Mentors in Waiting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Waste Water Transformed Into Heat Energy Abstract 1. Introduction
Waste water transformed into heat energy Authors: Konstantinos Ninikas 1, Nicholas Hytiris 1, Rohinton Emmanuel 1, Bjorn Aaen 1, Paul L. Younger 2 1 Glasgow Caledonian University, UK. – 2 University of Glasgow, UK. Abstract This study investigates the feasibility of utilising ground water ingress into the Glasgow Subway system. At present this unused excess water is being discharged into the city’s drainage system as waste. This valuable resource could be channelled through a Water Source Heat Pump (WSHP) to produce heat energy for domestic or public use (heating and domestic hot water). A study has been carried out in order to calculate the heat contained in the water. Water flow and water temperature have been recorded over a ten month period (since May 2014) at fifteen different points within the network of underground tunnels. Water sampling has also been undertaken at all of these points, with chemical analysis results for six of them already obtained. The measurements will continue for at least seven more months to have readings for an 18 months period. A feasibility study to review the number of support factors (i.e. Renewable Heat Incentive) that could profit the subway system has been undertaken as well. Options have been discussed and a selection of a site inside the tunnels for a pilot system has been decided and is due to be installed in June 2015. The findings of this study are expected to develop an appropriate renewable solution through a cost effective heat pump system design. This waste water will be collected and used as renewable energy. -
Campus Travel Guide Final 08092016 PRINT READY
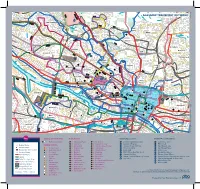
Lochfauld V Farm ersion 1.1 27 Forth and 44 Switchback Road Maryhill F C Road 6 Clyde Canal Road Balmore 1 0 GLASGOW TRANSPORT NETWORK 5 , 6 F 61 Acre0 A d Old Blairdardie oa R Drumchapel Summerston ch lo 20 til 23 High Knightswood B irkin e K F 6 a /6A r s de F 15 n R F 8 o Netherton a High d 39 43 Dawsholm 31 Possil Forth and Clyde Canal Milton Cadder Temple Gilshochill a 38 Maryhill 4 / 4 n F e d a s d /4 r a 4 a o F e River Lambhill R B d Kelvin F a Anniesland o 18 F 9 0 R 6 n /6A 1 40 r 6 u F M 30 a b g Springburn ry n h 20 i ill r R Ruchill p Kelvindale S Scotstounhill o a Balornock 41 d Possil G Jordanhill re Park C at 19 15 W es 14 te rn R 17 37 oa Old Balornock 2 d Forth and D um Kelvinside 16 Clyde b North art 11 Canal on Kelvin t Ro Firhill ad 36 ee 5 tr 1 42 Scotstoun Hamiltonhill S Cowlairs Hyndland 0 F F n e 9 Broomhill 6 F ac 0 r Maryhill Road V , a ic 6 S Pa tor Dowanhill d r ia a k D 0 F o S riv A 8 21 Petershill o e R uth 8 F 6 n F /6 G r A a u C 15 rs b R g c o u n Whiteinch a i b r 7 d e Partickhill F 4 p /4 S F a River Kelvin F 9 7 Hillhead 9 0 7 River 18 Craighall Road Port Sighthill Clyde Partick Woodside Forth and F 15 Dundas Clyde 7 Germiston 7 Woodlands Renfrew Road 10 Dob Canal F bie' 1 14 s Loa 16 n 5 River Kelvin 17 1 5 F H il 7 Pointhouse Road li 18 5 R n 1 o g 25A a t o Shieldhall F 77 Garnethill d M 15 n 1 14 M 21, 23 10 M 17 9 6 F 90 15 13 Alexandra Parade 12 0 26 Townhead 9 8 Linthouse 6 3 F Govan 33 16 29 Blyt3hswood New Town F 34, 34a Anderston © The University of Glasgo North Stobcross Street Cardonald -

Student / Living
1 STUDENT / LIVING 3 INVESTMENT CONSIDERATIONS • Prime student accommodation opportunity in • Commonwealth Games in Glasgow in 2014 core city centre location, fully let for 2013/14 will help bolster the city’s international reputation • Additional income from Sainsbury’s and Ask Restaurants • Potential to increase future income by continuing to move all student • 133 bedroom studio accommodation (140 accommodation contract lengths to 51 weeks beds), providing an average bedroom size of 27.14 sq m and excellent common facilities • Savills are instructed to seek offers in excess of £16,500,000 (sixteen million five • Highest specified scheme in Glasgow. The hundred thousand pounds) for the heritable property is a former lifestyle boutique hotel, title of the property, which reflects a net initial extensively refurbished and converted to yield of 6.40% on the student income, 6.00% student use in 2011 for the Sainsbury’s and 6.75% on the Ask unit, assuming purchaser’s costs of 5.80%. • Glasgow is a renowned and established The asset is for sale inclusive or exclusive of centre for higher education, boasting three the retail element. The SPV is also available main universities and a full time student to purchase and details can be provided on population of 50,450 request. • Excellent location within the heart of the city in close proximity to university campuses including Glasgow Caledonian and Strathclyde universities 4 S A R LOCATION A C E N S T A81 Glasgow is Scotland’s largest city and one of A879 the largest in the United Kingdom boasting G five recognised higher education institutions. -

Download Download
Scottish Tradition Vol. 27 2002 WORKING CLASS CULTURE, FAMILY LIFE AND DOMESTIC VIOLENCE ON CLYDESIDE, C 1918-1939: A VIEW FROM BELOW. ‘People have no idea how the poor lived in those days. They seemed to be at loggerheads all the time.’ 1 he inter-war years were distinguished by marked changes that affected the lives and neighbourhoods of Tmany working class men and women. These changes would prove to have positive and negative implications for working-class family life. New employment opportunities extended the breadth of jobs open to working class people, espe- cially in the new consumer industries that employed significant numbers of women. Correspondingly, the commercialisation of leisure expanded the possibilities of pleasure. Information on birth control and the greater ease of availability of contraceptives also offered a better potential to postpone marriage and reduce family size. Yet, the new employment opportunities did little to alter the ‘pin money’ wages of women and women’s economic dependency on marriage. Marriage was still seen as an attractive alternative to employment in the longer term.2 Marriage and motherhood were actively promoted as the natural and fulfilling aspirations for women by the state, state agencies, the clergy, religious organisations and the media. Adding to the appeal was the ideal of the ‘companionate marriage’ in which husbands were expected to share chores, child-care, leisure and provide love and companionship. It seems that this was a ‘fairly norma- tive’ aspiration amongst many sectors of the working class between the wars, at least amongst women. Change, however, was not just ideological.3 After World War I, the building of ‘homes fit for heroes’ and the growth of ‘new garden cities’, were linked with ideals of the companionate marriage, maternalism, privacy, respectable domesticity and the growth of male home- centred pastimes. -

7A Bus Time Schedule & Line Route
7A bus time schedule & line map 7A Westburn - Summerston via Rutherglen, Kings Park View In Website Mode and Glasgow City Centre The 7A bus line (Westburn - Summerston via Rutherglen, Kings Park and Glasgow City Centre) has 5 routes. For regular weekdays, their operation hours are: (1) Cambuslang: 6:30 PM (2) Glasgow: 6:48 AM - 10:29 PM (3) Rutherglen: 4:58 PM - 11:00 PM (4) Summerston: 6:27 AM - 5:07 PM (5) Westburn: 6:42 AM - 4:38 PM Use the Moovit App to ƒnd the closest 7A bus station near you and ƒnd out when is the next 7A bus arriving. Direction: Cambuslang 7A bus Time Schedule 6 stops Cambuslang Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 6:30 PM Dunlop Street, Westburn 205 Westburn Road, Glasgow Tuesday 6:30 PM Northbank Street, Westburn Wednesday 6:30 PM Newton Road, Westburn Thursday 6:30 PM Friday 6:30 PM Old Mill Road, Cambuslang Saturday Not Operational Kings Crescent, Cambuslang Christie Place, Cambuslang 7A bus Info Direction: Cambuslang Stops: 6 Trip Duration: 6 min Line Summary: Dunlop Street, Westburn, Northbank Street, Westburn, Newton Road, Westburn, Old Mill Road, Cambuslang, Kings Crescent, Cambuslang, Christie Place, Cambuslang Direction: Glasgow 7A bus Time Schedule 57 stops Glasgow Route Timetable: VIEW LINE SCHEDULE Sunday 7:30 AM - 10:29 PM Monday 6:48 AM - 10:29 PM Dunlop Street, Westburn 205 Westburn Road, Glasgow Tuesday 6:48 AM - 10:29 PM Northbank Street, Westburn Wednesday 6:48 AM - 10:29 PM Newton Road, Westburn Thursday 6:48 AM - 10:29 PM Friday 6:48 AM - 10:29 PM Old Mill Road, -

75 Bus Time Schedule & Line Route
75 bus time schedule & line map 75 Castlemilk - Milton via Glasgow City Centre View In Website Mode The 75 bus line (Castlemilk - Milton via Glasgow City Centre) has 3 routes. For regular weekdays, their operation hours are: (1) Castlemilk: 12:01 AM - 11:31 PM (2) Glasgow: 5:40 AM (3) Milton: 4:33 AM - 11:23 PM Use the Moovit App to ƒnd the closest 75 bus station near you and ƒnd out when is the next 75 bus arriving. Direction: Castlemilk 75 bus Time Schedule 77 stops Castlemilk Route Timetable: VIEW LINE SCHEDULE Sunday 12:01 AM - 11:31 PM Monday 12:01 AM - 11:31 PM Milton Bus Terminus, Milton Skerray Street, Glasgow Tuesday 12:01 AM - 11:31 PM Shapinsay Street, Milton Wednesday 12:01 AM - 11:31 PM Scaraway Street, Glasgow Thursday 12:01 AM - 11:31 PM Scaraway Terrace, Milton Friday 12:01 AM - 11:31 PM Scaraway Street, Milton Saturday 12:01 AM - 11:31 PM Shillay Street, Milton John Marshall Drive, Milton Ashgill Road, Glasgow 75 bus Info Direction: Castlemilk Colston Road, Milton Stops: 77 Trip Duration: 73 min St Augustines Church, Milton Line Summary: Milton Bus Terminus, Milton, Shapinsay Street, Milton, Scaraway Terrace, Milton, Berneray Street, Milton Scaraway Street, Milton, Shillay Street, Milton, John Marshall Drive, Milton, Colston Road, Milton, St Ashƒeld Street, Milton Augustines Church, Milton, Berneray Street, Milton, Ashƒeld Street, Milton, Kippen Street, Milton, Ashƒeld Harmetray Street, Glasgow Railway Station, Possil, Hawthorn Quadrant, Possil, Kippen Street, Milton Hawthorn Court, Possil, Saracen Street, Possil, Closeburn -

UK Data Archive Study Number 66037 - Survey of Party Workers in Glasgow, 1966
UK Data Archive Study Number 66037 - Survey of Party Workers in Glasgow, 1966 SSRC C001-25 66037 PRETEST ACTIVIST INTERVIEW INTERVIEWER'S NAME COVER SHEET NO. TIME STARTED DATE 1. WHEN DID YOU FIRST BECOME ACTIVE IN POLITICS? 2. HAVE YOU BEEN ACTIVE IN POLITICS EVER SINCE? YES NO DON'T KNOW IF YES, GO TO Q.3 (IF NO OR DON'T KNOW) 2A WOULD YOU TELL ME ABOUT THAT? 3. HAVE YOU HELD ANY (OTHER) OFFICES IN THE PARTY? YES NO DON'T KNOW (IF YES) 3A. WHAT IS THAT? WHEN WAS THAT? (GET OFFICES AND DATES) IF NO OR DON'T KNOW, GO TO Q.4 4. HAVE YOU HELD ANY PUBLIC OFFICES? YES NO DON'T KNOW (IF YES) 4A. WHAT IS THAT? WHEN WAS THAT? (FIND IF R HOLDS OFFICE NOW) IF NO OR DON'T KNOW, GO TO Q.5 5. THINKING BACK TO WHEN YOU FIRST BECAME ACTIVE IN POLITICS, WHY DID YOU BECOME ACTIVE THEN? (IF FRIENDS OR RELATIVES NOT MENTIONED) 5A. WOULD YOU SAY THAT ANY FRIENDS OR RELATIVES WERE IMPORTANT IN GETTING YOU INTERESTED IN POLITICAL ACTIVITY? YES NO (IF YES) 5B. IN WHAT WAY? (IF NECESSARY) WHO WERE THEY? (GET RELATIONSHIP) IF NO, GO TO Q.5C (IF ORGANIZATIONS NOT MENTIONED) 5C. WAS YOUR MEMBERSHIP IN ANY ORGANIZATIONS IMPORTANT IN GETTING YOU INTERESTED IN POLITICAL ACTIVITY? YES NO (IF YES) 5D. IN WHAT WAY? (IF NECESSARY) WHAT ORGANIZATION(S) WERE THOSE? IF NO, GO TO Q.6 (IF R HAS A PARTY OFFICE) 6. WHEN YOU FIRST BECAME (R'S PRESENT OFFICE) WERE THERE ANY OTHER CANDIDATES FOR THE OFFICE? YES NO DON'T KNOW 7. -

International Welcome Brochure January 2021
Campus Life Team Glasgow Caledonian University Cowcaddens Road Glasgow G4 0BA Contact Student Events Team E: [email protected] Join our Officia Group: groups/ janwelcome2021 Connect: InternationalWelcomeGCUGCUStudentsLife www Visit: gcu.ac.uk/ students/ studentlife/ events Glasgow Caledonian University is a registered Scottish charity, number SC021474. © Glasgow Caledonian University 2020, 08/ 20. International Student Welcome Programme January 2021 3 Hello and welcome Hello and welcome from the Student Engagement and Events Team at Glasgow Caledonian University. We are delighted you have chosen to study at GCU and join our international University. This is an exciting time as you take the next step towards your future. We host the International Welcome Programme to support you Meet Jessica in making this big step. The programme includes social events, Jessica is our Student Events Coordinator and they are opportunities to meet students and staff, and essential responsible for delivering our International Welcome information. Programme, as well as Freshers' Week and other on-campus student events. As you begin your studies, you may find that joining a new university and moving to a new city or country can be a challenging experience. We are here to help you throughout this time. Remember, other students are going through similar experiences to you so invite your new friends along to events and activities as well. We wish you every success in your studies at GCU and hope the experience is rewarding, successful and most of all, fun. We look forward to meeting you during the programme and getting to know you during your journey at GCU. -

55 Blythswood Street Glasgow to Let G2
To Let Modern refurbished 55 Blythswood Street office space Glasgow 5th floor G2 7AT 9,658 sq ft / 897 sq m The Spectrum Building gives occupiers the opportunity to work from one of Glasgow’s most recognisable office buildings, right in the heart of the Central Business District. SPECTRUM BUILDING 03 Large, flexible open - Floor to ceiling height glazing - Exceptional natural daylighting plan floor plates - 150mm metal deck raised access floor - 4 pipe fan coil air-conditioning The Spectrum Building offers space planning - Metal suspended ceiling incorporating LED lighting options that can be tailored to suit your business. - 4 secure car parking spaces Following extensive refurbishment, Indicative Space Planning the Spectrum Building provides outstanding contemporary space to 5th Floor suit the most discerning of occupiers. 9,658 sq ft 897 sq m ACC. WC 1:8 sq m per person FEMALE TOILETS MALE Total Staff: 109 Break Out / Collaboration Space (x1) TOILETS LIFT Reception (x1) Canteen / Informal Breakout (x1) SHOWER LOBBY Office (x1) Recycling / Print Area (x2) COMMS ROOM Meeting Rooms (x3) Storage Room (x1) LIFT MEETING ROOM Project Space (x2) Comms Room (x1) (14 person) Study Booth (x2) OPEN PLAN (x28) CANTEEN & INFORMAL BREAKOUT STORAGE BREAKOUT COLLABORATION SPACE MEETING ROOM RECEPTION RECYCLING MEETING ROOM (6 person) RECYCLING (6 person) STUDY STUDY PROJECT PROJECT BOOTH BOOTH SPACE SPACE PRINT PRINT OPEN PLAN (x78) OFFICE ACC. 1:10 sq m per person WC FEMALE TOILETS Total Staff: 87 Project Space (x2) MALE Reception (x1) Break Out / -

21E New City Road, Cowcaddens
21E New City Road, Cowcaddens www.nicolestateagents.co.uk Situation New City Road is conveniently located for access to the City Centre, the Merchant City, Financial District and West End amenities including Glasgow University, Botanic Gardens and Kelvingrove Park & Art Galleries. The City Centre, West End and the Merchant City offers a wealth of amenities including both general and specialist shopping, wine bars and many highly acclaimed restaurants. The property is near Strathclyde & Caledonian Universities and the Glasgow School of Art. The area benefits from frequent public transport with easy access to Central and Queens Street Train Stations, Cowcaddens and Buchanan Street subway stations. The nearby Clydeside Expressway, Clyde Tunnel, M77 and the M8/M80 ensure good commuter access throughout the Central Belt and is within easy reach of some of Scotland’s most impressive countryside attractions, including Loch Lomond and The Trossachs National Park. Description A bright and well presented upgraded one bedroom second floor flat, located within this popular development, close to Glasgow’s City Centre and West End, with a private allocated resident’s parking space. The complete accommodation comprises: Well-kept communal entrance with stair access to all levels. Welcoming reception hallway. Bright sitting /dining room. Well appointed refitted kitchen with a range of floor and wall cabinets and coordinated worktops. Double bedroom with wardrobe. An attractive bathroom with three piece suite with electric shower completes the overall accommodation. The property is further complemented by private allocated resident’s parking space, replacement double glazing and electric central heating. www.nicolestateagents.co.uk 21E New City Road, Cowcaddens, G4 9DE Approximate gross internal area 446 sq ft - 41 sq m Viewing Energy Efficiency Rating By appointment through Band C Nicol Estate Agents 46 Ayr Road Services Newton Mearns, Glasgow G46 6SA The property will be supplied by mains water, Telephone 0141 616 3960 electricity and drainage. -

Glasgow North West Youth Programme
Glasgow NW Youth Network Draft Logic Model What will the Youth Network produce, create or establish? What What will change in the What will be What will resources are short-term? achieved in improve needed? Engagement: the medium- in the Youth Network: GNW Youth DRC term? long- Produce a A&M Training Individuals: term Asset Audit: logic model Programme Glasgow Life Improved confidence future? Data gathered on with a e.g. strategic J&BG More engaged in learning Local Youth focus CPP More active & making Providers Establish a G15 Targeted Support: healthy choices Note of ladder of TSYP Quarriers resources support Aberlour Glasgow Council (e.g. buildings providing an on Alcohol & staff) open NW CHP Schools & Note of New Experiences: Community: programme NW HIT Young existing funds SiMY Reduced truancy & and targeted J&BG people are Note of Community exclusion support Lifelink more active, Improved existing across the PT Charitable Breaking the NEET DRC Generations respected, Trust trends health & programmes area responsible, Glasgow Life YMCA (Mentoring) wellbeing Organise a Improved area included, Note of other NUC statistics partnership safe, for young resources e.g. structure More involvement healthy, people in local m and in community/ achieving Glasgow parks/public resources to Advanced volunteering and nurtured North West places & fit with the Opportunities: Better qualifications (GIRFEC) spaces model NG Sports Specialists Joint training Legacy Potential Marketing Glasgow Life funds/funders -

Cowcaddens 81 Port Dundas Road, Flat 1/1
Cowcaddens 81 Port Dundas Road, Flat 1/1 www.clydeproperty.co.uk 81 Port Dundas Road, Flat 1/1, Cowcaddens G4 0HF This beautifully appointed three bedroom urban living on offer, this property will surely executive flat is set on the preferred first floor of appeal to many types of prospective purchasers. the much admired Fourth Quarter development There is an abundance of great storage space by Messrs Bellway Homes. The property enjoys offered throughout. The specification of the Viewing a fabulous location, close to the many amenities property includes high performance double By appointment please through and attractions offered by Glasgow’s pulsating glazed window units, gas fired central heating Clyde Property West End City centre. Glasgow, Strathclyde and Caledonia and security entry system. There is also a Universities are all within close proximity, as lift service in operation which gives swift 0141 576 1777 are the world renowned School of Art, Dental access to all floors. The property also benefits [email protected] Hospital and The Royal Conservatoire of from a concierge service. The commodious we’re available till 8pm every day Scotland. This particular property has a covered accommodation on offer comprises; welcoming private parking space and balcony with open reception hallway with storage cupboards off, EER Rating Band C views over the raised communal garden area naturally bright spacious lounge which gives which offers a wonderful outdoor space in access to the balcony and has ample space for which to relax and unwind. dining table and chairs, fully fitted kitchen which Property Ref HP02051 is open plan to the lounge, master bedroom with As soon as you set foot inside this stunning built in wardrobes and ensuite shower room, property you will appreciate the level of attention two further double bedrooms, both of which to detail throughout.