Full PDF Issue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Effects of State Succession on Cultural Property: Ownership, Control, Protection
Department of Law The Effects of State Succession on Cultural Property: Ownership, Control, Protection Andrzej Jakubowski Thesis submitted for assessment with a view to obtaining the degree of Doctor of Laws of the European University Institute Florence, May 2011 2 EUROPEAN UNIVERSITY INSTITUTE Department of Law The Effects of State Succession on Cultural Property: Ownership, Control, Protection Andrzej Jakubowski Thesis submitted for assessment with a view to obtaining the degree of Doctor of Laws of the European University Institute Examining Board: Prof. Francesco Francioni, European University Institute (Supervisor) Prof. Ernst-Ulrich Petersmann, European University Institute Prof. Kurt Siehr, Max-Planck-Institute for Comparative and International Private Law Prof. Władysław Czapliński, Polish Academy of Sciences © 2011, Andrzej Jakubowski No part of this thesis may be copied, reproduced or transmitted without prior permission of the author 1 2 Acknowledgments It is a pleasure to acknowledge the input and assistance that I have received in the writing of this dissertation. Research for this study has been possible by a Polish national grant at the Law Department of the European University Institute, which provided me with excellent institutional support. I would also like to acknowledge the assistance of the Max-Planck Institute for Comparative and Private International Law in Hamburg, and the Max-Planck Institute for Comparative Public Law and International Law in Heidelberg. I am very fortunate to have been able to receive guidance from my supervisor, Francesco Francioni, who constantly encouraged me in my research and showed me what academic excellence and professionalism stand for. I am whole heartedly thankful for his patience, support and enthusiasm. -

At War's End: Allied Forces at Bergen-Belsen Mark
AT WAR'S END: ALLIED FORCES AT BERGEN-BELSEN * MARK CELINSCAK A DISSERTATION SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY GRADUATE PROGRAM IN HUMANITIES YORK UNIVERSITY TORONTO, ONTARIO APRIL 2012 © Mark Celinscak, 2012 Library and Archives Bibliotheque et Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington Ottawa ON K1A0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-90347-6 Our file Notre reference ISBN: 978-0-494-90347-6 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, preter, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distrbute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriete du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette these. Ni thesis. Neither the thesis nor la these ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent etre imprimes ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

Newsletter Jabez Olmsted of Ware
NEWSLETTER JABEZ OLMSTED OF WARE Volume 7, Issue 2 April 2004 PURPOSE The purpose of this newsletter is to facilitate the exchange of research information among Jabez descendants Published and and to encourage and assist with ongoing research. Edited by : Carlton O. Hommel JOE BARBER’S COLUMN As I sit down to write this message, I lines in North America are all related. Summer Address am hoping for spring. Even though we 68 Leisure Lane Frye Island, ME 04071 spent January in Apache Junction, AZ In Volume 6, Issue 2 (May 2003) Doreen Dol- 207-655-7175 it seems like the winter of 2003/4 has leman wrote about using the Google search en- been pretty long. gine for online searching. As well as searching Winter Address by name and place you can also search by 5903 Princess Diana Ct. My research continues at a steady newspaper, as many newspapers have archived Leesburg, FL 34748 pace. Highlights in the past few and indexed their obituary notices. The period 352-315-4324 months have been making contact with of time such archiving and indexing covers var- three new kin and the exchange of in- ies from newspaper to newspaper and can vary [email protected] formation that has taken place. from a number of months to several years. I (Note Change) have found obituaries to be a good source of A descendant of Israel (son of Capt. genealogical information. Newspapers that AND Jabez) has recently undergone Y- carry birth announcements may also archive chromosome DNA testing. His results and index these announcements. -

April 1982 the Newsletter^^^ United States Department of State
The Newsletter^^^ United States Department of State April 1982 THE COVER—You’re looking at a platter that, sooner or later, will be playing back that cable you drafted, or typed, or cleared, or read, or whatever. Bye-bye, Mr. File Drawer, Mr. File Drawer, Mr. File Drawer, Mr. File Drawer, Mr. File Dr. And poof to you, Mr. Terrorist! (Story on Page 2.) Letters to April 1982 the Editor State No. 244 ‘Hi! Hayward here!’ Jerusalem Dear Sir: It has now been almost a year Since I left my post “there” to come “here.” But if State does not show it How can my friends know it? I’ve become a non-person, I fear. I’ve probably never been missed But I’d like to get back on your list. So please report I’ve left Egypt For I don’t want to be gypped. News stories 41 Steigman discusses I’m in Jerusalem now, I insist! 12 Selwa Roosevelt is “senior surplus” Yours sincerely, chief of protocol Martha Haywvrd 12 Marvin Garrett named Photo stories US. consulate general security chief 17 Hail and farewell (Since May 1981) ■ 13 Milam wins $5,000 28 It’s about time 32 Med lab week Be a blood donor Dunn Award Be a blood donor, if you can 18 More acquisitions for Departments and features And plan to give on the day reception rooms 35 Alcohol 1 Letters to Editor When the Department sponsors its 25 Department meets ’81 Awareness 64 Library Booklist Bloodmobile: hiring goals 48 "American 59 Look-Alikes You will haw helped in a great big way. -

Canadian Policy Research Networks Inc
Frontline Health Care in Canada: Innovations in Delivering Services to Vulnerable Populations David Hay Judi Varga-Toth Emily Hines Research Report F|63 Family Network September 2006 Canadian Policy Research Networks Inc. 600 – 250 Albert Street, Ottawa, Ontario K1P 6M1 Tel: (613) 567-7500 Fax: (613) 567-7640 Web Site: www.cprn.org Frontline Health Care in Canada: Innovations in Delivering Services to Vulnerable Populations By David Hay Judi Varga-Toth Emily Hines September 2006 © Canadian Policy Research Networks Inc. Contents Executive Summary .................................................................................................. iii 1. Introduction and Overview ............................................................................ 1 2. Research Questions and Methods ............................................................... 3 3. Profiling the People on the Frontlines .......................................................... 4 3.1 Rural Populations in Canada ............................................................................... 4 3.1.1 What Is Defined as Rural, Remote, Northern? ....................................... 4 3.1.2 Health Status of Rural, Remote and Northern Canadians ...................... 5 3.1.3 Access to Health Care in Rural Canada ................................................. 6 3.2 Inner City and Marginalized Populations in Canada .......................................... 10 3.2.1 What Is Defined as Inner City? ............................................................... 10 3.2.2 -

Beyond Freefall: Halting Rural Poverty
BEYOND FREEFALL: HALTING RURAL POVERTY Final Report of the Standing Senate Committee on Agriculture and Forestry The Honourable Joyce Fairbairn, P.C. Chair The Honourable Leonard J. Gustafson Deputy Chair June 2008 Ce rapport est aussi disponible en français Available on the Parliamentary Internet: www.parl.gc.ca (Committee Business — Senate — Reports) 39th Parliament — 2nd Session BEYOND FREEFALL: HALTING RURAL POVERTY TABLE OF CONTENTS MEMBERS.........................................................................................................................5 ORDER OF REFERENCE................................................................................................. 6 ACKNOWLEDGEMENTS................................................................................................ 7 EXECUTIVE SUMMARY ................................................................................................ 9 SUMMARY OF RECOMMENDATIONS ...................................................................... 23 PREFACE......................................................................................................................... 35 SECTION I: PUTTING RURAL CANADA BACK ON THE POLICY AGENDA............ 1 CHAPTER 1: THE NEED FOR A RURAL VISION........................................................ 1 Why Does Rural Canada Matter? ............................................................................... 3 What do we Want Rural Canada to Look Like? ......................................................... 6 Five principals to guide -

A Memo.Rial History
A MEMO.RIAL HISTORY OF JiVHlCH INCLUDES RECORDS OF THE DIFFERENT HIGHLAND AND OTHER FAlllflLIES. vVJTH WHOM THEY HA VE INTERMARRIED. \ 1 0 c·..., ~ \ 1 I I _ "AIR A' CHUIDEACHD CHAOMH SO DH' FHALBH UAll\I. 71 "OF THE GREAT AND GOOD WHO ARE GONE." GAELIC SONG. :lJrintea for ~uhsr.ril.T.ers antr :tarHntf£ 01irrulation. L01VDON: SilVIl\iONS & BOTTEN, SHOE LANE, E.C. I 882. 1----,_ ' . ····-····---. ·-· ... ___ - ··-··--- ·····-··· ·- . - :: ··-·-·--- --"-~:::;]-" :=={:=_:_-:~~~~-: cC::= i : ·- - - -~ TH·E ·PASS OF MELFORT-.. PREF ACE. desire to preserve s·ome record or memorial of the origin and _descent of the Family of Campbell of Melfort, has been inspired by the wish to perpetuate the noble and _patriotic duty of a_ race during all time remarkable for their fidelity to their sovereign and to the chief of their clan. We are instructed by the Highest Authority that the glory of children are their fathers ; in this belief, and in expressing the hope that the honourable devotion to duty in the past may be emulated in future generations, I have been induced to undertake this labour of love, and_ to collate the materials I ha':.e put on record. In my researches, finding frequent mention of intermarriages between the families of Campbells of Melfort, Achalader, Barcaldine, Lochend, Kinloch, Dunstaffnage, and Duntroon, MacDougall of MacDougall, Maclachlan of Maclachlan, and Cameron of Lochiel, I thought it might interest were some mention of each included in this memorial of the M elfort family. In bidding my worthy" clansmen and fair clanswomen farewell, I do so with hearty thanks for their sympathy in my labours, wishing prosperity and happiness to all who may be sufficiently interested to devote a mom·ent to the perusal of these, I fear, but imperfect records of a family, whose lands, now possessed by strangers, might otherwise B . -

Annual Report 2010 | 2011
ANNUAL REPORT 2010 | 2011 CANADIAN MUSEUM OF CIVILIZATION | CANADIAN WAR MUSEUM Information and Services: 819-776-7000 / 1-800-555-5621 CANADIAN Teletype (TTY): 819-776-7003 Group Reservations: 819-776-7014 Facility Rentals: 819-776-7018 MUSEUM OF Membership: 819-776-7100 Volunteers: 819-776-7011 CIVILIZATION Financial Support for the Corporation: 819-776-7016 Publications: 819-776-8387 Cyberboutique: cyberboutique.civilization.ca CORPORATION Friends of the Canadian War Museum: 819-776-8618 100 Laurier Street, Gatineau, Quebec, K1A 0M8 Published by Corporate Communications, www.civilization.ca Public Affairs and Publishing Design by: Stéphane Breton Cat. no. NM20-1/2011E-PDF ISSN 1495-1886 © CMCC 1 Vimy Place, Ottawa, Ontario, K1A 0M8 www.warmuseum.ca Steven Darby IMG2011-0101-0016-Dm William Kent IMG2011-0101-0032-Dm Steven Darby IMG2008-0187-0002-Dm Marie-Louise Deruaz IMG2010-0167-0003-Dm Marie-Louise Deruaz IMG2011-0101-0038-Dm Marie-Louise Deruaz IMG2009-0063-0021-Dm Steven Darby IMG2011-0101-0018-Dm Marie-Louise Deruaz IMG2011-0101-0004-Dm Steven Darby IMG2011-0101-0019-Dm William Kent IMG2011-0101-0026-Dm Steven Darby IMG2011-0101-0017-Dm Marie-Louise Deruaz IMG2009-0063-0124-Dm 5 TABLE OF CONTENTS 04 Corporation Highlights 06 Museum of Civilization Highlights 08 War Museum Highlights 10 Message from the Chair 11 Message from the President and CEO 14 THE MUSEUMS 15 Exhibitions 24 Artifact Collections 32 Research 36 Public Programs 43 Websites and Publishing 47 Public Affairs 51 THE CORPORATION 52 Mandate and Guiding Principles -
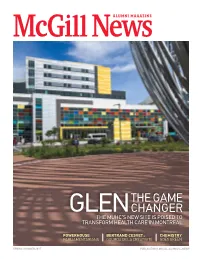
The GAME Changer
ALUMNI MAGAZINE THE GAME GLEN CHANGER THE MUHC’S NEW SITE IS POISED to TRANSFORM HealtH CARE IN MONTREAL POWERHOUSE BERTRAND CESVET : CHEMISTRY PARLIAMENTARIANS GOUROU DE LA CRÉATIVITÉ GOES GREEN SPRING /SUMMER 2015 PUBLICATIONS.MCGILL.CA/MCGILLNEWS Chart the best course for your life in the years ahead. Start with preferred insurance rates. Supporting you... On average, alumni and McGill University. who have home and auto Your needs will change as your life and career evolve. As a McGill University Alumni insurance with us Association member, you have access to the save $400.* TD Insurance Meloche Monnex program, which offers preferred insurance rates, other discounts and great protection, that is easily adapted to your changing needs. Plus, every year our program contributes to supporting your alumni association, so it’s a great way to save and show you care at the same time. Get a quote today! Our extended business hours make it easy. Monday to Friday: 8 a.m. to 8 p.m. Home and auto insurance program recommended by the Saturday: 9 a.m. to 4 p.m. HOME | AUTO | TRAVEL Ask for your quote today at 1-888-589-5656 or visit melochemonnex.com/mcgillalumni Average based on the home and auto premiums for active policies on July 31, 2014 of our Alberta clients who belong to a professional or alumni group that has an agreement with us when compared to the premiums they would have paid with the same insurer without the preferred insurance rate for groups and the multi-product discount. Savings are not guaranteed and may vary based on the client’s profile. -

Index Index 1105
INDEX INDEX 1105 A Mya Lay, U, 609 Abdel Rahman ai-Irani, 1077 Abdul-Hossein Mirza Farman Farma, 467 Aandahl, Fred, 1020 Abdel Sabra, 1078 Abdul Jailul Akhbar (Brunei), 181 Ab Egg, Alfred, 865 Abdelahi Mohammed, 253 Abdul Jailul Jabbar (Brunei), 181 Aba, Edward, 683 Abdelazziz Bouteflika, 60 Abdul Jalil Saif an-Nasr, 536 Ablicherli, Alois, 886 Abdelhamid Brahimi, 60 Abdul Jalil Shah, 556 Abadie, Henry, 958 Abdellatif Filali, 603 Abdul Jalloud, 535 Abaijah, Josephine, 680 Abdelmalek Benhabyles, 60 Abdul Jamil bin Rais, 559 Abarca Alcaron, Raimundo, 580 Abdelmuhsin al-Sudeary, 44 Abdul Kadir Sheikh, 669 Abashidze, Asian, 362 Abderrahman Khene, 32 Abdul Kahar, 181 Abayev, Solomon, 735 Abderrahman (Morocco), 602 Abdul Karami, 528 Abba Gana Terab, 642 Abdessalam Bussairy, 536 Abdul Karim I (Lahej), 1082 Abba Kyari, 647 Abdic, Fikret, 146 Abdul Karim II (Lahej), 1083 Abba Musa Rimi, 647 Abdirashid Shermarke, 797 Abdul Kassem, 471 Abbas Djoussouf, 253 Abdoh, Djalal, 464 Abdul Kubar, 535 Abbas I (Egypt), 302 Abdou Mohammed Hussain, 254 Abdul Mackawee, 1080 Abbas I (Iran), 466 Abdou Mohammed Mindhi, 254 Abdul Mahid bin Yusof, 551 Abbas II (Egypt), 302 Abdoulaye Souley, 634 Abdul Majid Didi, 562 Abbas II (Iran), 466 Abdrazyakov, Abdulkhak, 738 Abdul Majid Didi (Maldives), 561 Abbas III (Iran), 466 Abdu Bako, 648 Abdul-Majid Mirza Ayn od-Dowleh, 467 Abbas Khalatbary, 7 Abdukarimov, Isatai, 507 Abdul Majid (Turkey), 930 Abbasi, S.M., 669 Abdul Adisa, 654 Abdul Malek bin Yusuf, 553 Abbe, Godwin, 640, 655 Abdul Ajib bin Ahmed, 552 Abdul Malik bin Yusof, -

T8.3.2 English Maclellan
Second World War Discovery Box Personal Stories Keith MacLellan Canadian Army When Keith was 25, he witnessed the horrors of war while helping to liberate the notorious Bergen-Belsen concentration camp. Studio portrait of Keith MacLellan Courtesy of the MacLellan family Early Years Born in Aylmer, Quebec, in 1920, Keith Political Science and pre-law. While at McGill, William MacLellan grew up in Montréal. He he joined the Canadian Officer Training Corps. attended McGill University, where he took warmuseum.ca/supplyline Keith MacLellan 1 Witness to the Horrors of War Putting his academic studies on hold, Keith On 15 April 1945, Keith’s unit reached joined the Royal Montreal Regiment, and Bergen-Belsen — a Nazi concentration camp — became an officer in the Canadian Army. before other Allied troops in the area arrived. He was sent overseas, arriving in England He was one of the first Allied soldiers to enter in February 1944. the camp, and the first Canadian. In September 1944, he joined the Special Air Inside, he found unimaginable horrors. In Service, an elite special forces unit within the addition to countless dead, both unburied and British Army. Parachuting into northwestern in mass graves, there were tens of thousands Europe in November 1944, he took part of sick and starving inmates, many of whom in secret operations behind enemy lines, could not be saved. It was at Belsen, just weeks ahead of advancing Allied forces. During his before the Allies entered, that Anne Frank service, he undertook missions in Belgium, (whose wartime diary was later published) the Netherlands, Germany, and Norway.