A Role for Topical Decongestants?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers with Topical Pharmaceutical Agents
Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Author Watts, Annabelle M, Cripps, Allan W, West, Nicholas P, Cox, Amanda J Published 2019 Journal Title FRONTIERS IN PHARMACOLOGY Version Version of Record (VoR) DOI https://doi.org/10.3389/fphar.2019.00294 Copyright Statement © Frontiers in Pharmacology 2019. The attached file is reproduced here in accordance with the copyright policy of the publisher. Please refer to the journal's website for access to the definitive, published version. Downloaded from http://hdl.handle.net/10072/386246 Griffith Research Online https://research-repository.griffith.edu.au fphar-10-00294 March 27, 2019 Time: 17:52 # 1 REVIEW published: 29 March 2019 doi: 10.3389/fphar.2019.00294 Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Annabelle M. Watts1*, Allan W. Cripps2, Nicholas P. West1 and Amanda J. Cox1 1 Menzies Health Institute Queensland, School of Medical Science, Griffith University, Southport, QLD, Australia, 2 Menzies Health Institute Queensland, School of Medicine, Griffith University, Southport, QLD, Australia Allergic rhinitis (AR) is a chronic upper respiratory disease estimated to affect between 10 and 40% of the worldwide population. The mechanisms underlying AR are highly complex and involve multiple immune cells, mediators, and cytokines. As such, the development of a single drug to treat allergic inflammation and/or symptoms is confounded by the complexity of the disease pathophysiology. Complete avoidance of allergens that trigger AR symptoms is not possible and without a cure, the available therapeutic options are typically focused on achieving symptomatic relief. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

Rhinitis - Allergic (1 of 15)
Rhinitis - Allergic (1 of 15) 1 Patient presents w/ signs & symptoms of rhinitis 2 • Consider other classifi cations of rhinitis DIAGNOSIS No - Please see Rhinitis Is allergic rhinitis - Nonallergic disease confi rmed? management chart Yes 3 ASSESS DURATION & SEVERITY OF ALLERGIC RHINITIS A Non-pharmacological therapy • Allergen avoidance • Patient education VAS <5 VAS ≥5 B Pharmacological therapy B Pharmacological therapy • Antihistamines (oral/nasal), &/or • Corticosteroids (nasal), w/ or without • Corticosteroids (nasal), or • Antihistamines (nasal), or • Cromone (nasal), or • LTRA • Leukotriene receptor antagonists (LTRA)MIMS TREATMENT © See next page Specifi cally for patients w/ asthma Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B167 © MIMS Pediatrics 2020 Rhinitis - Allergic (2 of 15) Previously treated symptomatic Previously treated symptomatic patient (VAS <5) on antihistamines patient (VAS ≥5) on intensifi ed (oral/nasal) &/or corticosteroids (nasal) therapy w/ corticosteroids (nasal) w/ or without antihistamines (nasal) Intermittent Persistent symptoms, symptoms or without allergen w/ allergen exposure exposure B Pharmacological therapy B Pharmacological therapy • Step down or discontinue therapy • Continue or step up therapy Untreated REASSESS DISEASE SEVERITY VAS symptomatic patient DAILY UP TO DAY 3 (VAS <5 or ≥5) 4 CONTINUE Yes THERAPY & STEP EVALUATION VAS <5 DOWN THERAPY1 Improvement of symptoms? No VAS ≥5 B Pharmacological therapy • Step-up therapy REASSESS DISEASE SEVERITY MIMSVAS DAILY UP TO DAY 7 4 Yes EVALUATION VAS <5 Improvement of symptoms? No TREATMENT © VAS ≥5 See next page Continue therapy if symptomatic; consider step-down or discontinuation of therapy if symptoms subside Not all products are available or approved for above use in all countries. -

Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

7-Nose II.Docx ( Updated F1 )
1 [Color index: Important | Notes | Extra] Editing 2 Diseases of the nose Supernumerary nostril Midline nasal sinus: Nasal clefts: Proboscis lateralis: Incomplete fusion of the right Failure of frontal nasal Due to imperfect fusion and left medial nasal process to develop between the maxillary process prominence. appropriately results into and the lateral nasal process. two separated halves of the nose. Polyrrhinia: Arrhinia: due to bilateral Half nose: due to unilateral absence of nasal placode Duplication of the medial nasal absence of nasal placodes. processes. This is serious because the newborn is a nose breather. mouth breathing is a learning process. Atresia of posterior nares ❖ Types: ● Bony (most commonly) ● Membranous ● Mixed ● Complete unilateral (most commonly) ● Complete bilateral surgical emergency ● Incomplete unilateral ● Incomplete bilateral ❖ Diagnosis: ● Total absence of nasal air flow ● Plastic catheter cannot be passed through the nose ● Post-rhinoscopy ● Radiographs 3 ● Emergency ● Transnasal perforation ● Trans-palatal excision ❖ Management: ﻧﻔﺘﺢ ﻓﻤﻪ ﻓﯿﻀﻄﺮ ﯾﺘﻨﻔﺲ ﻣﻦ ﻓﻤﻪ (Put something to open the mouth (oral airway ● ● Perforate it If membranous ● Surgery (endoscopic) ● In bilateral it is an emergency, in unilateral it is not an emergency and we can wait until the child gains weight then we do surgery. ● Rhinitis refers to inflammatory changes in the nasal mucosa. As the nasal mucosa is continuous over the nose and sinuses, there is nearly always some inflammatory change in the sinuses as 1 well. Hence Rhinosinusitis is a better term. ● Types: - acute rhinitis (less than 4 weeks) - chronic rhinitis (more than four consecutive weeks) ● Types based on etiology: 1) Infectious rhinitis(viral/bacterial) 2)Non-allergic Rhinitis,Non-infectious rhinitis -Eosinophilic syndromes(Nares/Nasal polyposis) -NonEosinophilic syndromes(Vasomotor rhinitis/Rhinitis medicamentosa/occupational rhinitis/Rhinitis of pregnancy/hypothyroidism/Medication(OCP). -

Rhinitis (415) 833-3780
Department of Allergy, Asthma & Immunology Kaiser Permanente San Francisco 1635 Divisadero Street, Suite 101 San Francisco, California 94115 RHINITIS (415) 833-3780 RHINITIS Nasal congestion, runny nose, sneezing, itching, post nasal drip, and sometimes headache are signs of a sensitive and inflamed nose or rhinitis. Rhinitis affects more than 40 million people in the United States. Rhinitis can be allergic or non-allergic. Allergy testing will help differentiate between allergic and non-allergic rhinitis. In addition, allergic rhinitis and non-allergic rhinitis can be present in the same person. ALLERGIC RHINITIS Allergic rhinitis is caused by allergens such as pollens, dust mite, animal dander or mold. Seasonal allergies caused by airborne pollens occur during spring, summer and fall. In contrast, allergies that can occur at any time of the year are caused by indoor allergens such as house dust mite, animals and mold. Eye symptoms, such as itching, tearing, red eye as well as asthma may be present with allergic rhinitis. Testing can be helpful in identifying both seasonal and non-seasonal allergens. For further help on controlling your allergies, please refer to the brochure, Controlling Your Airborne Allergies. Management of Allergic Rhinitis 1. Avoid allergens when possible. 2. Medical Management. The first line of medical therapy is nasal inhaled steroids. Oral medications like antihistamines and decongestants and can be helpful. If you want to use decongestants, you need to discuss their use with your provider. Other medications may be considered by your provider as well. 3. Allergy immunotherapy (shots) may be an option for some patients. NON-ALLERGIC RHINITIS If it isn’t an allergy, what is it? If it isn’t an allergy, most likely it is a condition that mimics allergic rhinitis, known as vasomotor rhinitis. -
2013 Report on Prohibited Substances
2013 REPORT ON PROHIBITED SUBSTANCES Compiled by the Racing Medication and Testing Consortium, Supervised by the Advisory Council on Equine Prohibited Substances and Practices of the IFHA Racing Medication and Testing Consortium 821 Corporate Drive, Lexington, KY 40503, USA Phone +1(859) 224-2844 Fax +1(859) 296-3033 rmtcnet.com I. RACING DAY SAMPLES TOTAL DECLARED TOTAL DECLARED BOTH BOTH DECLARED DECLARE DECLARED DECLARE POSITIVE TOTAL TOTAL TOTAL URINE URINE BLOOD BLOOD NUMBER TOTAL DECLARED TOTAL POSITIVE HORSES HORSES URINE & URINE & TOTAL TOTAL DECLARED POSITIVE D POSITIVE D CASES ON SUBSTANCES NUMBER NUMBER BOTH ONLY ONLY ONLY ONLY OF DECLARED DECLARED POSITIVE DECLARED CASES ON SAMPLED SAMPLED BLOOD BLOOD URINE BLOOD POSITIVES CASES ON POSITIVE CASES ON POSITIVE BOTH DETECTED IN COUNTRY OF RACES OF URINE & SAMPLED SAMPLED SAMPLED SAMPLED DECLARE POSITIVES POSITIVE CASES ON POSITIVE BOTH PRE- POST- SAMPLED SAMPLED ONLY ONLY POST- URINE CASES ON BLOOD CASES ON URINE & OTHER HORSE (flat & HORSES BLOOD PRE- POST- PRE- POST- D PRE-RACE CASES ON URINE PRE- CASES ON URINE & RACE RACE PRE- POST- SAMPLED SAMPLED RACE POST- BLOOD POST- BOTH BLOOD COMPETITIONS jumps) SAMPLED SAMPLED RACE RACE RACE RACE POSITIVE URINE RACE BLOOD BLOOD RACE RACE RACE PRE-RACE RACE URINE & POST- CASES PRE-RACE BLOOD RACE Argentina 5,475 11,432 199 10,930 313 116 116 Australia 19,626 45,384 17,823 27,561 70 52 17 35 18 1 17 Austria 122 34 34 18 18 16 16 0 Bahrain 26 223 223 88 88 135 135 1 1 1 Belgium 189 183 157 26 0 Brazil 5,570 5,570 414 414 4,836 4,836 320 -

Research Article Meta-Analysis of the Efficacy of Ectoine Nasal Spray in Patients with Allergic Rhinoconjunctivitis
Hindawi Publishing Corporation Journal of Allergy Volume 2014, Article ID 292545, 12 pages http://dx.doi.org/10.1155/2014/292545 Research Article Meta-Analysis of the Efficacy of Ectoine Nasal Spray in Patients with Allergic Rhinoconjunctivitis Andrea Eichel,1 Andreas Bilstein,2 Nina Werkhäuser,2 and Ralph Mösges1 1 Institute of Medical Statistics, Informatics and Epidemiology, Faculty of Medicine, University of Cologne, Lindenburger Allee 42, 50931 Cologne, Germany 2 Bitop AG, Stockumer Straße 28, 58453 Witten, Germany Correspondence should be addressed to Andrea Eichel; [email protected] Received 15 January 2014; Revised 14 April 2014; Accepted 15 April 2014; Published 11 May 2014 Academic Editor: Desiderio Passali Copyright © 2014 Andrea Eichel et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Objectives. The meta-analysis aims to investigate the efficacy of ectoine nasal spray and eye drops in the treatment of allergic rhinitis and rhinoconjunctivitis symptoms. Design and Methods. This meta-analysis is based on yet unpublished data of four studies. Both nasal and eye symptoms were documented in patient diary cards. All scales were transformed into a 4-point scale: 0 = no, 1 = mild, 2 = moderate, and 3 = severe symptoms. Each symptom was analysed individually in a meta-analysis of the area under the curve values as well as in a meta-analysis of pre- and posttreatment comparison. Results. After seven days of treatment with ectoine nasal spray both nasal and ocular symptoms decreased significantly. -

Common Cold and Allergic Rhinitis
Common cold and allergic rhinitis • Sneezing, runny nose, and headache, were the main complaint of a man , his past medical history is negative, he does not take any medicine and he is not alcoholic, the best for him is (are) • Flue-out tab. • Phenylephrine +paracetamol. • Diphenhydramine alone. • Loratidine +phenylephrine. • All of the above. • You refused to give ampiclox vials to a father who describes the clinical picture of his child as follow: fever, rhinorrhea, sneezing, nasal congestion. All of the followings are causes of your rejection EXCEPT: • It is not an OTC drug. • The condition is caused by rota virus. • It rarely complicate to bacterial infection. • Use of ampiclox increases resistance to drugs. • The condition is self limiting. • A mother asks for something to prevent allergic rhinitis of her 5 years old child before symptoms starts, your choice will be: • Subcutaneous injection with child specific allergen. • Beclomethasone nasal spray. • Diphenhydramine syrup. • Cromolyn sodium nasal solution. • All are correct. Definition C.c is a self limiting viral infection. of upper respiratory tract. C.c is usually self limiting but the bothersome symptoms make patients self medicate themselves. Pathophysiology of c.c 200 virus can cause c.c but the majority of cases are caused by rhinovirus Others: adenovirus, echovirus, respiratory syncytial virus. Viral and bacterial co-inf. is rare. Infected cells will enhance inflammatory process which result in vasodilatation, glandular secretion, sneez and cough reflexes viral inf. ends once enough neutralizing antibodies leaks into mucosa to end viral replication. Clinical picture cl.p appears 1-3 days after inf. 1st symptom sore throat 2nd nasal symptom 3rd cough (infrequent) 20% low grade fever Complication These are rare: sinusitis otitis media bronchitis bacterial pneumonia exacerbation of asthma and COPD Differentiation between c.c & other respiratory disorders Influenza: Myalgia, arthralgia, fever, fatigue. -
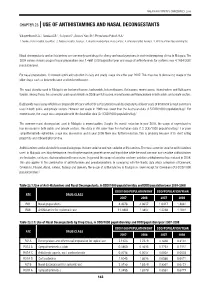
Chapter 23 |Use of Antihistamines and Nasal
MALAYSIAN STATISTICS ON MEDICINES 2008 CHAPTER 23 | USE OF ANTIHISTAMINES AND NASAL DECONGESTANTS Valuyeetham K.A.1, Saraiza A.B.2, Suliyana Y.3, Aswani Yanti B.4, Primuharsa PutraS.H.A.5 1. Tuanku Ja’afar Hospital, Seremban, 2. Serdang Hospital, Selangor, 3. Hospital Kuala Lumpur, Kuala Lumpur, 4. AmpangHospital, Selangor, 5. KPJ Seremban Specialist Hospital. Nasal decongestants and antihistamines are commonly used drugs for allergy and nasal symptoms in otorhinolaryngology clinics in Malaysia. The 2008 survey showed usage of nasal preparations was 1.4881 DDD/population/year and usage of antihistamines for systemic was 4.1654 DDD/ population/year. For nasal preparations, it showed significant reduction in daily and yearly usage since the year 2007. This may due to decreasing usage of the older drugs such as betamethasone and beclomethasone. The nasal steroids used in Malaysia are beclomethasone, budesonide, betamethasone, fluticasone, mometasone, triamcinolone and fluticasone furoate. Among these, the commonly used nasal steroids in 2008 are fluticasone, mometasone and triamcinolone in both public and private sectors. Budesonide nasal spray which has comparable efficacy with other corticosteroid nasal decongestants at lower costs of treatment is most commonly used in both public and private sectors. However our usage in 2008 was lower than the Australian data (1.5 DDD/1000 population/day)1. For mometasone, the usage was comparable with the Australian data (0.4 DDD/1000 population/day).1 The common nasal decongestant used in Malaysia is oxymetazoline. Despite the overall reduction in year 2008, the usage of oxymetazoline has increased in both public and private sectors. This data is still lower than the Australian data (1.2 DDD/1000 population/day).1 For plain sympathomimetic ephedrine, usage was uncommon and in year 2008 there was further reduction. -

Consultation Submission: OTC Nasal Decongestant Preparations For
05 May 2014 RASML Officer OTC Medicines Evaluation Office of Medicines Authorisation Therapeutic Goods Administration PO Box 100 WODEN ACT 2606 Dear Sir/Madam, Re: OTC nasal decongestant preparations for topical use - proposed advisory statements for labelling Novartis Consumer Health (NCH) is the manufacturer and distributor of Otrivin® containing xylometazoline hydrochloride as the active ingredient. We appreciate the opportunity to respond to the consultation on the proposed advisory statements for OTC nasal decongestant preparations for topical use. Our comments on the proposed Required Advisory Statements for Medicine Labels (RASML) are discussed below. 1. Proposed advisory statement: "Frequent or prolonged use may cause nasal congestion to recur or worsen." NCH supports this advisory statement, as it provides clear information for consumers on why the medicine should not be used more frequently or longer than directed. 2. Proposed advisory statement: "Do not use for more than three days at a time unless advised by a doctor or pharmacist." NCH proposes to amend this statement to "Do not use for more than three five days at a time unless advised by a doctor or pharmacist." We agree that consumers need clear instructions on the maximum duration of use. However, the recommendation for 3 days is inconsistent with the body of clinical evidence and Australian standard reference texts. Clinical evidence Topical nasal decongestants are widely used to alleviate symptoms of rhinitis. These products are very effective at rapidly improving nasal congestion1, a symptom which may in turn cause insomnia, snoring and disturbed sleep1,2. Current evidence suggests prolonged or repeated use of topical decongestants can cause problems, leading to the development of rhinitis medicamentosa (RM), commonly known as rebound congestion. -

Rhinitis: Allergic & Non-Allergic
Schiffert Health Center www.healthcenter.vt.edu Rhinitis: Allergic & Non-allergic Rhinitis 101 immune system’s response to small airborne particles Rhinitis is a condition that affects nearly everyone called allergens. Your immune system may identify at some point in life. Symptoms of rhinitis include dust mites, for example, as an allergen. This triggers nasal discharge, drainage, itching, sneezing, and the production of antibodies called IgE, which in turn congestion. Rhinitis can be allergic (AR) or non- trigger cells to release chemicals like histamine. It is allergic (NAR) and affects 10-40% of the population in these chemicals that cause your sneezing, stuffy industrialized countries. nose, and the like. Risk factors for AR include a Acute rhinitis is often caused by cold or flu personal or family history of allergies, asthma, or viruses, as well as allergic reactions to various eczema. Most cases of AR begin before 20yo. allergens. Other causes of rhinitis include Non-allergic/Vasomotor Rhinitis (NAR) medications, hormones (pregnancy/lactation), hot/ NAR can be inflammatory or non-inflammatory, spicy foods, temperature/weather, and irritant. Viral and both types have a component of complex rhinitis is generally self-limited (gets better within a autonomic nervous system reflexes. Triggers of NAR couple of weeks.) Most sinus infections are actually symptoms include environmental and respiratory caused by viruses; however, some are bacterial and irritants (i.e. cigarette/fireplace/stove smoke, car may require antibiotic therapy. Nasal polyps, large exhaust, dust), weather changes (cold air), changes adenoids, or a deviated nasal septum may cause long in humidity, hot/spicy food, alcohol, strong odors -term or worsening symptoms.