Cleistanthus Collinus Poisoning
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Interactions of Some Commonly Used Drugs in Dermatology
Table Drug interactions of some commonly used drugs in dermatology M. J. Cyriac Department of Dermatology and Venereology, Medical College, Kottayam, India. Address for correspondence: Dr. M. J. Cyriac, Professor and Head, Department of Dermatology and Venereology, Medical College, Kottayam, India. E-mail: [email protected] Drug interactions leading to serious adverse effects are alternative medicines or food should also be borne in to be cautiously watched for when multiple drugs are mind.2 Increased risk of drug induced toxicity or used simultaneously.1 It is important for the physician therapeutic failure can occur when a new drug is added to be aware of these interactions. Although in many to a treatment regimen. It is impossible to remember instances the adverse interaction does not reach a all possible drug interactions. A ready to refer checklist magnitude of recognizable clinical expression, rarely is useful as a handy reference. it can result in a serious adverse outcome. Some of the commonly used drugs in dermatology and Adverse drug interactions may lead to increased their interactions, resultant clinical effect and possible toxicity, decreased efficacy or both. The possibility of underlying mechanisms are given in Table 1. Table 2 lists interaction with non-prescription drugs, herbal or the drugs with their relative risk for inducing interactions. Table 1: Drug interactions of some commonly used drugs Drug Interacting drug Adverse effect Remarks Erythromycin/Clarithromycin Theophylline Theophylline toxicity Precipitates -

DRI® Digoxin Assay
DRI® Digoxin Assay For In Vitro Diagnostic Use 1669 (25 mL, 8 mL Kit) 1669-A (25 mL, 8 mL Kit) Intended Use Reagent Preparation and Storage The DRI® Digoxin Assay is intended for the quantitative determination of digoxin in human The reagents are ready for use. No reagent preparation is required. All assay components, serum or plasma. when stored properly at 2-8°C, are stable until the expiration date indicated on the label. Summary and Explanation of the Test Specimen Collection and Handling Digitalis is known to have the ability to increase the force and velocity of myocardial Pharmacokinetic factors, such as dosage form, mode of administration, concomitant drug therapy contraction.1 Digoxin is one of the most commonly used forms of digitalis in the treatment as well as the patient’s clinical condition may influence the correct time of sample collection.2,3 For of congestive heart failure and arrhythmia such as atrial fibrillation and atrial flutter. The reliable interpretation of results, a serum specimen should be collected 6 to 8 hours following therapeutic range of digoxin is narrow. Futhermore, individual differences in drug absorption, the last oral dose of digoxin. Either serum or heparin and EDTA treated plasma samples can distribution, metabolism, and excretion as well as factors such as concurrent use of other drugs be used with the assay. Samples may be stored refrigerated at 2-8°C for up to 7 days or frozen and illness can also alter the serum concentration in response to a given dosage. Monitoring (-20°C) for up to 6 months. -

Report on the National Seminar on Radioimmunoassays Radiation Medicine Centre, B.A.R.C
REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16-20, 1978 RADIATION MEDICINE CENTRE, B.A.R.C. DEPARTMENT OF ATOMIC ENERGY AND WORLD HEALTH ORGANISATION REPORT ON THE NATIONAL SEMINAR ON RADIOIMMUNOASSAYS JANUARY 16—20, 1978 RADIATION MEDICINE CENTRE, BARC TATA MEMORIAL HOSPITAL ANNEXE JERBAI WADIA ROAD, PAREL BOMBAY 400 012 ORGANISED UNDER THE AUSPICES OF THE DEPARTMENT OF ATOMIC ENERGY & WORLD HEALTH ORGANISATION CONTENTS Page Preface .. .. .. .. .. .. .. 3 Administrative Responsibilities .. .. .. .. 6 List of Participants 7 Programme .. .. .. .. .. .. .. 11 Basic Requirements of RIA in India .. .. .. 14 a. Radioisotopes for RIA's .. .. .. .. .. 15 b. Kits for RIA 17 c. Availability of Antibodies 19 d. National Pituitary Agency .. .. .. .. 20 e. Well-counter for RIA 21 f. Radiation Protection Aspects of RIA 23 Review of Discussion following the Session .. .. 26 State of Art of RIA's in India 28 Trigger Sessions 36 a. Quality Control of RIA's 37 b. Usefulness and limitations of RIA's in clinical diagnosis 39 c. RIA's in tropical diseases •. .. .. .. .. 42 d. Centralised assay services .. .. .. .. 44 Recommendations and Guidelines .. .. .. .. 46 Backword 51 Bibliography . .. .. .. .. .. .. 53 PREFACE This National Seminar on Radioimmunoassays was the second National Seminar jointly sponsored by Department of Atomic Energy and World Health Organisation and organised at Radiation Medicine Centre. The first one on 'Nuclear Medicine in India' was held in December 1976. The present Seminar on Radioimmunoassays was distinguished by the participation of Dr. Rosalyn Yalow, Nobel Laureate in Medicine for 1977. She, along with Dr. Solomon A. Berson, discovered the technique of Radioimmunoassay and nurtured it through the early years with hard and meticulous work to establish its usefulness in medical science. -

Ethnobotanical Observations of Euphorbiaceae Species from Vidarbha Region, Maharashtra, India
Ethnobotanical Leaflets 14: 674-80, 2010. Ethnobotanical Observations of Euphorbiaceae Species from Vidarbha region, Maharashtra, India G. Phani Kumar* and Alka Chaturvedi# Defence Institute of High Altitude Research (DRDO), Leh-Ladakh, India #PGTD Botany, RTM Nagpur University, Nagpur, India *corresponding author: [email protected] Issued: 01 June, 2010 Abstract An attempt has been made to explore traditional medicinal knowledge of plant materials belonging to various genera of the Euphorbiaceae, readily available in Vidharbha region of Maharasthtra state. Ethnobotanical information were gathered through several visits, group discussions and cross checked with local medicine men. The study identified 7 species to cure skin diseases (such as itches, scabies); 5 species for antiseptic (including antibacterial); 4 species for diarrhoea; 3 species for dysentery, urinary infections, snake-bite and inflammations; 2 species for bone fracture/ dislocation, hair related problems, warts, fish poisons, night blindness, wounds/cuts/ burns, rheumatism, diabetes, jaundice, vomiting and insecticide; 1 species as laxative , viral fever and arthritis. The results are encouraging but thorough scientific scrutiny is absolutely necessary before being put into practice. Key words: Ethnopharmacology; Vidarbha region; Euphorbiaceae; ethnobotanical information. Introduction The medicinal properties of a plant are due to the presence of certain chemical constituents. These chemical constituents, responsible for the specific physiological action, in the plant, have in many cases been isolated, purified and identified as definite chemical compounds. Quite a large number of plants are known to be of medicinal use remain uninvestigated and this is particularly the case with the Indian flora. The use of plants in curing and healing is as old as man himself (Hedberg, 1987). -

Ex-Situ Conservation of Indigenous, Threatened and Ethno- Medicinal Diversity of Forest Species
International Journal of Bio-Science and Bio-Technology Vol.7, No.3 (2015), pp.9-22 http://dx.doi.org/10.14257/ijbsbt.2015.7.3.02 Ex-situ Conservation of Indigenous, Threatened and Ethno- Medicinal Diversity of Forest Species O.P. Chaubey, Archana Sharma and G. Krishnamurthy State Forest Research Institute, Jabalpur - 482008 (M.P.), India E-mail: [email protected] Abstract Madhya Pradesh is rich in plant wealth and endemic flora. As a part of conservation programme, institute has established an arboretum-cum-botanic garden in 1976, covering an area of 7.34 ha. The garden complex includes various sections situated in the campus and nursery. The main forest botanic garden is situated in 4.25 ha area and houses a wide array of forest flora including trees, shrubs, climbers and herbal plant species in various sections. Of the total species planted, over 50% were threatened and ascribed with conservation value. The garden was of scientific and educational utility. The institute provides diploma and degree courses in collaboration with Universities and colleges. The institute forest botanic garden has been registered under the network of Indian Botanic Gardens in 2005. It was one among the 140 Botanic gardens of India registered by Botanic Garden Conservation International under BGCI-Investing in Nature-India programme. Detailed online information was available on the IBGN website (http//www.ibgn.org). SFRI-BG is unique in terms of its scientific arrangement of plants. The species wise conservation status and uses pertaining to ethnic, medicinal and economic importance were described here. Keywords: Plant diversity, ethno-medicinal plants, conservation, threatened plants. -

Euphorbiaceae) in the Philippines
BLUMEA 44 (1999) 109-148 Revision of the genus Cleistanthus (Euphorbiaceae) in the Philippines Stefan Dressler 1 Rijksherbarium/Hortus Botanicus, P.O. Box 9514, 2300 RA Leiden, The Netherlands Summary The Philippine species of the euphorbiaceous genus Cleistanthus are revised. Sixteen species are recognised for this archipelago of which two are recorded from there for the first time. The oldest available combination from the Philippines [C. orgyalis (Blanco) Merr.] remains obscure and three collections from Palawan treated Three are tentatively as a separate taxon (C. spec. A). species are illustrated here and distribution maps for the Philippines are given for all species. Key words. Cleistanthus, Philippines, taxonomy. Introduction The genus Cleistanthus was established in 1848 by Planchon for a single species from West Tropical Africa using an unpublished name of J.D. Hooker. Before and after that several species were described affiliated to other (partly new) genera (e.g., Roxburgh, 1802; Hasskarl, 1855;Miquel, 1861; Thwaites, 1861, 1864; MiillerArgo- viensis, 1863) but MiillerArgoviensis (1866) soon clarified the taxonomy and made thenecessary new combinationsin his revision ofthe Euphorbiaceae for De Candolle's Prodromus. Later the genus was treated in some floras or regional revisions (e.g., Bentham, 1873; Hooker, 1887; Robinson, 1908). Jablonsky (1915) still represents the most recent complete generic treatment. With all its weaknesses his infrageneric classification is the one still adopted nowadays (cf. Shaw's various and indeed is determination Airy papers, see below) a handy tool. However, I consider it to be rather artificialin parts (e.g., sections based on indumentum of sepals, division of styles), but without having revised the full genus no other is pro- posed here. -
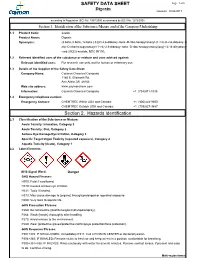
Digoxin SAFETY DATA SHEET Section 2. Hazards Identification
SAFETY DATA SHEET Page: 1 of 6 Digoxin Revision: 08/24/2017 according to Regulation (EC) No. 1907/2006 as amended by (EC) No. 1272/2008 Section 1. Identification of the Substance/Mixture and of the Company/Undertaking 1.1 Product Code: 22266 Product Name: Digoxin Synonyms: (3.beta.,5.beta.,12.beta.)-3-[(O-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl-(1->4)-O-2,6-dideoxy-.b eta.-D-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-D-ribo-hexopyranosyl)oxy]-12,14-dihydroxy- card-20(22)-enolide; NSC 95100; 1.2 Relevant identified uses of the substance or mixture and uses advised against: Relevant identified uses: For research use only, not for human or veterinary use. 1.3 Details of the Supplier of the Safety Data Sheet: Company Name: Cayman Chemical Company 1180 E. Ellsworth Rd. Ann Arbor, MI 48108 Web site address: www.caymanchem.com Information: Cayman Chemical Company +1 (734)971-3335 1.4 Emergency telephone number: Emergency Contact: CHEMTREC Within USA and Canada: +1 (800)424-9300 CHEMTREC Outside USA and Canada: +1 (703)527-3887 Section 2. Hazards Identification 2.1 Classification of the Substance or Mixture: Acute Toxicity: Inhalation, Category 3 Acute Toxicity: Oral, Category 2 Serious Eye Damage/Eye Irritation, Category 2 Specific Target Organ Toxicity (repeated exposure), Category 2 Aquatic Toxicity (Acute), Category 1 2.2 Label Elements: GHS Signal Word: Danger GHS Hazard Phrases: H300: Fatal if swallowed. H319: Causes serious eye irritation. H331: Toxic if inhaled. H373: May cause damage to {organs} through prolonged or repeated exposure. H400: Very toxic to aquatic life. -

Hypocalcemia in Cleistanthus Collinus Poisoning Iron and Zinc Deficiency
CORRESPONDENCE Hypocalcemia in Cleistanthus concentration of plant glycosides) and the delay in gastric lavage probably contributed to the death of the 2 girls [3]. collinus Poisoning The boy probably survived owing to decreased amount ingested. Apart from metabolic acidosis and hypokalemia, all three children had persistent hypocalcemia. The leaves of Cleistanthus collinus (CC) known as Hypercalciuria associated with distal renal tubular oduvanthazhai in Tamil language is a commonly acidosis probably contributed to the hypocalcemia. consumed plant poison in rural areas, usually with a However, urinary calcium excretion could not be suicidal intention. Distal renal tubular acidosis is known to documented. In addition to metabolic acidosis, occur with CC poisoning and hypokalemia is a risk factor hypocalcemia perhaps contributed to myocardial for mortality [1,2]. However, hypocalcemia in children dysfunction and mortality. In a child with CC poisoning, it with CC poisoning has not been documented. is prudent to watch for hypocalcemia and correct the same, if present. Two girls (12 years and 8 years of age) and their brother (9 years) were brought to our hospital with alleged C VENKATESH AND B ADHISIVAM history of consumption of 100-200 mL of boiled leaf Department of Pediatrics, extract of CC. Their mother had given them the poison Jawaharlal Institute of Post graduate before consuming herself due to a family dispute. They Medical Education and Research, developed vomiting, drowsiness and breathing difficulty Pondicherry 605 006, India. after an hour. Gastric lavage was done in a nearby hospital [email protected] after 4 hours of consumption and brought to JIPMER after REFERENCES 48 hours of ingestion. -

Digoxin Toxicity 1
Chronic Digoxin Toxicity Reviewers: Shawn M. Varney, Authors: Matthew Riddle, MD, Mel Otten, MD MD Target Audience: Emergency Medicine Residents (junior and senior level postgraduate learners), Medical Students Primary Learning Objectives: 1. Recognize signs and symptoms of digoxin toxicity 2. Order appropriate diagnostic studies for evaluation of digoxin toxicity 3. Appropriately interpret ECG 4. Administer digoxin-specific antibody fragments (DSFab) 5. Recognize acute kidney injury as a precipitating factor of toxicity, and treat acute kidney injury appropriately 6. Select an appropriate disposition for patient with digoxin toxicity Secondary Learning Objectives: detailed technical/behavioral goals, didactic points 1. Develop independent differential diagnosis in setting of leading information from the nurse 2. Describe the mechanism of digoxin toxicity and treatment, DSFab 3. Use appropriate dosing strategy for DSFab administration Critical actions checklist: 1. Order a basic metabolic panel 2. Order a digoxin level 3. Obtain ECG 4. Provide volume resuscitation for acute kidney injury 5. Administer digoxin antibody fragments 6. Consult Poison Center/Toxicologist 7. Admit to the MICU Environment: Emergency Department treatment area 1. Room Set Up – ED critical care area a. Manikin Set Up – Mid or high fidelity simulator b. Props – Standard ED equipment 2. Distractors – ED noise, alarming monitor For Examiner Only CASE SUMMARY SYNOPSIS OF HISTORY/ Scenario Background The setting is an urban emergency department. The patient is a 63-year-old male with a history of atrial fibrillation, HTN, and CHF brought to the emergency department by EMS for nausea and vomiting for the past four days and confusion that began shortly before arrival. PMHx: atrial fibrillation, HTN, and CHF PSHx: None Medications: ASA 81 mg once daily, Digoxin 250 mcg once daily, Amlodipine 10 mg once daily, Lasix 20 mg twice daily, warfarin 5 mg once daily Allergies: NKDA SocHx: smokes ½ ppd for 40 years. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Top Ten Potential Drug Interactions in Small Animal Medicine EJCAP 26(34 Autumn 2016 P 9
Top Ten Potential Drug Interactions in Small Animal Medicine EJCAP 26(34 Autumn 2016 P 9 Fecava lecture* Top Ten Potential Drug Interactions in Small Animal Medicine Jennifer M. Reinhart, Lauren A. Trepanier1 SUMMARY Today, comorbidities are increasingly diagnosed in veterinary patients and multiple drug combinations are common. However, as the number of administered drugs increases, so too does the risk for adverse drug interactions. Much of what is known about drug-drug interactions is taken from the human literature, but a growing body of work in veterinary medicine also exists. The purpose of this review is to summarize the current knowledge of potential drug interactions in humans and dogs for ten ‘at risk’ drugs used in small animal medicine: cimetidine, sucralfate, ketoconazole, fluoroquinolone antibiotics, omeprazole, phenobarbital, clomipramine, furosemide, metoclopramide, and cyclosporine. Increased awareness of these potential drug interactions will enhance therapeutic decision-making and improve the level of care for veterinary patients. Key words: drug-drug interaction, drug metabolism, adverse drug reaction, polypharmacy *This paper is based on the FECAVA lecture Cimetidine delivered at the 22nd EuroCongress in Vienna, Austria in June 2016. Eur J Comp An Pract Cimetidine, a histamine (H2) blocker often used to prevent (Winter 2016) 26(4); p9-p19. Go to http:// and treat gastrointestinal ulcers, is a potent inhibitor of www.ejcap.org for the interactive online presentation of this paper several families of cytochrome P450 enzymes in humans, including CYP2D6 and CYP3A4 [2]. Cimetidine can also inhibit transporter pumps and decrease the renal tubular Introduction secretion of some drugs [3]. Cimetidine decreases the clearance of many drugs to variable degrees in humans, In humans, the risk of adverse drug interactions multiplies including theophylline [4,5], lidocaine [6], midazolam [7,8], as the number of administered drugs increases. -

Cleistanthus Nokrensis (Euphorbiaceae), a New Species from Indian Himalaya
Taiwania, 59(3): 197‒205, 2014 DOI: 10.6165/tai.2014.59.197 RESEARCH ARTICLE Cleistanthus nokrensis (Euphorbiaceae), a New Species from Indian Himalaya Bikarma Singh(1,2*), S.K. Borthakur(3) and S. J. Phukan(4) 1. Plant Biotechnology Division (Herbarium & Plant Systematic Section), CSIR-Indian Institute of Integrative Medicine, Canal Road, Jammu-Tawi-180001, India. 2. Academy of Scientific and Innovative Research, Anusandhan Bhawan, 2 Rafi Marg, New Delhi-110001, India. 3. Department of Botany, Gauhati University, Guwahati-781014, Assam, India. 4. Botanical Survey of India, Eastern Regional Circle, Shillong 793001, India. * Corresponding author. Email: [email protected] (Manuscript received 27 December 2013; accepted 04 April 2014) ABSTRACT: A new species, Cleistanthus nokrensis (Euphorbiaceae), was collected and described from Indian Himalaya. This species is confined to the Nokrek Biosphere Reserve where it grows on the calcareous habitat in karst topography. On the basis of the critical features of its habitat, branches, petioles, leaves, and fruits, the species is compared with the closely related allied species, C. tonkinensis Jabl. and C. balakrishnanii Chakrab. Notes on its taxonomic description, photographs, ecology, associated species, population data, and threat perspective as per latest IUCN conservation status are provided. A key to the other taxa in the genus reported from India is provided for the first time, along with their distributional records and endemism. KEY WORDS: Cleistanthus nokrensis, Euphorbiaceae, Indian Himalaya, IUCN Red List, new species. INTRODUCTION to Chakrabarty et al. (2002) and Mabberley (2008) has its centre of diversity in the Old World tropics and Myers et al. (2000) estimated that 133,149 plant represented by 148 species.