Do You Have Work-Related Asthma?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Caring for Children with Special Needs ALLERGIES and ASTHMA
caring for children with special needs ALLERGIES AND ASTHMA We don’t usually think of children with allergies or asthma as children with “special needs,” but they certainly are. In fact, children with these conditions are probably the most frequently encountered “special needs” children. Child care providers can do a great deal to help individual children manage their specific allergy or asthma needs and feel more comfortable in a child care setting. Allergies wastes. Every house has them, no matter how clean. Other inhaled Children with allergies face the allergens include mold, pollen (hay same social difficulties as do adults, fever), animal dander (especially but they have less maturity and from cats), chemicals, and per emotional resources to deal with fumes. them. Children find that they cannot eat what their friends eat or The most common allergy symp cannot play outside during some toms are seasons. Until a child is mature � a clear, runny nose and enough to understand why she sneezing, cannot do something, you must be � itchy or stuffed-up nose or careful to help the child through the itchy, runny eyes, and difficulties. Start teaching a child early on about what he is allergic to; � asthma (remember that not all you will not always be able to people with asthma have monitor everything. allergies and not all allergies Some foods can cause a life cause or develop into asthma). threatening reaction. The mouth, throat, and bronchial tubes swell enough to interfere with breathing. Strategies for inclusion The person may wheeze or faint. Some parents have found that by Often there are generalized hives volunteering to bring food to and/or a swollen face. -

Symptoms Related to Asthma and Chronic Bronchitis in Three Areas of Sweden
Eur Respir J, 1994, 7, 2146–2153 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07122146 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Symptoms related to asthma and chronic bronchitis in three areas of Sweden E. Björnsson*, P. Plaschke**, E. Norrman+, C. Janson*, B. Lundbäck+, A. Rosenhall+, N. Lindholm**, L. Rosenhall+, E. Berglund++, G. Boman* Symptoms related to asthma and chronic bronchitis in three areas of Sweden. E. Björnsson, *Dept of Lung Medicine and Asthma P. Plaschke, E. Norrman, C. Janson, B. Lundbäck, A. Rosenhall, N. Lindholm, L. Research Center, Akademiska sjukhu- Rosenhall, E. Berglund, G. Boman. ERS Journals Ltd 1994. set, Uppsala University, Uppsala, Sweden. ABSTRACT: Does the prevalence of respiratory symptoms differ between regions? **Asthma and Allergy Research Center, Sahlgren's Hospital, University of Göteborg, As a part of the European Community Respiratory Health Survey, we present data Göteborg, Sweden. +Dept of Pulmonary from an international questionnaire on asthma symptoms occurring during a 12 Medicine and Allergology, Univer- month period, smoking and symptoms of chronic bronchitis. The questionnaire was sity Hospital of Northern Sweden, Umeå, mailed to 10,800 persons aged 20–44 yrs living in three regions of Sweden (Västerbotten, Sweden. ++Dept of Pulmonary Medicine, Uppsala and Göteborg) with different environmental characteristics. The total Sahlgrenska University Hospital, Göteborg, response rate was 86%. Sweden. Wheezing was reported by 20.5%, and the combination of wheezing without a Correspondence: E. Björnsson, Dept of cold and wheezing with breathlessness by 7.4%. The use of asthma medication was Lung Medicine, Akademiska sjukhuset, S- reported by 5.3%. -

Occupational Airborne Particulates
Environmental Burden of Disease Series, No. 7 Occupational airborne particulates Assessing the environmental burden of disease at national and local levels Tim Driscoll Kyle Steenland Deborah Imel Nelson James Leigh Series Editors Annette Prüss-Üstün, Diarmid Campbell-Lendrum, Carlos Corvalán, Alistair Woodward World Health Organization Protection of the Human Environment Geneva 2004 WHO Library Cataloguing-in-Publication Data Occupational airborne particulates : assessing the environmental burden of disease at national and local levels / Tim Driscoll … [et al.]. (Environmental burden of disease series / series editors: Annette Prüss-Ustun ... [et al.] ; no. 7) 1.Dust - adverse effects 2.Occupational exposure 3.Asthma - chemically induced 4.Pulmonary disease, Chronic obstructive - chemically induced 5.Pneumoconiosis - etiology 6.Cost of illness 7.Epidemiologic studies 8.Risk assessment - methods 9.Manuals I.Driscoll, Tim. II.Prüss-Üstün, Annette. III.Series. ISBN 92 4 159186 2 (NLM classification: WA 450) ISSN 1728-1652 Suggested Citation Tim Driscoll, et al. Occupational airborne particulates: assessing the environmental burden of disease at national and local levels. Geneva, World Health Organization, 2004. (Environmental Burden of Disease Series, No. 7). © World Health Organization 2004 All rights reserved. Publications of the World Health Organization can be obtained from Marketing and Dissemination, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). -

Dust Exposure and Byssinosis Among Cotton Textile Workers in Dar Es Salaam, Tanzania
MOJ Public Health Research Article Open Access Dust exposure and byssinosis among cotton textile workers in Dar es salaam, Tanzania Abstract Volume 9 Issue 6 - 2020 Background: Cotton dust exposure increases the risk of developing lung diseases including Luco P Mwelange, Simon Mamuya, Gloria Byssinosis. The prevalence of byssinosis is more in developing countries compare to developed countries. For the past forty years there are little information known about the Sakwari, Witness John Axwesso Department of Environmental and Occupational Health, prevalence of byssinosis and its associated risk factors among textile workers in Tanzania. Muhimbili University of Health and Allied Sciences, Tanzania Objective: The study aimed to assess dust exposure and associated risk factors among textile workers, in Dar es Salaam, Tanzania. Correspondence: Luco P Mwelange, Muhimbili University of Health and Allied Sciences, Tanzania, Tel+255655049524, Material and methods: The study design was descriptive cross sectional study conducted Email from March to August 2019. Stratified sampling technique was used to obtain 325 participants (exposed 164 and control 161) respectively. A modified British Medical Received: October 29, 2020 | Published: November 30, 2020 Research Council (BMRC) questionnaire and Side Kick Casella Pump were used for data collection. Data were analyzed using Statistical Package for Social Science software 23 versions. Chi square test and Binary logistic regression were performed to check for association. A 95% confidence Interval with a significance expressed in P˂0.05 was used. Results: Prevalence of byssinosis in the exposed group was 18.9% and 6.2% in the control group. Respiratory symptoms such as Coughing more days in three consecutive months (P˂0.001), wheezing (P˂0.02), dyspnoea I (P˂0.03), dyspnoea II (P˂0.007), and dyspnoea III (P˂0.002), were higher among exposed group compare to control group and the differences were statistically significant. -
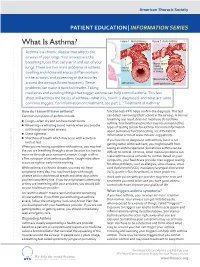
What Is Asthma? Figure 1
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Asthma? Figure 1. Normal Airway Figure 2. Acute Asthma Asthma is a chronic disease that affects the airways of your lungs. Your airways are the breathing tubes that carry air in and out of your Muscle spasm causing lungs. There are two main problems in asthma: relaxed narrowing muscles swelling and increased mucus (inflammation) of airways in the airways, and squeezing of the muscles Mucus build up around the airways (bronchospasm). These open airways Swelling/inammation problems can make it hard to breathe. Taking medicines and avoiding things that trigger asthma can help control asthma. This fact sheet will address the basics of asthma—what it is, how it is diagnosed, and what are some common triggers. For information on treatment, see part 2, “Treatment of Asthma”. How do I know if I have asthma? function test–PFT) helps confirm the diagnosis. This test Common symptoms of asthma include: can detect narrowing (obstruction) in the airways. A normal breathing test result does not mean you do not have ■ Cough—often dry and can have harsh bursts asthma. Your healthcare provider may recommend other ■ Wheezing—a whistling sound mainly when you breathe types of testing to look for asthma. For more information out through narrowed airways about pulmonary function testing, see ATS Patient ■ Chest tightness Information series at www.thoracic.org/patients. ■ Shortness of breath which may occur with activity or If you have been diagnosed with asthma, but it is not even at rest getting better with treatment, you might benefit from When you are having a problem with asthma, you may feel CLIP AND COPY AND CLIP seeing an asthma specialist. -

Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation
Allergic Bronchopulmonary Aspergillosis and Severe Asthma with Fungal Sensitisation Dr Rohit Bazaz National Aspergillosis Centre, UK Manchester University NHS Foundation Trust/University of Manchester ~ ABPA -a41'1 Severe asthma wl'th funga I Siens itisat i on Subacute IA Chronic pulmonary aspergillosjs Simp 1Ie a:spe rgmoma As r§i · bronchitis I ram une dysfu net Ion Lun· damage Immu11e hypce ractivitv Figure 1 In t@rarctfo n of Aspergillus Vliith host. ABP A, aHerg tc broncho pu~ mo na my as µe rgi ~fos lis; IA, i nvas we as ?@rgiH os 5. MANCHl·.'>I ER J:-\2 I Kosmidis, Denning . Thorax 2015;70:270–277. doi:10.1136/thoraxjnl-2014-206291 Allergic Fungal Airway Disease Phenotypes I[ Asthma AAFS SAFS ABPA-S AAFS-asthma associated with fu ngaIsensitization SAFS-severe asthma with funga l sensitization ABPA-S-seropositive a llergic bronchopulmonary aspergi ll osis AB PA-CB-all ergic bronchopulmonary aspergi ll osis with central bronchiectasis Agarwal R, CurrAlfergy Asthma Rep 2011;11:403 Woolnough K et a l, Curr Opin Pulm Med 2015;21:39 9 Stanford Lucile Packard ~ Children's. Health Children's. Hospital CJ Scanford l MEDICINE Stanford MANCHl·.'>I ER J:-\2 I Aspergi 11 us Sensitisation • Skin testing/specific lgE • Surface hydroph,obins - RodA • 30% of patients with asthma • 13% p.atients with COPD • 65% patients with CF MANCHl·.'>I ER J:-\2 I Alternar1a• ABPA •· .ABPA is an exagg·erated response ofthe imm1une system1 to AspergUlus • Com1pUcatio n of asthm1a and cystic f ibrosis (rarell·y TH2 driven COPD o r no identif ied p1 rior resp1 iratory d isease) • ABPA as a comp1 Ucation of asth ma affects around 2.5% of adullts. -

Diseases of the Respiratory System (J00-J99) ICD-10-CM
Diseases of the Respiratory System (J00-J99) ICD-10-CM Coverage provided by Amerigroup Inc. This publication contains proprietary information. This material is for informational purposes only. Reference the Centers for Medicare and Medicaid Services (CMS) for more information on Risk Adjustment and the CMS-HCC Model. Redistribution or other use is strictly forbidden This publication is for informational purposes only and is not guaranteed to be without defect. Please reference the current version(s) of the ICD-10-CM codebook, CMS-HCC Risk Adjustment Model, and AHA Coding Clinic for complete code sets and official coding guidance. AGPCARE-0080-19 63321MUPENABS 10/05/16 Diseases of the respiratory system are located in chapter Intermittent asthma which is defined as less 10 of the ICD-10-CM code book; this chapter includes than or equal to two occurrences per week. conditions such as asthma, pneumonia, and chronic Persistent asthma which includes three levels obstructive pulmonary disease (COPD). of severity: Mild: more than two times per week Reporting respiratory conditions Moderate: daily and may restrict Codes for reporting diseases of the respiratory physical activity system in ICD-10-CM feature relatively minor Severe: throughout the day with changes from ICD-9-CM. Most of the changes recurrent severe attacks limiting the involve understanding the medical terminology that ability to breathe the more specific codes include, as well as, the new The fourth character indicates severity, and the general coding structure and rules. fifth identifies whether status asthmaticus or At the beginning of chapter 10 for “Diseases of exacerbation is present. the Respiratory System (J00-J99),” an instructional note states, “When a respiratory condition is Asthma ICD-10-CM description described as occurring in more than one site and Category J45 Asthma is not specifically indexed, it should be classified Includes: to the lower anatomic site.” For example, Allergic: tracheobronchitis is classified to bronchitis with Asthma code J40. -

Occupational Lung Diseases
24 Occupational lung diseases Introduction i Occupational diseases are often thought to be Key points uniquely and specifically related to factors in the work environment; examples of such diseases are • Systematic under-reporting and the pneumoconioses. However, in addition to other difficulties in attributing causation both contribute to underappreciation of the factors (usually related to lifestyle), occupational burden of occupational respiratory exposures also contribute to the development or diseases. worsening of common respiratory diseases, such • Work-related exposures are estimated as chronic obstructive pulmonary disease (COPD), to account for about 15% of all adult asthma and lung cancer. asthma cases. • Boththe accumulation of toxic dust in the Information about the occurrence of occupational lungs and immunological sensitisation respiratory diseases and their contribution to to inhaled occupational agents can morbidity and mortality in the general population is cause interstitial lung disease. provided by different sources of varying quality. Some • Despite asbestos use being phased European countries do not register occupational out, mesothelioma rates are forecast diseases and in these countries, information about to continue rising owing to the long latency of the disease. the burden of such diseases is completely absent. • The emergence of novel occupational In others, registration is limited to cases where causes of respiratory disease in compensation is awarded, which have to fulfil specific recent years emphasises the need for administrative or legal criteria as well as strict continuing vigilance. medical criteria; this leads to biased information and underestimation of the real prevalence. Under- reporting of occupational disease is most likely to occur in older patients who are no longer at work but whose condition may well be due to their previous job. -

Allergic Bronchopulmonary Aspergillosis: a Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2
Review Allergy Asthma Immunol Res. 2016 July;8(4):282-297. http://dx.doi.org/10.4168/aair.2016.8.4.282 pISSN 2092-7355 • eISSN 2092-7363 Allergic Bronchopulmonary Aspergillosis: A Perplexing Clinical Entity Ashok Shah,1* Chandramani Panjabi2 1Department of Pulmonary Medicine, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi, India 2Department of Respiratory Medicine, Mata Chanan Devi Hospital, New Delhi, India This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. In susceptible individuals, inhalation of Aspergillus spores can affect the respiratory tract in many ways. These spores get trapped in the viscid spu- tum of asthmatic subjects which triggers a cascade of inflammatory reactions that can result in Aspergillus-induced asthma, allergic bronchopulmo- nary aspergillosis (ABPA), and allergic Aspergillus sinusitis (AAS). An immunologically mediated disease, ABPA, occurs predominantly in patients with asthma and cystic fibrosis (CF). A set of criteria, which is still evolving, is required for diagnosis. Imaging plays a compelling role in the diagno- sis and monitoring of the disease. Demonstration of central bronchiectasis with normal tapering bronchi is still considered pathognomonic in pa- tients without CF. Elevated serum IgE levels and Aspergillus-specific IgE and/or IgG are also vital for the diagnosis. Mucoid impaction occurring in the paranasal sinuses results in AAS, which also requires a set of diagnostic criteria. Demonstration of fungal elements in sinus material is the hall- mark of AAS. -

08-0205: N.M. and DEPARTMENT of the NAVY, PUGET S
United States Department of Labor Employees’ Compensation Appeals Board __________________________________________ ) N.M., Appellant ) ) and ) Docket No. 08-205 ) Issued: September 2, 2008 DEPARTMENT OF THE NAVY, PUGET ) SOUND NAVAL SHIPYARD, Bremerton, WA, ) Employer ) __________________________________________ ) Appearances: Oral Argument July 16, 2008 John Eiler Goodwin, Esq., for the appellant No appearance, for the Director DECISION AND ORDER Before: DAVID S. GERSON, Judge COLLEEN DUFFY KIKO, Judge JAMES A. HAYNES, Alternate Judge JURISDICTION On October 30, 2007 appellant filed a timely appeal from a November 17, 2006 decision of the Office of Workers’ Compensation Programs denying his occupational disease claim. Pursuant to 20 C.F.R. §§ 501.2(c) and 501.3, the Board has jurisdiction over the merits of the claim. ISSUE The issue is whether appellant has established that he sustained occupational asthma in the performance of duty due to accepted workplace exposures. On appeal, he, through his attorney, asserts that the Office did not provide Dr. William C. Stewart, the impartial medical examiner, with a complete, accurate statement of accepted facts. FACTUAL HISTORY On December 8, 2004 appellant, then a 57-year-old insulator, filed an occupational disease claim (Form CA-2) asserting that he sustained occupational asthma and increasing shortness of breath due to workplace exposures to fiberglass, silicates, welding smoke, polychlorobenzenes, rubber, dusts, gases, fumes and smoke from “burning out” submarines from 1991 through January -
Right Heart Pressures in Bronchial Asthma
Thorax: first published as 10.1136/thx.26.1.39 on 1 January 1971. Downloaded from Thorax (1971), 26, 39. Right heart pressures in bronchial asthma R. F. GUNSTONE St. George's Hospital, London S.W.1 Right heart pressures, electrocardiograms, blood gases, and peak expiratory flow rates were measured in nine patients admitted to hospital with severe bronchial asthma. Low or normal right heart pressures were found despite electrocardiographic changes in five patients consisting of right atrial P waves, abnormal right axis deviation, and in one patient T-wave changes in pre- cordial leads. These electrocardiographic changes reverted towards normal on recovery of the patient from the asthmatic attack. Electrocardiographic changes suggestive of right The procedure was carried out in the general ward heart embarrassment have been noted in acute with the patient in the sitting position supported at 60 bronchial asthma, particularly right atrial P waves to 90 degrees to the horizontal because orthopnoea (P and abnormal right axis deviation was always present. Immediately after catheterization pulmonale) the peak expiratory flow rate was measured with a (Harkavy and Romanoff, 1942; Miyamato, Wright peak flow meter (Wright and McKerrow, Bastaroli, and Hoffman, 1961; Ambiavagar, 1959) and blood (capillary or arterial) was taken for Jones and Roberts, 1967). These observations measurement of pH, Pco2, and standard bicarbonate raise the possibility that death in bronchial asthma by the Astrup method (Astrup, J0rgensen, Andersen, may be due to acute cor pulmonale although and Engel, 1960). The peak flow rate and electro- copyright. necropsy evidence is against this suggestion (Earle, cardiogram were repeated after recovery. -

National Occupational Research Agenda (Nora)
NATIONAL OCCUPATIONAL RESEARCH AGENDA (NORA) NATIONAL OCCUPATIONAL RESEARCH AGENDA FOR HEALTHCARE AND SOCIAL ASSISTANCE (HCSA) February 2019 Developed by the NORA HCSA Council 1 . For more information about the National Occupational Research Agenda (NORA), visit the web site: https://www.cdc.gov/niosh/nora/ For monthly updates on NORA, subscribe to NIOSH eNews at www.cdc.gov/niosh/eNews Disclaimer This is a product of the National Occupational Research Agenda (NORA) Healthcare and Social Assistance Sector Council. It does not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, or U.S. Department of Health and Human Services. 2 INTRODUCTION What is the National Occupational Research Agenda? The National Occupational Research Agenda (NORA) is a partnership program to stimulate innovative research and workplace interventions. In combination with other initiatives, the products of this program are expected to reduce the occurrence of injuries and illnesses at work. Unveiled in 1996, NORA has become a research framework for the Nation and the National Institute for Occupational Safety and Health (NIOSH). Diverse parties collaborate to identify the most critical issues in workplace safety and health and develop research objectives for addressing those needs. NORA enters its third decade in 2016 with an enhanced structure. The ten sectors formed for the second decade will continue to prioritize occupational safety and health research by major areas of the U.S. economy. In addition, there are seven cross-sectors organized according the major health and safety issues affecting the U.S. working population. While NIOSH is serving as the steward to move this effort forward, it is truly a national effort.