 10 3.1 BUSES AND VANS 13 3.2 RAPID RAIL VEHICLES 17 3.3 LIGHT RAIL VEHICLES 18 3.4 COMMUTER RAIL CARS 21 3.5 OTHER CONSIDERATIONS 23 4 ENSURING THAT VEHICLES ARE COMPLIANT 24 4.1 UNDERSTANDING THE SPECIFICATIONS 24 4.2 OBTAINING PUBLIC INPUT 24 4.3 ADDITIONAL SPECIFICATIONS 25 4.4 INSPECTIONS 25 5 DEFINITIONS 26 6 AUTHORITIES 28 7 REFERENCES 29 APPENDICES APPENDIX 1 SAMPLE BUS AND VAN SPECIFICATION CHECKLIST !"#$#%#$&'()*+,($$ -./')+.$#)0*'1'2'34$&/,52.($6$%(,72$ 8)239.($:;<:$ =,>.$<$37$:? ! 1 INTRODUCTION This Circular chapter on vehicle acquisition serves as a reference document for public transportation providers acquiring vehicles to ensure that these vehicles meet the requirements of the U.S. Department of Transportation (DOT) Americans with Disabilities Act (ADA) regulations. It is the goal of the Federal Transit Administration (FTA) to help transportation providers meet their obligations under the ADA by outlining the regulations, describing effective practices, and presenting the information in an easy-to-use format. Please note that this Circular does not alter, amend, or otherwise affect the DOT ADA regulations themselves; transportation providers are advised to use this Circular in addition to (not in lieu of) the DOT ADA regulations. -

Battery Powered Wheelchair and Mobility Aid Guidance Document
Battery Powered Wheelchair and SafetyMobility requirements applicableAid toGuidance the carriage of battery powered Document wheelchairs and mobility aids when carried by passengers travelling by air Based on the 2019 Regulation compliance with the IATA Dangerous Goods Introduction Regulations. This document is based on the provisions set out in Passengers may only travel with a battery-powered the 2019-2020 Edition of the International Civil mobility aid with the airline’s approval. Proper pre- Aviation Organization (ICAO) Technical Instruction notification by the user helps to ensure that: for the Safe Transport of Dangerous Goods by Air (Technical Instructions) and the 60th Edition of the ▪ all in the transportation chain know what IATA Dangerous Goods Regulations (DGR). device(s) and battery type(s) they are transporting; Information on the DGR can be found here: ▪ how to properly load and handle them; and https://www.iata.org/publications/dgr/Pages/index. ▪ what to do if an incident or accident occurs aspx either in-flight or on the ground. The batteries that power wheelchairs and mobility The pilot-in-command must be informed of the aids are considered dangerous goods when carried location of the mobility aid with installed batteries, by air. These and some other dangerous goods that removed batteries and spare batteries, to best deal are permitted for carriage by passengers can be with any emergencies that may occur. transported safely by air provided certain safety requirements are met. The requirements are Inadvertent operation of battery powered mobility detailed in the IATA Dangerous Goods Regulations, aids can cause friction or electrical load which which are based on the ICAO Technical could lead to a fire. -
2017 Ada Update on Service Animal Rules
2017 ADA UPDATE ON SERVICE ANIMAL RULES The California Hotel & Lodging Association receives many questions regarding the rights and obligations of lodging establishments with respect to service animals. This document contains CHLA’s updated discussion of this topic. First, there has been a significant change regarding California law related to service animals. This change, which is discussed below, will make it easier for lodging operators to deal with guests who claim that their pets are service animals. Here are the basics of California law as it relates to service animals: • There was a time when the California Department of Fair Employment and Housing, which administers California’s Fair Employment and Housing Act (Act), took the position that the Act applied to the lodging industry. At that time, there was concern that lodging operators would have to comply with the more stringent requirements of the Act: (1) it is not limited to dogs— depending on the circumstances, the FEHA protects other types of animals and treats them as service animals; and (2) it provides protections for people who use “comfort” and “companion” animals. Contrary to the Department’s earlier position, however, CHLA was recently advised that the Act only applies to homes, condos, and apartments, and that it does not apply to hotels! • It is important for lodging operators to bear in mind that although the 2011 revisions to the ADA rules regarding service animals expressly state that (1) only dogs qualify as service animals,1 and that (2) “comfort” and “companion” dogs are not service animals,2 if a local jurisdiction in California has broader, more stringent rules than the ADA, the local rules must be complied with. -

Download Bare Bones, Kathy Reichs, Random House, 1999
Bare Bones, Kathy Reichs, Random House, 1999, , . DOWNLOAD http://archbd.net/17PVC8q Bones are Forever , Kathy Reichs, 2013, Fiction, 414 pages. The gripping new Temperance Brennan novel from the world class forensic anthropologist and Number 1 bestselling author.A newborn baby is found wedged in a vanity cabinet in a .... The Law of Betrayal , Tess Collins, Jun 30, 2006, Fiction, 292 pages. When she was ten years old Alma's father disappeared. The only man who knows the true story is brutally killed, but she must defend herself against an accusation of murder.. Break No Bones A Novel, Kathy Reichs, Jul 11, 2006, Fiction, 352 pages. Following the tremendous success of Cross Bones, Kathy Reichs explores another high-profile topic in Break No Bones -- a case that lands forensic anthropologist Temperance .... Bones Buried Deep, Max Allan Collins, Kathy Reichs, Feb 28, 2006, Fiction, 304 pages. Forensic anthropologist Dr. Termperance Brennan is called in by Special Agent Seeley Booth to assist in the investigation into a bag of skeletal remains, complete with note .... Cross Bones , Kathy Reichs, May 23, 2006, Fiction, 496 pages. Receiving mysterious clues about a shooting murder in Montreal, Tempe Brennan wonders if the victim may have been a Jewish black market antiquities trader and teams up with .... Deadly Decisions A Novel, Kathy Reichs, Aug 8, 2000, Fiction, 336 pages. Nobody tells a chilling story like international bestselling author Kathy Reichs, whose "most valuable tool is her expertise...she's the real thing" (New York Newsday). Drawing .... Corpi freddi La serie di Temperance Brennan #1, Kathy Reichs, , Fiction, 362 pages. -

Relationship Between Body Image and Physical Functioning Following Rehabilitation for Lower-Limb Amputation
Western University Scholarship@Western Physical Therapy Publications Physical Therapy School 2019 Relationship between body image and physical functioning following rehabilitation for lower-limb amputation Jessica Desrochers Courtney Frengopoulos Michael W.C. Payne Ricardo Viana Susan W. Hunter Follow this and additional works at: https://ir.lib.uwo.ca/ptpub Part of the Physical Therapy Commons Relationship between body image and physical functioning following rehabilitation for lower limb amputation Jessica Desrochers BHSc1; Courtney Frengopoulos MSc2; Michael WC Payne MD3; Ricardo Viana MD3; Susan W Hunter PhD3,4 1. School of Health Studies, University of Western Ontario, London, ON; 2. Faculty of Health & Rehabilitation Sciences, University of Western Ontario, London, ON; 3. Department of Physical Medicine & Rehabilitation, Schulich School of Medicine and Dentistry, University of Western Ontario, London, ON; 4. School of Physical Therapy, University of Western Ontario, London, ON. Running title: Body image and mobility in lower extremity amputees Corresponding author: Dr. Susan W Hunter University of Western Ontario School of Physical Therapy Room 1588, Elborn College 1201 Western Road, London, Ontario Email: [email protected] Telephone: 519-661-2111 ext88845 Funding: This work was supported by the St. Joseph’s Foundation Cognitive Vitality and Brain Health Seed Funding Opportunity. The funding body had no involvement in the conduct of the study. Conflict of interest: None to report. Relationship between body image and physical functioning following rehabilitation for lower limb amputation ABSTRACT Objectives: To evaluate change in body image and the association between body image at discharge and mobility 4 months post rehabilitation. Methods: Prospective cohort of consecutive admissions to inpatient prosthetic rehabilitation. -

The Economics of Enhancing Accessibility Estimating the Benefits and Costs of Participation
The Economics of Enhancing Accessibility Estimating the Benefits and Costs of Participation Discussion01 Paper 2017 • 01 Bridget R.D. Burdett TDG Ltd, Hamilton, New Zealand Stuart M. Locke University of Waikato Management School, Hamilton, New Zealand Frank Scrimgeour Institute for Business Research, University of Waikato, Hamilton, New Zealand The Economics of Enhancing Accessibility Estimating the Benefits and Costs of Participation Discussion Paper No. 2017-01 Prepared for the Roundtable on Economics of Accessible Transport 3-4 March 2016, Paris Bridget R.D. Burdett TDG Ltd, Hamilton, New Zealand Stuart M. Locke Department of Finance, University of Waikato Management School, Hamilton, New Zealand Frank Scrimgeour Institute for Business Research, University of Waikato, Hamilton, New Zealand February 2017 The International Transport Forum The International Transport Forum is an intergovernmental organisation with 57 member countries. It acts as a think tank for transport policy and organises the Annual Summit of transport ministers. ITF is the only global body that covers all transport modes. The ITF is politically autonomous and administratively integrated with the OECD. The ITF works for transport policies that improve peoples’ lives. Our mission is to foster a deeper understanding of the role of transport in economic growth, environmental sustainability and social inclusion and to raise the public profile of transport policy. The ITF organises global dialogue for better transport. We act as a platform for discussion and pre- negotiation of policy issues across all transport modes. We analyse trends, share knowledge and promote exchange among transport decision-makers and civil society. The ITF’s Annual Summit is the world’s largest gathering of transport ministers and the leading global platform for dialogue on transport policy.