Mechanisms of Cancer Pain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidline for the Evidence-Informed Primary Care Management of Low Back Pain
Guideline for the Evidence-Informed Primary Care Management of Low Back Pain 2nd Edition These recommendations are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances. They should be used as an adjunct to sound clinical decision making. Guideline Disease/Condition(s) Targeted Specifications Acute and sub-acute low back pain Chronic low back pain Acute and sub-acute sciatica/radiculopathy Chronic sciatica/radiculopathy Category Prevention Diagnosis Evaluation Management Treatment Intended Users Primary health care providers, for example: family physicians, osteopathic physicians, chiro- practors, physical therapists, occupational therapists, nurses, pharmacists, psychologists. Purpose To help Alberta clinicians make evidence-informed decisions about care of patients with non- specific low back pain. Objectives • To increase the use of evidence-informed conservative approaches to the prevention, assessment, diagnosis, and treatment in primary care patients with low back pain • To promote appropriate specialist referrals and use of diagnostic tests in patients with low back pain • To encourage patients to engage in appropriate self-care activities Target Population Adult patients 18 years or older in primary care settings. Exclusions: pregnant women; patients under the age of 18 years; diagnosis or treatment of specific causes of low back pain such as: inpatient treatments (surgical treatments); referred pain (from abdomen, kidney, ovary, pelvis, -

Clinical Data Mining Reveals Analgesic Effects of Lapatinib in Cancer Patients
www.nature.com/scientificreports OPEN Clinical data mining reveals analgesic efects of lapatinib in cancer patients Shuo Zhou1,2, Fang Zheng1,2* & Chang‑Guo Zhan1,2* Microsomal prostaglandin E2 synthase 1 (mPGES‑1) is recognized as a promising target for a next generation of anti‑infammatory drugs that are not expected to have the side efects of currently available anti‑infammatory drugs. Lapatinib, an FDA‑approved drug for cancer treatment, has recently been identifed as an mPGES‑1 inhibitor. But the efcacy of lapatinib as an analgesic remains to be evaluated. In the present clinical data mining (CDM) study, we have collected and analyzed all lapatinib‑related clinical data retrieved from clinicaltrials.gov. Our CDM utilized a meta‑analysis protocol, but the clinical data analyzed were not limited to the primary and secondary outcomes of clinical trials, unlike conventional meta‑analyses. All the pain‑related data were used to determine the numbers and odd ratios (ORs) of various forms of pain in cancer patients with lapatinib treatment. The ORs, 95% confdence intervals, and P values for the diferences in pain were calculated and the heterogeneous data across the trials were evaluated. For all forms of pain analyzed, the patients received lapatinib treatment have a reduced occurrence (OR 0.79; CI 0.70–0.89; P = 0.0002 for the overall efect). According to our CDM results, available clinical data for 12,765 patients enrolled in 20 randomized clinical trials indicate that lapatinib therapy is associated with a signifcant reduction in various forms of pain, including musculoskeletal pain, bone pain, headache, arthralgia, and pain in extremity, in cancer patients. -

Approach to Polyarthritis for the Primary Care Physician
24 Osteopathic Family Physician (2018) 24 - 31 Osteopathic Family Physician | Volume 10, No. 5 | September / October, 2018 REVIEW ARTICLE Approach to Polyarthritis for the Primary Care Physician Arielle Freilich, DO, PGY2 & Helaine Larsen, DO Good Samaritan Hospital Medical Center, West Islip, New York KEYWORDS: Complaints of joint pain are commonly seen in clinical practice. Primary care physicians are frequently the frst practitioners to work up these complaints. Polyarthritis can be seen in a multitude of diseases. It Polyarthritis can be a challenging diagnostic process. In this article, we review the approach to diagnosing polyarthritis Synovitis joint pain in the primary care setting. Starting with history and physical, we outline the defning characteristics of various causes of arthralgia. We discuss the use of certain laboratory studies including Joint Pain sedimentation rate, antinuclear antibody, and rheumatoid factor. Aspiration of synovial fuid is often required for diagnosis, and we discuss the interpretation of possible results. Primary care physicians can Rheumatic Disease initiate the evaluation of polyarthralgia, and this article outlines a diagnostic approach. Rheumatology INTRODUCTION PATIENT HISTORY Polyarticular joint pain is a common complaint seen Although laboratory studies can shed much light on a possible diagnosis, a in primary care practices. The diferential diagnosis detailed history and physical examination remain crucial in the evaluation is extensive, thus making the diagnostic process of polyarticular symptoms. The vast diferential for polyarticular pain can difcult. A comprehensive history and physical exam be greatly narrowed using a thorough history. can help point towards the more likely etiology of the complaint. The physician must frst ensure that there are no symptoms pointing towards a more serious Emergencies diagnosis, which may require urgent management or During the initial evaluation, the physician must frst exclude any life- referral. -

Pathological Cause of Low Back Pain in a Patient Seen Through Direct Margaret M
Pathological Cause of Low Back Pain in a Patient Seen through Direct Margaret M. Gebhardt PT, DPT, OCS Access in a Physical Therapy Clinic: A Case Report Staff Physical Therapist, Motion Stability, LLC, and Adjunct Clinical Faculty, Mercer University, Atlanta, GA ABSTRACT cal therapists primarily treat patients that sporadic.9 Deyo and Diehl6 found that the Background and Purpose: A 66-year- fall into the mechanical LBP category, but 4 clinical findings with the highest positive old male presented directly to a physical need to be aware that although infrequent, likelihood ratios for detecting the presence therapy clinic with complaints of low back 7% to 8% of LBP complaints are due to of cancer in LBP were: a previous history of pain (LBP). The purpose of this case report is nonmechanical spinal conditions or visceral cancer, failure to improve with conservative to describe the clinical reasoning that led to disease.5 Malignant neoplasms are the most medical treatment in the past month, an age a medical referral for a patient not respond- common of the nonmechanical spinal con- of at least 50 years or older, and unexplained ing to conservative treatment that ultimately ditions causing LBP, but comprise less than weight loss of more than 4.5 kg in 6 months led to the diagnosis of multiple myeloma. 1% of all total LBP conditions.6 (Table 1).10 In Deyo and Diehl’s6 study, they Methods: Data was collected during the In this era of autonomous practice, analyzed 1975 patients that presented with course of the patient’s treatment in an out- increasing numbers of physical therapists are LBP and found 13 to have cancer. -
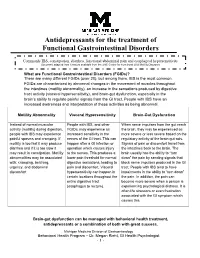
Antidepressants for Functional Gastrointestinal Disorders
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

Managing Cancer Pain
The British Pain Society's Managing cancer pain - information for patients From the British Pain Society, supported by the Association of Palliative Medicine and the Royal College of General Practitioners January 2010 To be reviewed January 2013 2 Cancer Pain Management Published by: The British Pain Society 3rd floor Churchill House 35 Red Lion Square London WC1R 4SG Website: www.britishpainsociety.org ISBN: 978-0-9551546-8-3 © The British Pain Society 2010 Information for Patients 3 Contents Page What can be done for people with cancer pain 4 Understanding cancer pain 4 Knowing what to expect 6 Options for pain control – most pain can be controlled 6 Coping with cancer pain 8 Describing pain – communicating with your doctors 9 Talking to others with cancer pain 12 Finding help managing cancer pain 12 References 12 Methods 12 Competing Interests 13 Membership of the group and expert contributors 13 4 Cancer Pain Management What can be done for people with cancer pain? There are medicines and expertise available that can help to control cancer pain. However, surveys show that cancer pain is still poorly controlled in many cases. As a result, patients must know what is available, what they have a right to and how to ask for it. Cancer itself and the treatments for cancer, including both medicines and surgery, can cause pain. Treatments can be directed either at the cause of the pain (for example, the tumour itself) or at the pain itself. Understanding cancer pain Cancer pain can be complicated, involving pain arising from inflammation (swelling), nerve damage and tissue damage from many sites around the body. -

The IASP Classification of Chronic Pain for ICD-11: Chronic Cancer-Related
Narrative Review The IASP classification of chronic pain for ICD-11: chronic cancer-related pain Michael I. Bennetta, Stein Kaasab,c,d, Antonia Barkee, Beatrice Korwisie, Winfried Riefe, Rolf-Detlef Treedef,*, The IASP Taskforce for the Classification of Chronic Pain Abstract 10/27/2019 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3FlQBFFqx6X+GYXBy6C6D13N3BXo5wGkearAMol2nLQo= by https://journals.lww.com/pain from Downloaded Downloaded Worldwide, the prevalence of cancer is rising and so too is the number of patients who survive their cancer for many years thanks to the therapeutic successes of modern oncology. One of the most frequent and disabling symptoms of cancer is pain. In addition to from the pain caused by the cancer, cancer treatment may also lead to chronic pain. Despite its importance, chronic cancer-related pain https://journals.lww.com/pain is not represented in the current International Classification of Diseases (ICD-10). This article describes the new classification of chronic cancer-related pain for ICD-11. Chronic cancer-related pain is defined as chronic pain caused by the primary cancer itself or metastases (chronic cancer pain) or its treatment (chronic postcancer treatment pain). It should be distinguished from pain caused by comorbid disease. Pain management regimens for terminally ill cancer patients have been elaborated by the World Health Organization and other international bodies. An important clinical challenge is the longer term pain management in cancer patients by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3FlQBFFqx6X+GYXBy6C6D13N3BXo5wGkearAMol2nLQo= and cancer survivors, where chronic pain from cancer, its treatment, and unrelated causes may be concurrent. This article describes how a new classification of chronic cancer-related pain in ICD-11 is intended to help develop more individualized management plans for these patients and to stimulate research into these pain syndromes. -

ASCO Answers: Managing Cancer-Related Pain
Managing Cancer-Related Pain A Guide for Patients, Families, and Caregivers from the American Society of Clinical Oncology ABOUT ASCO Founded in 1964, the American Society of Clinical Oncology, Inc. (ASCO®) is committed to making a world of diference in cancer care. As the world’s leading organization of its kind, ASCO rep- resents nearly 45,000 oncology professionals who care for people living wizth cancer. Through research, education, and promotion of the highest-quality patient care, ASCO works to conquer cancer and create a world where cancer is prevented or cured, and every survivor is healthy. ASCO furthers its mission through Cancer.Net and Conquer Cancer, the ASCO Foundation. Cancer.Net (www.cancer.net) brings the expertise and resources of ASCO to people living with cancer and those who care for and about them. All the information and content on Cancer.Net is developed and approved by members of ASCO, making Cancer.Net an up-to-date and trusted resource for cancer information. Conquer Cancer (www.conquer.org) funds research into every facet of cancer to beneft every patient, everywhere. Conquer Cancer helps turn science into a sigh of relief for patients around the world by supporting groundbreaking research and education across cancer’s full continuum. Learn more at www.ASCO.org. Follow us on Facebook, Twitter, LinkedIn, and YouTube. MILLIONS OF PEOPLE RELY ON CANCER.NET FOR: • Information on 120+ cancer types • Information on navigating cancer care • Coping and survivorship resources GET YOUR CANCER INFORMATION IN THE FORMAT -

An Unusual Cause of Back Pain in Osteoporosis: Lessons from a Spinal Lesion
Ann Rheum Dis 1999;58:327–331 327 MASTERCLASS Series editor: John Axford Ann Rheum Dis: first published as 10.1136/ard.58.6.327 on 1 June 1999. Downloaded from An unusual cause of back pain in osteoporosis: lessons from a spinal lesion S Venkatachalam, Elaine Dennison, Madeleine Sampson, Peter Hockey, MIDCawley, Cyrus Cooper Case report A 77 year old woman was admitted with a three month history of worsening back pain, malaise, and anorexia. On direct questioning, she reported that she had suVered from back pain for four years. The thoracolumbar radiograph four years earlier showed T6/7 vertebral collapse, mild scoliosis, and degenerative change of the lumbar spine (fig 1); but other investigations at that time including the eryth- rocyte sedimentation rate (ESR) and protein electophoresis were normal. Bone mineral density then was 0.914 g/cm2 (T score = −2.4) at the lumbar spine, 0.776 g/cm2 (T score = −1.8) at the right femoral neck and 0.738 g/cm2 (T score = −1.7) at the left femoral neck. She was given cyclical etidronate after this vertebral collapse as she had suVered a previous fragility fracture of the left wrist. On admission, she was afebrile, but general examination was remarkable for pallor, dental http://ard.bmj.com/ caries, and cellulitis of the left leg. A pansysto- lic murmur was heard at the cardiac apex on auscultation; there were no other signs of bac- terial endocarditis. She had kyphoscoliosis and there was diVuse tenderness of the thoraco- lumbar spine. Her neurological examination was unremarkable. on September 29, 2021 by guest. -

Pain Management & Palliative Care
Guidelines on Pain Management & Palliative Care A. Paez Borda (chair), F. Charnay-Sonnek, V. Fonteyne, E.G. Papaioannou © European Association of Urology 2013 TABLE OF CONTENTS PAGE 1. INTRODUCTION 6 1.1 The Guideline 6 1.2 Methodology 6 1.3 Publication history 6 1.4 Acknowledgements 6 1.5 Level of evidence and grade of guideline recommendations* 6 1.6 References 7 2. BACKGROUND 7 2.1 Definition of pain 7 2.2 Pain evaluation and measurement 7 2.2.1 Pain evaluation 7 2.2.2 Assessing pain intensity and quality of life (QoL) 8 2.3 References 9 3. CANCER PAIN MANAGEMENT (GENERAL) 10 3.1 Classification of cancer pain 10 3.2 General principles of cancer pain management 10 3.3 Non-pharmacological therapies 11 3.3.1 Surgery 11 3.3.2 Radionuclides 11 3.3.2.1 Clinical background 11 3.3.2.2 Radiopharmaceuticals 11 3.3.3 Radiotherapy for metastatic bone pain 13 3.3.3.1 Clinical background 13 3.3.3.2 Radiotherapy scheme 13 3.3.3.3 Spinal cord compression 13 3.3.3.4 Pathological fractures 14 3.3.3.5 Side effects 14 3.3.4 Psychological and adjunctive therapy 14 3.3.4.1 Psychological therapies 14 3.3.4.2 Adjunctive therapy 14 3.4 Pharmacotherapy 15 3.4.1 Chemotherapy 15 3.4.2 Bisphosphonates 15 3.4.2.1 Mechanisms of action 15 3.4.2.2 Effects and side effects 15 3.4.3 Denosumab 16 3.4.4 Systemic analgesic pharmacotherapy - the analgesic ladder 16 3.4.4.1 Non-opioid analgesics 17 3.4.4.2 Opioid analgesics 17 3.4.5 Treatment of neuropathic pain 21 3.4.5.1 Antidepressants 21 3.4.5.2 Anticonvulsant medication 21 3.4.5.3 Local analgesics 22 3.4.5.4 NMDA receptor antagonists 22 3.4.5.5 Other drug treatments 23 3.4.5.6 Invasive analgesic techniques 23 3.4.6 Breakthrough cancer pain 24 3.5 Quality of life (QoL) 25 3.6 Conclusions 26 3.7 References 26 4. -

PATIENT FACT SHEET Chronic Recurrent Multifocal Osteomyelitis (CRMO)
PATIENT FACT SHEET Chronic Recurrent Multifocal Osteomyelitis (CRMO) Chronic recurrent multifocal osteomyelitis (CRMO), or thought to be rare, occurring in about 0.4 out of 100,000 chronic nonbacterial osteomyelitis (CNO), is an auto- people per year. As recognition of CRMO is increasing, it inflammatory disorder that causes bone pain due to appears to be more common than that. In fact, CRMO may inflammation in the bones not caused by infection. be nearly as common as bone infections. The average age CONDITION Chronic recurrent multifocal osteomyelitis (CRMO) can that CRMO starts is 9 to 10 years. More girls are affected take months to years to diagnose. CRMO was previously than boys. DESCRIPTION Bone pain is the most common symptom. There is a genetic component. Some families have more than one usually tenderness at the affected site (it hurts to be person with CRMO. pushed on). The pain can cause the person to avoid using CRMO is monitored by following symptoms and imaging the affected body part. Some people with CRMO can studies. MRI is the best way to assess resolution of active develop arthritis (joint swelling). Fatigue is common during bone lesions and/or detect new lesions. active disease. A small fraction of people with CRMO have SIGNS/ SYMPTOMS Treatment of CRMO depends on how severe it is and zoledronic acid). People taking methotrexate and biologic which bones it affects. Treatment usually starts with medications are at a higher risk of infection and should be NSAID medications (ibuprofen, naproxen, meloxicam), evaluated by a doctor if they develop fever or symptoms but some patients need stronger medicines, including of infection. -

Interventional Techniques for Cancer Pain
Interventional Techniques for Cancer Pain Cancer pain may result either from primary or metastatic neoplasms or from invasive or diagnostic procedures. Cancer treatments that may cause pain include surgery, radiation, chemotherapy, immunotherapy, and hormonal therapy. The presentation of pain may depend on etiology; however, it is important to realize that patients with cancer are not immune to pain that commonly occurs in noncancer patients. Cancer pain is typically nociceptive, visceral, or neuropathic, or a combination of these. Interventional techniques targeted to control pain may be appropriate adjuvants or alternatives to oral or systemic pharmacological treatment. These techniques may also be more appropriate in patients who are unable to tolerate side effects of systemic medications. Some examples of interventional techniques are listed below. Intraspinal Analgesia Epidural • Is the most common option for spinal or radicular pain caused by primary or metastatic lesions • Causes lesions that may affect intervertebral disks, nerve roots, or spinal canal size • Provides highly selective pain relief, while producing analgesia over a large area • Targets cervical, thoracic, lumbar, or caudal levels • Allows single injections of a steroid, sometimes with a local anesthetic (e.g., lidocaine or bupivacaine) • Allows continuous infusions of an opioid with a temporary catheter Intrathecal • Provides highly selective pain relief of spinal origin • Allows for minimal side effects typically associated with higher dosages of oral medications