Mild Primary Hyperparathyroidism C.W
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
In Silico Methods for Drug Repositioning and Drug-Drug Interaction Prediction
In silico Methods for Drug Repositioning and Drug-Drug Interaction Prediction Pathima Nusrath Hameed ORCID: 0000-0002-8118-9823 Submitted in total fulfilment of the requirements for the degree of Doctor of Philosophy Department of Mechanical Engineering THE UNIVERSITY OF MELBOURNE May 2018 Copyright © 2018 Pathima Nusrath Hameed All rights reserved. No part of the publication may be reproduced in any form by print, photoprint, microfilm or any other means without written permission from the author. Abstract Drug repositioning and drug-drug interaction (DDI) prediction are two fundamental ap- plications having a large impact on drug development and clinical care. Drug reposi- tioning aims to identify new uses for existing drugs. Moreover, understanding harmful DDIs is essential to enhance the effects of clinical care. Exploring both therapeutic uses and adverse effects of drugs or a pair of drugs have significant benefits in pharmacology. The use of computational methods to support drug repositioning and DDI prediction en- able improvements in the speed of drug development compared to in vivo and in vitro methods. This thesis investigates the consequences of employing a representative training sam- ple in achieving better performance for DDI classification. The Positive-Unlabeled Learn- ing method introduced in this thesis aims to employ representative positives as well as reliable negatives to train the binary classifier for inferring potential DDIs. Moreover, it explores the importance of a finer-grained similarity metric to represent the pairwise drug similarities. Drug repositioning can be approached by new indication detection. In this study, Anatomical Therapeutic Chemical (ATC) classification is used as the primary source to determine the indications/therapeutic uses of drugs for drug repositioning. -

DIURETICS Diuretics Are Drugs That Promote the Output of Urine Excreted by the Kidneys
DIURETICS Diuretics are drugs that promote the output of urine excreted by the Kidneys. The primary action of most diuretics is the direct inhibition of Na+ transport at one or more of the four major anatomical sites along the nephron, where Na+ reabsorption takes place. The increased excretion of water and electrolytes by the kidneys is dependent on three different processes viz., glomerular filtration, tubular reabsorption (active and passive) and tubular secretion. Diuretics are very effective in the treatment of Cardiac oedema, specifically the one related with congestive heart failure. They are employed extensively in various types of disorders, for example, nephritic syndrome, diabetes insipidus, nutritional oedema, cirrhosis of the liver, hypertension, oedema of pregnancy and also to lower intraocular and cerebrospinal fluid pressure. Therapeutic Uses of Diuretics i) Congestive Heart Failure: The choice of the diuretic would depend on the severity of the disorder. In an emergency like acute pulmonary oedema, intravenous Furosemide or Sodium ethacrynate may be given. In less severe cases. Hydrochlorothiazide or Chlorthalidone may be used. Potassium-sparing diuretics like Spironolactone or Triamterene may be added to thiazide therapy. ii) Essential hypertension: The thiazides usually sever as primary antihypertensive agents. They may be used as sole agents in patients with mild hypertension or combined with other antihypertensives in more severe cases. iii) Hepatic cirrhosis: Potassium-sparing diuretics like Spironolactone may be employed. If Spironolactone alone fails, then a thiazide diuretic can be added cautiously. Furosemide or Ethacrymnic acid may have to be used if the oedema is regractory, together with spironolactone to lessen potassium loss. Serum potassium levels should be monitored periodically. -

(12) Patent Application Publication (10) Pub. No.: US 2005/0113314 A1 Fong Et Al
US 20050113314A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2005/0113314 A1 Fong et al. (43) Pub. Date: May 26, 2005 (54) CICLETANINE IN COMBINATION WITH Publication Classification ORAL ANTIDIABETIC AND/OR BLOOD LIPID-LOWERING AGENTS ASA COMBINATION THERAPY FOR DIABETES (51) Int. Cl." ..................... A61K 31/70; A61K 31/4741; AND METABOLIC SYNDROME A61K 31/426; A61K 31/155; A61K 31/175 (76) Inventors: Benson M. Fong, San Francisco, CA (52) U.S. Cl. ............................ 514/25; 514/302; 514/369; (US); Glenn V. Cornett, Palo Alto, CA 514/592; 514/635 (US) Correspondence Address: KNOBBE MARTENS OLSON & BEAR LLP 2040 MAIN STREET (57) ABSTRACT FOURTEENTH FLOOR IRVINE, CA 92614 (US) Preferred embodiments of the present invention are related to novel therapeutic drug combinations and methods for (21) Appl. No.: 10/929,108 treating and/or preventing complications in patients with (22) Filed: Aug. 27, 2004 diabetes and/or metabolic Syndrome. More particularly, aspects of the present invention are related to using a Related U.S. Application Data combination of cicletanine and an oral antidiabetic agent for treating and/or preventing complications (including microal (60) Provisional application No. 60/498,916, filed on Aug. buminuria, nephropathies, retinopathies and other compli 29, 2003. cations) in patients with diabetes or metabolic Syndrome. US 2005/0113314 A1 May 26, 2005 CICLETANNE IN COMBINATION WITH ORAL women >0.85) and/or Body Mass Index >30 kg/M); 6) ANTIDIABETIC AND/OR BLOOD micro albuminuria (urine albumin excretion: 220 ugmin' LIPID-LOWERING AGENTS ASA COMBINATION or albumin/creatinine ratio22.0 mg/mmol. -

US20050113367A1.Pdf
US 20050113367A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2005/0113367 A1 Sada et al. (43) Pub. Date: May 26, 2005 (54) PHARMACEUTICAL COMPOSITION (52) U.S. Cl. ......................................... 514/223.5; 514/381 (75) Inventors: Toshio Sada, Tokyo (JP); Makoto (57) ABSTRACT Mizuno, Funabashi-shi (JP) A pharmaceutical composition which comprises (i) an Correspondence Address: angiotensin II receptor antagonist having the following FRISHAUF, HOLTZ, GOODMAN & CHICK, formula (I), a pharmacologically acceptable Salt thereof, a PC pharmacologically acceptable ester thereof or a pharmaco 767 THIRDAVENUE logically acceptable Salt of Such ester, and (ii) a diuretic 25TH FLOOR which is at least one thiazide compound: NEW YORK, NY 10017-2023 (US) (73) Assignee: SANKYO COMPANY, LIMITED, (I) Tokyo (JP) HC (21) Appl. No.: 11/020,624 CH N OH (22) Filed: Dec. 23, 2004 Related U.S. Application Data --> (63) Continuation of application No. 10/442,874, filed on May 20, 2003, now Pat. No. 6,878,703, which is a continuation of application No. PCT/JP01/10095, filed on Nov. 19, 2001. (30) Foreign Application Priority Data Nov. 21, 2000 (JP). 2000-354327 May 31, 2001 (JP)...................................... 2001-164009 Publication Classification The pharmaceutical composition has an excellent hypoten Sive effect and low toxicity, and therefore is useful as a (51) Int. Cl." .................... A61K 3.1/549; A61K 31/4178 medicament for treating hypertension or heart disease. US 2005/0113367 A1 May 26, 2005 PHARMACEUTICAL COMPOSITION nist and one or more diuretics to warm-blooded animals (particularly humans) at effective doses, and a pharmaceu CROSS-REFERENCE TO RELATED tical composition for administering Simultaneously or APPLICATIONS Sequentially a specific angiotensin II receptor antagonist and one or more diuretics for preventing or treating hyperten 0001. -
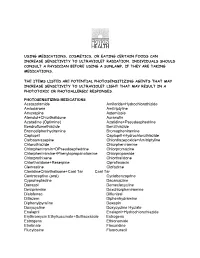
Using Medications, Cosmetics, Or Eating Certain Foods Can Increase Sensitivity to Ultraviolet Radiation
USING MEDICATIONS, COSMETICS, OR EATING CERTAIN FOODS CAN INCREASE SENSITIVITY TO ULTRAVIOLET RADIATION. INDIVIDUALS SHOULD CONSULT A PHYSICIAN BEFORE USING A SUNLAMP, IF THEY ARE TAKING MEDICATIONS. THE ITEMS LISTED ARE POTENTIAL PHOTOSENSITIZING AGENTS THAT MAY INCREASE SENSITIVITY TO ULTRAVIOLET LIGHT THAT MAY RESULT IN A PHOTOTOXIC OR PHOTOALLERGIC RESPONSES. PHOTOSENSITIZING MEDICATIONS Acetazolamide Amiloride+Hydrochlorothizide Amiodarone Amitriptyline Amoxapine Astemizole Atenolol+Chlorthalidone Auranofin Azatadine (Optimine) Azatidine+Pseudoephedrine Bendroflumethiazide Benzthiazide Bromodiphenhydramine Bromopheniramine Captopril Captopril+Hydrochlorothiazide Carbaamazepine Chlordiazepoxide+Amitriptyline Chlorothiazide Chlorpheniramine Chlorpheniramin+DPseudoephedrine Chlorpromazine Chlorpheniramine+Phenylopropanolamine Chlorpropamide Chlorprothixene Chlorthalidone Chlorthalidone+Reserpine Ciprofloxacin Clemastine Clofazime ClonidineChlorthalisone+Coal Tar Coal Tar Contraceptive (oral) Cyclobenzaprine Cyproheptadine Dacarcazine Danazol Demeclocycline Desipramine Dexchlorpheniramine Diclofenac Diflunisal Ditiazem Diphenhydramine Diphenylpyraline Doxepin Doxycycline Doxycycline Hyclate Enalapril Enalapril+Hydrochlorothiazide Erythromycin Ethylsuccinate+Sulfisoxazole Estrogens Estrogens Ethionamide Etretinate Floxuridine Flucytosine Fluorouracil Fluphenazine Flubiprofen Flutamide Gentamicin Glipizide Glyburide Gold Salts (compounds) Gold Sodium Thiomalate Griseofulvin Griseofulvin Ultramicrosize Griseofulvin+Hydrochlorothiazide Haloperidol -

Polythiazide in the Treatment of Congestive Heart Failure
Henry Ford Hospital Medical Journal Volume 10 | Number 4 Article 4 12-1962 Polythiazide In The rT eatment Of Congestive Heart Failure John W. Keyes Gerald M. Breneman Jose R. De Jesus Jr. Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Recommended Citation Keyes, John W.; Breneman, Gerald M.; and De Jesus, Jose R. Jr. (1962) "Polythiazide In The rT eatment Of Congestive Heart Failure," Henry Ford Hospital Medical Bulletin : Vol. 10 : No. 4 , 555-561. Available at: https://scholarlycommons.henryford.com/hfhmedjournal/vol10/iss4/4 This Article is brought to you for free and open access by Henry Ford Health System Scholarly Commons. It has been accepted for inclusion in Henry Ford Hospital Medical Journal by an authorized editor of Henry Ford Health System Scholarly Commons. For more information, please contact [email protected]. Henry Ford Hosp. Med. Bull. Vol. 10, December, 1962 POLYTHIAZIDE IN THE TREATMENT OF CONGESTIVE HEART FAILURE JOHN W. KEYES, M.D., GERALD M. BRENEMAN, M.D., JOSE R. DE JESUS, JR., M.D."' THE INTRODUCTION of chlorothiazide and its analogues in the past few years have made available potent oral diuretics which approach the organic mercurial compounds in efficacy. These drugs have shifted the emphasis from parenteral mercury, particularly for the long term management of various derivatives, all appear to be effective and safe diuretics. All of these compounds are active saluretic agents inhibiting tubular reabsorption of sodium, and causing increased excretion of chlorides. Potassium excretion is also significantly increased, but varies somewhat, depending on the particular analogue in use. -

FDA Listing of Established Pharmacologic Class Text Phrases January 2021
FDA Listing of Established Pharmacologic Class Text Phrases January 2021 FDA EPC Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: “(Drug) is a (FDA EPC Text Phrase) indicated for Active Moiety Name [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. -

Change Notification No 9
Northern Ireland BLOOD TRANSFUSION SERVICE Date of publication: 24th April 2006 Implementation: To be determined by each Service Change Notification UK National Blood Services No. 9 - 2006 Appendix 5 – Treatment for High Blood Pressure Applies to Tissue Donor Selection Guidelines – Bone Marrow and PBSC and also appears as Appendix 6 – Treatment for High Blood Pressure Applies to Donor Selection Guidelines - Whole Blood and Components The entry in both the guidelines is the same: Treatment for High Blood Pressure Donors who have been diagnosed with high blood pressure may donate provided that: 1. They have not suffered any adverse effects of raised blood pressure (BP) such as heart disease (angina, heart attack or heart failure), stroke, transient ischaemic attack (TIA or mini-stroke), or peripheral vascular disease (intermittent claudication, gangrene). 2. They are taking only a Beta(ß)-blocker and/or diuretic as their treatment for the raised BP. The list below shows the proper and trade names of allowed drugs. It is important to note that this list is not exclusive and that these drugs may be used to treat other conditions such as heart failure and abnormal heart rhythms (arrhythmia); both of which would mean the donor must not donate. Other medication should be assessed independently. 3. Treatment is stable. This requires: That the donor is well and not having any problems with feeling faint, fainting or giddiness. They have been on the same dose of medication for at least a month. They are not undergoing tests to find out the underlying -

European Patent Office
Europäisches Patentamt *EP001336407A1* (19) European Patent Office Office européen des brevets (11) EP 1 336 407 A1 (12) EUROPEAN PATENT APPLICATION published in accordance with Art. 158(3) EPC (43) Date of publication: (51) Int Cl.7: A61K 31/4178, A61K 31/54, 20.08.2003 Bulletin 2003/34 A61K 45/00, A61P 9/12 (21) Application number: 01982846.6 (86) International application number: PCT/JP01/10095 (22) Date of filing: 19.11.2001 (87) International publication number: WO 02/041890 (30.05.2002 Gazette 2002/22) (84) Designated Contracting States: (72) Inventors: AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU • SADA, Toshio SANKYO COMPANY, LIMITED MC NL PT SE TR Shinagawa-ku, Tokyo 140-8710 (JP) • MIZUNO, Makoto SANKYO COMPANY, LIMITED (30) Priority: 21.11.2000 JP 2000354327 Shinagawa-ku, Tokyo 140-8710 (JP) 31.05.2001 JP 2001164009 (74) Representative: (71) Applicant: Sankyo Company, Limited Gibson, Christian John Robert et al Tokyo 103-8426 (JP) MARKS & CLERK, 57/60 Lincoln’s Inn Fields London WC2A 3LS (GB) (54) MEDICINAL COMPOSITIONS (57) [Constitution] EP 1 336 407 A1 Printed by Jouve, 75001 PARIS (FR) (Cont. next page) EP 1 336 407 A1 A pharmaceutical composition comprises an angiotensin II receptor antagonist selected from among compounds having the above general formula (I), pharmacologically acceptable salts thereof, pharmacologically acceptable esters thereof and pharmacologically acceptable salts of said esters, and one or more diuretics. [Effects] The pharmaceutical composition of present invention has an excellent hypotensive effect and low toxicity, and therefore is useful as a medicament for preventing or treating hypertension or heart diseases. -

Eappendix Eappendix Table 1. Identification of Comorbidities That
eAppendix eAppendix Table 1. Identification of Comorbidities That Classified Patients as Receiving a Statin for Secondary Prevention ICD-9-CM Codes ICD-9-CM Procedure CPT Codes Codes Coronary artery 410.xx, 411.xx, 412.x, CABG codes CABG codes disease/Unstable 413.x, 414.x, 429.7, 36.10, 36.11, 36.12, 33510, 33511, 33512, angina/MI/CABG, 429.71 36.13, 36.14, 36.15, 33513, 33514, 33516, Revascularization 429.79 36.16, 36.17, 36.19, 33517, 33518, 33519, (any single code in 996.03, 36.2, 33521, 33522, 33523, prior 10 years). v45.81 33533, 33534, 33535, 33536, 33572, 4110F, s2205, s2206, s2207, PCI codes s2208, s2209 00.66, 36.06, 36.07, 36.09, v45.82 PCI codes 36.01-36.04 92973, 92980, 92981, 92982, 92984, 92995, 92996, G0290 G0291 Peripheral Vascular 440.2, 440.3, 440.4, 38.08, 38.09, 38.13 37220, 37221, 37222, disease (any single 443.9 38.18, 38.19 37223, 37224, 37225, code in prior 10 39.25, 39.26 37226, 37227,37228, years). 39.29, 39.50, 39.90 37229,37230, 37231, 37232,37233, 37234, 37235 Stroke or TIA (Reker’s high sensitivity algorithm adapted to include TIA) Admission or 362.32, 362.33, 362.34, discharge primary 430.xx, diagnosis 431.xx 432.xx 433.01 433.11, 433.21, 433.31, 433.81 433.91, 434.01,434.11, 434.91, 435.x 436.xx, 997.02 Rehab Admission or 342.xx 362.31 362.32 discharge primary 362.33 362.34 430.xx, diagnosis is V57.xx 431.xx 432.xx 433.01, (Rehabilitation) and 433.11, 433.21, 433.31, any secondary 433.81, 433.91, diagnosis 434.01,434.11, 434.91, 435.x, 436.xx, 997.02 Admission or 342.xx 362.31 362.32 discharge primary 362.33 362.34 430.xx, diagnosis is 433.xx 431.xx 432.xx 433.01, and 434.xx and any 433.11, 433.21, 433.31, secondary diagnosis 433.81, 433.91, code 434.01,434.11, 434.91, 435.x 436.xx, 997.02 eAppendix Table 2. -

SUPPLEMENTARY MATERIAL 1: Search Strategy
SUPPLEMENTARY MATERIAL 1: Search Strategy Medline search strategy 1. exp basal ganglia hemorrhage/ or intracranial hemorrhages/ or cerebral hemorrhage/ or intracranial hemorrhage, hypertensive/ or cerebrovascular disorders/ 2. ((brain$ or cerebr$ or cerebell$ or intracerebral or intracran$ or parenchymal or intraparenchymal or intraventricular or infratentorial or supratentorial or basal gangli$ or putaminal or putamen or posterior fossa or hemispher$ or pon$ or lentiform$ or brainstem or cortic$ or cortex$ or subcortic$ or subcortex$) adj5 (h?emorrhag$ or h?ematoma$ or bleed$)).tw 3. ((hemorrhag$ or haemorrhag$) adj6 (stroke$ or apoplex$ or cerebral vasc$ or cerebrovasc$ or cva)).tw 4. (ICH or ICHs or PICH or PICHs).tw 5. 1 or 2 or 3 or 4 6. exp blood pressure/ 7. exp hypertension/ 8. (blood pressure or bloodpressure).tw 9. ((bp or blood pressure) adj5 (lowering or reduc$)).tw 10. ((strict$ or target$ or tight$ or intens$ or below) adj3 (blood pressure or systolic or diastolic or bp or level$)).tw 11. (hypertension or hypertensive).tw 12. ((manage$ or monitor$) adj3 (hypertension or blood pressure)).tw 13. ((intense or intensive or aggressive or accelerated or profound or radical or severe) adj5 ((bp or blood pressure) adj5 (lowering or reduc$ or decreas$ or decrement or dimin$ or declin$))).tw 14. ((standard or normal or ordinary or guideline or guide line or guideline recommend$ or recommend$ or convention$ or usual or established) adj5 ((bp or blood pressure) adj5 (lowering or reduc$ or decreas$ or decrement or dimin$ or declin$))).tw 15. (antihypertensive adj2 (agent$ or drug$ or medicat$)).tw 1 16. 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 17. -

Index Vol. 16-23
233 Index Vol. 16-23 The references of the Subject Index are given in the language of the respective contribution. Die Stichworte des Sachregisters sind in der jeweiligen Sprache der einzelnen Beitrage aufgeftihrt. Les termes repris dans la Table des matieres sont donnes selon la langue dans laquelle l'ouvrage est ecrit. A 17 Abortion, therapeutic 457,460 23 Acetylsalicylic acid (Aspirin®) 114 20 Academic research 169 16 O-Acetylserin-Sulfhydrylase A 390 18 Acanthocheilonema perstans 142 17 Acetylstrophanthidin 35 18 Acanthocheilonema streptocerca 142 22 Achromycin® (tetracycline) 53 22 Acaprin® (quinuronium sulfate) 42 19 Acidosis 529 20 Acebutolol 33, 36, 229 18 Acid phosphotase 66 18 Acedapson (Hansolar®, 4',4"'-sulfonylbis 16 Aconitase-Isomerase 436 acetanilide) 108, 156 17 Aconitine 35,46 17 Acedist® (bromfenofos, Ph 1882) 113, 134, 17 Acranil 119, 152 278 17 Acrichine® (quinacrine) 119 18 Aceperone 437 17 Acridine 295 16 Acetacetat-Decarboxylase 414 16 Acriftavin 100 17 2-Acetamido-5-nitrothiazole 261 17 Acrolein 358 17 Acetanilide 23, 497 18 Acronine 440 20 Acetanilide 400 21 Acrosin 366 23 Acetanilide 212 21 Acrylamide 186 20 Acetazolamide (Diamox®) 209,417 17 Actamer® (bithionol) 114,297 21 - 114 22 Actamer® (bithionol) 46 22 Acetohexamide (Dymelor®) 81 16 Actinomycin I 298 17 Acetohydroxamic acid 348 16 Actinomycin IV 298 17 Acetone 13, 17 16 Actinomycin V 298 16 Acetophenone 260 17 Actinomycin C, (actinomycin D) 376 17 2-Acetoxy-4' -chloro-3,5-diiodobenzanilide 16 Actinomycin D (actinomycin C" (clioxanide) 114,135,164,277,281