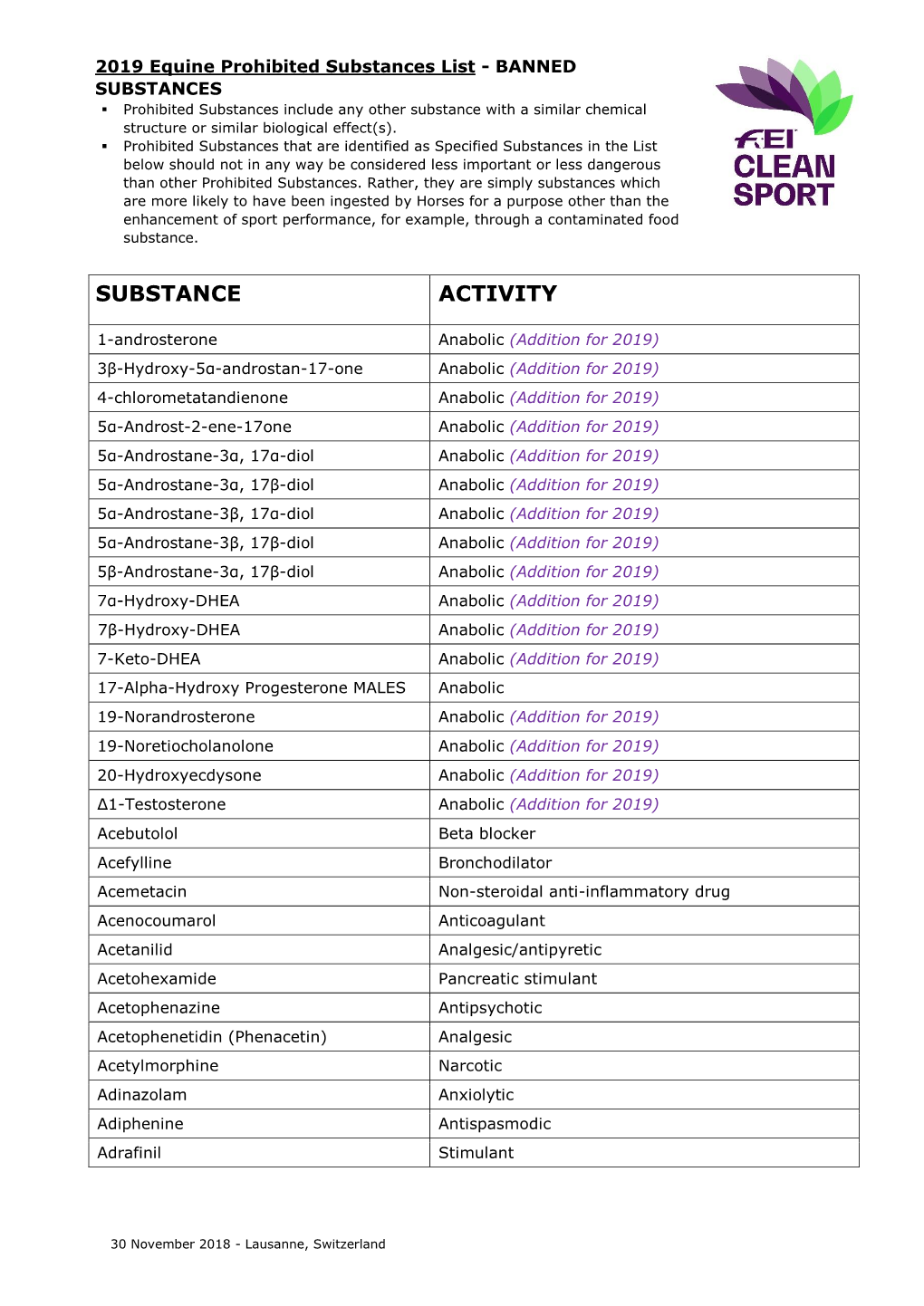
Substance Activity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kava (Piper Methysticum) and Its Methysticin Constituents Protect Brain Tissue Against Ischemic Damage in Rodents
5 Refs: Arletti R et al, Stimulating property of Turnera diffusa and Pfaffia paniculata extracts on the sexual-behavior of male rats. Psychopharmacology 143(1), 15-19, 1999. Berger F, Handbuch der drogenkunde . Vol 2, Maudrich, Wien, 1950. Martinez M, Les plantas medicinales de Mexico . Cuarta Edicion Botas Mexico , p119, 1959. Tyler VE et al, Pharmacognosy , 9 th edition, Lea & Febiger, Philadelphia, 1988. KAVA ( Piper methysticum ) - A REVIEW The Kava plant (Piper methysticum) is a robust, well-branching and erect perennial shrub belonging to the pepper family (Piperaceae). The botanical origin remains unknown, although it is likely that early Polynesian explorers brought the plant with them from island to island. Numerous varieties of Kava exist, and today it is widely cultivated in several Pacific Island countries both for local use as well as the rapidly growing demand for pharmaceutical preparations. The dried rhizomes (roots) are normally used. The first description to the western world of the ceremonial use of an intoxicating beverage prepared from Kava was made by Captain James Cook following his Pacific voyage in 1768. The drink, prepared as an infusion in an elaborate manner after first chewing the root, is consumed on formal occasions or meetings of village elders and chiefs, as well as in reconciling with enemies and on a more social basis. It remains an important social custom in many Pacific Island countries today. Most of the islands of the Pacific possessed Kava prior to European contact, particularly those encompassed by Polynesia, Melanesia and Micronesia. After drinking the Kava beverage a pleasantly relaxed and sociable state develops, after which a deep and restful sleep occurs. -

Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers with Topical Pharmaceutical Agents
Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Author Watts, Annabelle M, Cripps, Allan W, West, Nicholas P, Cox, Amanda J Published 2019 Journal Title FRONTIERS IN PHARMACOLOGY Version Version of Record (VoR) DOI https://doi.org/10.3389/fphar.2019.00294 Copyright Statement © Frontiers in Pharmacology 2019. The attached file is reproduced here in accordance with the copyright policy of the publisher. Please refer to the journal's website for access to the definitive, published version. Downloaded from http://hdl.handle.net/10072/386246 Griffith Research Online https://research-repository.griffith.edu.au fphar-10-00294 March 27, 2019 Time: 17:52 # 1 REVIEW published: 29 March 2019 doi: 10.3389/fphar.2019.00294 Modulation of Allergic Inflammation in the Nasal Mucosa of Allergic Rhinitis Sufferers With Topical Pharmaceutical Agents Annabelle M. Watts1*, Allan W. Cripps2, Nicholas P. West1 and Amanda J. Cox1 1 Menzies Health Institute Queensland, School of Medical Science, Griffith University, Southport, QLD, Australia, 2 Menzies Health Institute Queensland, School of Medicine, Griffith University, Southport, QLD, Australia Allergic rhinitis (AR) is a chronic upper respiratory disease estimated to affect between 10 and 40% of the worldwide population. The mechanisms underlying AR are highly complex and involve multiple immune cells, mediators, and cytokines. As such, the development of a single drug to treat allergic inflammation and/or symptoms is confounded by the complexity of the disease pathophysiology. Complete avoidance of allergens that trigger AR symptoms is not possible and without a cure, the available therapeutic options are typically focused on achieving symptomatic relief. -

Alternative Treatments for Depression and Anxiety
2019 PCB Conference: Strickland Benzodiazepines (BZDs), Herbal and Alternative Treatments for Anxiety & Depression BZD Learning Objectives • List at least three uses for benzodiazepines • Discuss at least two risk factors associated with benzodiazepine prescriptions Craig Strickland, PhD, Owner Biobehavioral Education and Consultation https://sites.google.com/site/bioedcon 1 2 BZD Pharmacokinetics Clinical Uses of BZDs Generic Name Trade Name Rapidity ½ Life Dose (mg) • Treat a variety of anxiety disorders alprazolam Xanax Intermediate Short 0.75-4 • Hypnotics • Muscle relaxants chlordiaze- Librium Intermediate Long 15-100 poxide • To produce anterograde amnesia clonazepam Klonopin Intermediate Long 0.5-4 • Alcohol & other CNS depressant withdrawal • Anti-convulsant therapy diazepam Valium Rapid Long 4-40 triazolam Halcion Intermediate Very short 0.125-0.5 temazepam Restoril Short Short 7.5-30 3 4 1 2019 PCB Conference: Strickland Issues with BZDs Herbal Medication and Alternative Therapies Used in the Treatment of Depression and Anxiety • Addictive potential • Confusion between “anti-anxiety” effects and the “warm-fuzzy) • Large dose ranges • Comparison of BZDs with medications like Buspar, etc. • They work, they work well and they work quickly 5 6 Alternative Tx. Learning Objectives Background Information on herbals: Natural does not necessarily mean “safe” • List several amino acid treatments for depression • Side-effects and adverse reactions • List at least three of the most common herbal – Herbal medications are “drugs” although -

Could Mycolactone Inspire New Potent Analgesics? Perspectives and Pitfalls
toxins Review Could Mycolactone Inspire New Potent Analgesics? Perspectives and Pitfalls 1 2 3, 4, , Marie-Line Reynaert , Denis Dupoiron , Edouard Yeramian y, Laurent Marsollier * y and 1, , Priscille Brodin * y 1 France Univ. Lille, CNRS, Inserm, CHU Lille, Institut Pasteur de Lille, U1019-UMR8204-CIIL-Center for Infection and Immunity of Lille, F-59000 Lille, France 2 Institut de Cancérologie de l’Ouest Paul Papin, 15 rue André Boquel-49055 Angers, France 3 Unité de Microbiologie Structurale, Institut Pasteur, CNRS, Univ. Paris, F-75015 Paris, France 4 Equipe ATIP AVENIR, CRCINA, INSERM, Univ. Nantes, Univ. Angers, 4 rue Larrey, F-49933 Angers, France * Correspondence: [email protected] (L.M.); [email protected] (P.B.) These three authors contribute equally to this work. y Received: 29 June 2019; Accepted: 3 September 2019; Published: 4 September 2019 Abstract: Pain currently represents the most common symptom for which medical attention is sought by patients. The available treatments have limited effectiveness and significant side-effects. In addition, most often, the duration of analgesia is short. Today, the handling of pain remains a major challenge. One promising alternative for the discovery of novel potent analgesics is to take inspiration from Mother Nature; in this context, the detailed investigation of the intriguing analgesia implemented in Buruli ulcer, an infectious disease caused by the bacterium Mycobacterium ulcerans and characterized by painless ulcerative lesions, seems particularly promising. More precisely, in this disease, the painless skin ulcers are caused by mycolactone, a polyketide lactone exotoxin. In fact, mycolactone exerts a wide range of effects on the host, besides being responsible for analgesia, as it has been shown notably to modulate the immune response or to provoke apoptosis. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

Diazepam and Kava Combination Article
Journal of Advanced Research (2014) 5, 587–594 Cairo University Journal of Advanced Research ORIGINAL ARTICLE Enhanced efficacy and reduced side effects of diazepam by kava combination Rasha A. Tawfiq a, Noha N. Nassar b,*, Wafaa I. El-Eraky c, Ezzeldein S. El-Denshary b a Egyptian Patent Office, Academy of Scientific Research and Technology, 101 Kasr El-Eini St., Cairo, Egypt b Department of Pharmacology and Toxicology, Faculty of Pharmacy, Cairo University, Kasr El-Eini St., Cairo, Egypt c Department of Pharmacology, National Research Center, El-Tahrir St., Giza, Egypt ARTICLE INFO ABSTRACT Article history: The long term use of antiepileptic drugs possesses many unwanted effects; thus, new safe com- Received 2 April 2013 binations are urgently mandated. Hence, the present study aimed to investigate the anticonvul- Received in revised form 18 July 2013 sant effect of kava alone or in combination with a synthetic anticonvulsant drug, diazepam Accepted 15 August 2013 (DZ). To this end, female Wistar rats were divided into two subsets, each comprising 6 groups Available online 22 August 2013 as follows: group (i) received 1% Tween 80 p.o. and served as control, while groups (ii) and (iii) received kava at two dose levels (100 and 200 mg/kg, p.o.). The remaining three groups received Keywords: (iv) DZ alone (10 mg/kg p.o.) or kava in combination with DZ (v) (5 mg/kg, p.o.) or (vi) (10 mg/ Kava kg, p.o.). Results of the present study revealed that kava increased the maximal electroshock Diazepam seizure threshold (MEST) and enhanced the anticonvulsant effect of diazepam following both Anticonvulsant acute and chronic treatment. -

Rhinitis - Allergic (1 of 15)
Rhinitis - Allergic (1 of 15) 1 Patient presents w/ signs & symptoms of rhinitis 2 • Consider other classifi cations of rhinitis DIAGNOSIS No - Please see Rhinitis Is allergic rhinitis - Nonallergic disease confi rmed? management chart Yes 3 ASSESS DURATION & SEVERITY OF ALLERGIC RHINITIS A Non-pharmacological therapy • Allergen avoidance • Patient education VAS <5 VAS ≥5 B Pharmacological therapy B Pharmacological therapy • Antihistamines (oral/nasal), &/or • Corticosteroids (nasal), w/ or without • Corticosteroids (nasal), or • Antihistamines (nasal), or • Cromone (nasal), or • LTRA • Leukotriene receptor antagonists (LTRA)MIMS TREATMENT © See next page Specifi cally for patients w/ asthma Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B167 © MIMS Pediatrics 2020 Rhinitis - Allergic (2 of 15) Previously treated symptomatic Previously treated symptomatic patient (VAS <5) on antihistamines patient (VAS ≥5) on intensifi ed (oral/nasal) &/or corticosteroids (nasal) therapy w/ corticosteroids (nasal) w/ or without antihistamines (nasal) Intermittent Persistent symptoms, symptoms or without allergen w/ allergen exposure exposure B Pharmacological therapy B Pharmacological therapy • Step down or discontinue therapy • Continue or step up therapy Untreated REASSESS DISEASE SEVERITY VAS symptomatic patient DAILY UP TO DAY 3 (VAS <5 or ≥5) 4 CONTINUE Yes THERAPY & STEP EVALUATION VAS <5 DOWN THERAPY1 Improvement of symptoms? No VAS ≥5 B Pharmacological therapy • Step-up therapy REASSESS DISEASE SEVERITY MIMSVAS DAILY UP TO DAY 7 4 Yes EVALUATION VAS <5 Improvement of symptoms? No TREATMENT © VAS ≥5 See next page Continue therapy if symptomatic; consider step-down or discontinuation of therapy if symptoms subside Not all products are available or approved for above use in all countries. -

Kava Kava Extract Is Available from Ashland Chemical Co., Mini Star International, Inc., and QBI (Quality Botanical Ingredients, Inc.)
SUMMARY OF DATA FOR CHEMICAL SELECTION Kava Kava 9000-38-8; 84696-40-2 November 1998 TABLE OF CONTENTS Basis for Nomination Chemical Identification Production Information Use Pattern Human Exposure Regulatory Status Evidence for Possible Carcinogenic Activity Human Data Animal Data Metabolism Other Biological Effects Structure-Activity Relationships References BASIS OF NOMINATION TO THE CSWG Kava kava is brought to the attention of the CSWG because it is a rapidly growing, highly used dietary supplement introduced into the mainstream U.S. market relatively recently. Through this use, millions of consumers using antianxiety preparations are potentially exposed to kava kava. A traditional beverage of various Pacific Basin countries, kava clearly has psychoactive properties. The effects of its long-term consumption have not been documented adequately; preliminary studies suggest possibly serious organ system effects. The potential carcinogenicity of kava and its principal constituents are unknown. INPUT FROM GOVERNMENT AGENCIES/INDUSTRY The U.S. Pharmacopeia is in the process of reviewing kava kava. No decision on preparation of a monograph has been made. SELECTION STATUS ACTION BY CSWG: 12/14/98 Studies requested: - Toxicological evaluation, to include studies of reproductive toxicity and neurotoxicity - Genotoxicity Priority: High Rationale/Remarks: - Significant human exposure - Leading dietary supplement with rapidly growing use - Concern that kava has been promoted as a substitute for ritilin in children - Test extract standardized to 30 percent kavalactones - NCI is conducting studies in Salmonella typhimurium CHEMICAL IDENTIFICATION CAS Registry Number: 9000-38-8 Kava-kava resin (8CI) Chemical Abstract Service Name: 84696-40-2 CAS Registry Number: Pepper (Piper), P. methysticum, ext. Chemical Abstract Service Name: Extract of kava; kava extract; Piper Synonyms and Trade Names: methisticum extract Description: The tropical shrub Piper methysticum is widely cultivated in the South Pacific. -
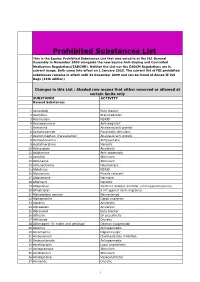
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

7-Nose II.Docx ( Updated F1 )
1 [Color index: Important | Notes | Extra] Editing 2 Diseases of the nose Supernumerary nostril Midline nasal sinus: Nasal clefts: Proboscis lateralis: Incomplete fusion of the right Failure of frontal nasal Due to imperfect fusion and left medial nasal process to develop between the maxillary process prominence. appropriately results into and the lateral nasal process. two separated halves of the nose. Polyrrhinia: Arrhinia: due to bilateral Half nose: due to unilateral absence of nasal placode Duplication of the medial nasal absence of nasal placodes. processes. This is serious because the newborn is a nose breather. mouth breathing is a learning process. Atresia of posterior nares ❖ Types: ● Bony (most commonly) ● Membranous ● Mixed ● Complete unilateral (most commonly) ● Complete bilateral surgical emergency ● Incomplete unilateral ● Incomplete bilateral ❖ Diagnosis: ● Total absence of nasal air flow ● Plastic catheter cannot be passed through the nose ● Post-rhinoscopy ● Radiographs 3 ● Emergency ● Transnasal perforation ● Trans-palatal excision ❖ Management: ﻧﻔﺘﺢ ﻓﻤﻪ ﻓﯿﻀﻄﺮ ﯾﺘﻨﻔﺲ ﻣﻦ ﻓﻤﻪ (Put something to open the mouth (oral airway ● ● Perforate it If membranous ● Surgery (endoscopic) ● In bilateral it is an emergency, in unilateral it is not an emergency and we can wait until the child gains weight then we do surgery. ● Rhinitis refers to inflammatory changes in the nasal mucosa. As the nasal mucosa is continuous over the nose and sinuses, there is nearly always some inflammatory change in the sinuses as 1 well. Hence Rhinosinusitis is a better term. ● Types: - acute rhinitis (less than 4 weeks) - chronic rhinitis (more than four consecutive weeks) ● Types based on etiology: 1) Infectious rhinitis(viral/bacterial) 2)Non-allergic Rhinitis,Non-infectious rhinitis -Eosinophilic syndromes(Nares/Nasal polyposis) -NonEosinophilic syndromes(Vasomotor rhinitis/Rhinitis medicamentosa/occupational rhinitis/Rhinitis of pregnancy/hypothyroidism/Medication(OCP). -

Effects of Low-Dose and Very Low-Dose Ketamine Among Patients with Major Depression
International Journal of Neuropsychopharmacology Advance Access published December 17, 2015 International Journal of Neuropsychopharmacology, 2015, 1–15 doi:10.1093/ijnp/pyv124 Advance Access Publication: November 17, 2015 Review review Effects of Low-Dose and Very Low-Dose Ketamine among Patients with Major Depression: a Systematic Review and Meta-Analysis Downloaded from Ying Xu, Maree Hackett, Gregory Carter, Colleen Loo, Verònica Gálvez, Nick Glozier, Paul Glue, Kyle Lapidus, Alexander McGirr, Andrew A. Somogyi, Philip B. Mitchell, Anthony Rodgers http://ijnp.oxfordjournals.org/ The George Institute for Global Health, The University of Sydney, Sydney, Australia (Drs Xu, Hackett, and Rodgers); Centre for Translational Neuroscience and Mental Health, University of Newcastle, Australia (Dr Carter); School of Psychiatry, University of New South Wales & Black Dog Institute, Sydney, Australia (Drs Loo, Gálvez, and Mitchell); Brain and Mind Research Institute, University of Sydney, Australia (Dr Glozier); Department of Psychiatry, University of Otago, New Zealand (Dr Glue); Departments of Psychiatry and Neurobiology, Stony Brook University, Stony Brook, NY (Dr Lapidus); Department of Psychiatry, University of British Colombia, Canada (Dr McGirr); Discipline of Pharmacology, Faculty of Health Sciences, The University of Adelaide, Adelaide, Australia (Dr Somogyi). by Karin Lavoie on April 20, 2016 Correspondence: Colleen Loo, MD, School of Psychiatry, University of New South Wales & Black Dog Institute, Sydney, Australia ([email protected]). Abstract Background: Several recent trials indicate low-dose ketamine produces rapid antidepressant effects. However, uncertainty remains in several areas: dose response, consistency across patient groups, effects on suicidality, and possible biases arising from crossover trials. Methods: A systematic search was conducted for relevant randomized trials in Medline, Embase, and PsycINFO databases up to August 2014. -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented.