Cannabinoids for the Treatment of Opioid Use Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -

The Opioid Epidemic: What Labs Have to Do with It?
The Opioid Epidemic: What labs have to do with it? Ewa King, Ph.D. Associate Director of Health RIDOH State Health Laboratories Analysis. Answers. Action. www.aphl.org Overview • Overdose trends • Opioids and their effects • Analytical testing approaches • Toxicology laboratories Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 1 Analysis. Answers. Action. www.aphl.org Opioid overdose crisis 2 Analysis. Answers. Action. www.aphl.org Opiates and Opioids • Opiates vs. Opioids • Opiates: Naturally occurring, derived from the poppy plant • Opioids: “Opiate-like” drugs in effects, not chemical structure Includes opiates • Narcotic analgesics • CNS depressants • DEA Schedule I or II controlled substances • Additive effect with other CNS depressant drugs Analysis. Answers. Action. www.aphl.org Efficacy of Opioids • How do opioids work? • Bind with opioid receptors • Brain, spinal cord, GI tract, and throughout the body • Pain, emotion, breathing, movement, and digestion Opioid Receptor Analysis. Answers. Action. www.aphl.org Effects of Opioids Physiological Psychological • Pain relief • Drowsiness/ sedation • Cough suppression • Mental confusion • GI motility • Loss of memory • Respiratory depression • Lethargy/ apathy • Pupillary constriction • Euphoria/ tranquility • Itching • Mood swings • Constipation • Depression • Dependence • Withdrawal • Dependence Analysis. Answers. Action. www.aphl.org Opiates 1 Opiates • Naturally occurring alkaloids Opium • Latex from the opium poppy plant Codeine: • Mild to moderate pain • Antitussive Morphine: • Severe pain • Metabolite of codeine and heroin Analysis. Answers. Action. www.aphl.org Opiates 2 Semi-synthetic Opiates: • Synthesized from a natural opiate Heroin: • Schedule I narcotic Hydrocodone (Vicodin): • Mild to moderate pain • Metabolizes to hydromorphone (Dilaudid) Oxycodone (Oxycontin/Percocet): • Moderate to severe pain • Metabolizes to oxymorphone (Opana) Analysis. Answers. Action. -

ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update
The ASAM NATIONAL The ASAM National Practice Guideline 2020 Focused Update Guideline 2020 Focused National Practice The ASAM PRACTICE GUIDELINE For the Treatment of Opioid Use Disorder 2020 Focused Update Adopted by the ASAM Board of Directors December 18, 2019. © Copyright 2020. American Society of Addiction Medicine, Inc. All rights reserved. Permission to make digital or hard copies of this work for personal or classroom use is granted without fee provided that copies are not made or distributed for commercial, advertising or promotional purposes, and that copies bear this notice and the full citation on the fi rst page. Republication, systematic reproduction, posting in electronic form on servers, redistribution to lists, or other uses of this material, require prior specifi c written permission or license from the Society. American Society of Addiction Medicine 11400 Rockville Pike, Suite 200 Rockville, MD 20852 Phone: (301) 656-3920 Fax (301) 656-3815 E-mail: [email protected] www.asam.org CLINICAL PRACTICE GUIDELINE The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update 2020 Focused Update Guideline Committee members Kyle Kampman, MD, Chair (alpha order): Daniel Langleben, MD Chinazo Cunningham, MD, MS, FASAM Ben Nordstrom, MD, PhD Mark J. Edlund, MD, PhD David Oslin, MD Marc Fishman, MD, DFASAM George Woody, MD Adam J. Gordon, MD, MPH, FACP, DFASAM Tricia Wright, MD, MS Hendre´e E. Jones, PhD Stephen Wyatt, DO Kyle M. Kampman, MD, FASAM, Chair 2015 ASAM Quality Improvement Council (alpha order): Daniel Langleben, MD John Femino, MD, FASAM Marjorie Meyer, MD Margaret Jarvis, MD, FASAM, Chair Sandra Springer, MD, FASAM Margaret Kotz, DO, FASAM George Woody, MD Sandrine Pirard, MD, MPH, PhD Tricia E. -

Opioids and Nicotine Dependence in Planarians
Pharmacology, Biochemistry and Behavior 112 (2013) 9–14 Contents lists available at ScienceDirect Pharmacology, Biochemistry and Behavior journal homepage: www.elsevier.com/locate/pharmbiochembeh Opioid receptor types involved in the development of nicotine physical dependence in an invertebrate (Planaria)model Robert B. Raffa a,⁎, Steve Baron a,b, Jaspreet S. Bhandal a,b, Tevin Brown a,b,KevinSongb, Christopher S. Tallarida a,b, Scott M. Rawls b a Department of Pharmaceutical Sciences, Temple University School of Pharmacy, Philadelphia, PA, USA b Department of Pharmacology & Center for Substance Abuse Research, Temple University School of Medicine, Philadelphia, PA, USA article info abstract Article history: Recent data suggest that opioid receptors are involved in the development of nicotine physical dependence Received 18 May 2013 in mammals. Evidence in support of a similar involvement in an invertebrate (Planaria) is presented using Received in revised form 18 September 2013 the selective opioid receptor antagonist naloxone, and the more receptor subtype-selective antagonists CTAP Accepted 21 September 2013 (D-Phe-Cys-Tyr-D-Trp-Arg-Thr-Pen-Thr-NH )(μ, MOR), naltrindole (δ, DOR), and nor-BNI (norbinaltorphimine) Available online 29 September 2013 2 (κ, KOR). Induction of physical dependence was achieved by 60-min pre-exposure of planarians to nicotine and was quantified by abstinence-induced withdrawal (reduction in spontaneous locomotor activity). Known MOR Keywords: Nicotine and DOR subtype-selective opioid receptor antagonists attenuated the withdrawal, as did the non-selective Abstinence antagonist naloxone, but a KOR subtype-selective antagonist did not. An involvement of MOR and DOR, but Withdrawal not KOR, in the development of nicotine physical dependence or in abstinence-induced withdrawal was thus Physical dependence demonstrated in a sensitive and facile invertebrate model. -

What Are the Treatments for Heroin Addiction?
How is heroin linked to prescription drug abuse? See page 3. from the director: Research Report Series Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year. Although heroin use in the general population is rather low, the numbers of people starting to use heroin have been steadily rising since 2007.1 This may be due in part to a shift from abuse of prescription pain relievers to heroin as a readily available, cheaper alternative2-5 and the misperception that highly pure heroin is safer than less pure forms because it does not need to be injected. Like many other chronic diseases, addiction can be treated. Medications HEROIN are available to treat heroin addiction while reducing drug cravings and withdrawal symptoms, improving the odds of achieving abstinence. There are now a variety of medications that can be tailored to a person’s recovery needs while taking into account co-occurring What is heroin and health conditions. Medication combined with behavioral therapy is particularly how is it used? effective, offering hope to individuals who suffer from addiction and for those around them. eroin is an illegal, highly addictive drug processed from morphine, a naturally occurring substance extracted from the seed pod of certain varieties The National Institute on Drug Abuse (NIDA) has developed this publication to Hof poppy plants. -
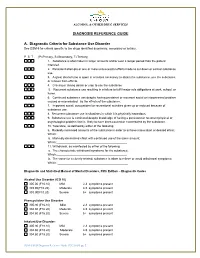
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -

Medications for Opioid Use Disorder for Healthcare and Addiction Professionals, Policymakers, Patients, and Families
Medications for Opioid Use Disorder For Healthcare and Addiction Professionals, Policymakers, Patients, and Families UPDATED 2020 TREATMENT IMPROVEMENT PROTOCOL TIP 63 Please share your thoughts about this publication by completing a brief online survey at: https://www.surveymonkey.com/r/KAPPFS The survey takes about 7 minutes to complete and is anonymous. Your feedback will help SAMHSA develop future products. TIP 63 MEDICATIONS FOR OPIOID USE DISORDER Treatment Improvement Protocol 63 For Healthcare and Addiction Professionals, Policymakers, Patients, and Families This TIP reviews three Food and Drug Administration-approved medications for opioid use disorder treatment—methadone, naltrexone, and buprenorphine—and the other strategies and services needed to support people in recovery. TIP Navigation Executive Summary For healthcare and addiction professionals, policymakers, patients, and families Part 1: Introduction to Medications for Opioid Use Disorder Treatment For healthcare and addiction professionals, policymakers, patients, and families Part 2: Addressing Opioid Use Disorder in General Medical Settings For healthcare professionals Part 3: Pharmacotherapy for Opioid Use Disorder For healthcare professionals Part 4: Partnering Addiction Treatment Counselors With Clients and Healthcare Professionals For healthcare and addiction professionals Part 5: Resources Related to Medications for Opioid Use Disorder For healthcare and addiction professionals, policymakers, patients, and families MEDICATIONS FOR OPIOID USE DISORDER TIP 63 Contents -

The Opioid Crisis and the Black/African American Population: an Urgent Issue
THE OPIOID CRISIS AND THE BLACK/AFRICAN AMERICAN POPULATION: AN URGENT ISSUE THE OPIOID CRISIS AND THE BLACK/AFRICAN AMERICAN POPULATION: AN URGENT ISSUE U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration Office of Behavioral Health Equity Table of Contents Introduction ...................................................................................................................................................... 3 i. Purpose of the Issue Brief ........................................................................................................................ 3 ii. Sources of Information ............................................................................................................................ 4 Opioids in Black/African American Communities: Context .................................................................. 4 i. What Do the National Data Show? ........................................................................................................ 4 ii. Routes to Opioid Misuse and Overdose Deaths: Pain Management, Illicit Drug Use, and Opioid Comorbidities in Black/African American Communities .................................................... 6 iii. Challenges to Prevention, Treatment, and Recovery .......................................................................... 7 Strategies to Address Opioid Misuse and OUD in Black/African American Communities ............ 9 i. Standard Treatment ................................................................................................................................ -

Phencyclidine: an Update
Phencyclidine: An Update U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse and Mental Health Administration Phencyclidine: An Update Editor: Doris H. Clouet, Ph.D. Division of Preclinical Research National Institute on Drug Abuse and New York State Division of Substance Abuse Services NIDA Research Monograph 64 1986 DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administratlon National Institute on Drug Abuse 5600 Fishers Lane Rockville, Maryland 20657 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National lnstitute on Drug Abuse and published by its Office of Science The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. SIDNEY COHEN, M.D. Temple University School of Medicine Los Angeles, California Philadelphia, Pennsylvania SYDNEY ARCHER, Ph.D. MARY L. JACOBSON Rensselaer Polytechnic lnstitute National Federation of Parents for Troy, New York Drug Free Youth RICHARD E. BELLEVILLE, Ph.D. Omaha, Nebraska NB Associates, Health Sciences Rockville, Maryland REESE T. JONES, M.D. KARST J. BESTEMAN Langley Porter Neuropsychiatric lnstitute Alcohol and Drug Problems Association San Francisco, California of North America Washington, D.C. DENISE KANDEL, Ph.D GILBERT J. BOTV N, Ph.D. College of Physicians and Surgeons of Cornell University Medical College Columbia University New York, New York New York, New York JOSEPH V. -

The Impact of Cannabis Access Laws on Opioid Prescribing
Journal of Health Economics 69 (2020) 102273 Contents lists available at ScienceDirect Journal of Health Economics j ournal homepage: www.elsevier.com/locate/econbase The impact of cannabis access laws on opioid prescribing a,∗ b c Benjamin J. McMichael , R. Lawrence Van Horn , W. Kip Viscusi a Assistant Professor of Law, University of Alabama School of Law, Box 870382, 101 Paul W. Bryant Drive East, Tuscaloosa, AL, 35487, United States b Associate Professor of Management and Law, Executive Director of Health Affairs, Owen Graduate School of Management, Vanderbilt University, 401 21st Avenue South, Nashville, TN, 37203, United States c University Distinguished Professor of Law, Economics, and Management, Vanderbilt University Law School. 131 21st Avenue South, Nashville, TN, 37203, United States a r a t i c l e i n f o b s t r a c t Article history: While recent research has shown that cannabis access laws can reduce the use of prescrip- Received 5 October 2018 tion opioids, the effect of these laws on opioid use is not well understood for all dimensions Received in revised form 17 July 2019 of use and for the general United States population. Analyzing a dataset of over 1.5 bil- Accepted 7 December 2019 lion individual opioid prescriptions between 2011 and 2018, which were aggregated to the Available online 14 December 2019 individual provider-year level, we find that recreational and medical cannabis access laws reduce the number of morphine milligram equivalents prescribed each year by 11.8 and 4.2 JEL classification: percent, respectively. These laws also reduce the total days’ supply of opioids prescribed, I180 the total number of patients receiving opioids, and the probability a provider prescribes K19 any opioids net of any offsetting effects. -

Opioid and Nicotine Use, Dependence, and Recovery: Influences of Sex and Gender
Opioid and Nicotine: Influences of Sex and Gender Conference Report: Opioid and Nicotine Use, Dependence, and Recovery: Influences of Sex and Gender Authors: Bridget M. Nugent, PhD. Staff Fellow, FDA OWH Emily Ayuso, MS. ORISE Fellow, FDA OWH Rebekah Zinn, PhD. Health Program Coordinator, FDA OWH Erin South, PharmD. Pharmacist, FDA OWH Cora Lee Wetherington, PhD. Women & Sex/Gender Differences Research Coordinator, NIH NIDA Sherry McKee, PhD. Professor, Psychiatry; Director, Yale Behavioral Pharmacology Laboratory Jill Becker, PhD. Biopsychology Area Chair, Patricia Y. Gurin Collegiate Professor of Psychology and Research Professor, Molecular and Behavioral Neuroscience Institute, University of Michigan Hendrée E. Jones, Professor, Department of Obstetrics and Gynecology; Executive Director, Horizons, University of North Carolina at Chapel Hill Marjorie Jenkins, MD, MEdHP, FACP. Director, Medical Initiatives and Scientific Engagement, FDA OWH Acknowledgements: We would like to acknowledge and extend our gratitude to the meeting’s speakers and panel moderators: Mitra Ahadpour, Kelly Barth, Jill Becker, Kathleen Brady, Tony Campbell, Marilyn Carroll, Janine Clayton, Wilson Compton, Terri Cornelison, Teresa Franklin, Maciej Goniewcz, Shelly Greenfield, Gioia Guerrieri, Scott Gottlieb, Marsha Henderson, RADM Denise Hinton, Marjorie Jenkins, Hendrée Jones, Brian King, George Koob, Christine Lee, Sherry McKee, Tamra Meyer, Jeffery Mogil, Ann Murphy, Christine Nguyen, Cheryl Oncken, Kenneth Perkins, Yvonne Prutzman, Mehmet Sofuoglu, Jack Stein, Michelle Tarver, Martin Teicher, Mishka Terplan, RADM Sylvia Trent-Adams, Rita Valentino, Brenna VanFrank, Nora Volkow, Cora Lee Wetherington, Scott Winiecki, Mitch Zeller. We would also like to thank those who helped us plan this program. Our Executive Steering Committee included Ami Bahde, Carolyn Dresler, Celia Winchell, Cora Lee Wetherington, Jessica Tytel, Marjorie Jenkins, Pamela Scott, Rita Valentino, Tamra Meyer, and Terri Cornelison. -

A Clinical Correlation Made Between Opioid-Induced Hyperalgesia and Hyperkatifeia with Brain Alterations Induced by Long-Term Prescription Opioid Use
Research & Reviews: A Journal of Neuroscience Volume 2, Issue 2, August 2012, Pages 1-11 __________________________________________________________________________________________ A Clinical Correlation Made Between Opioid-induced Hyperalgesia and Hyperkatifeia with Brain Alterations Induced by Long-term Prescription Opioid Use John K. Grandy (B.S., M.S., RPA-C )* North Country Urgent Care, Rte. 12f, Outer Coffeen street, Watertown NY 13601 ABSTRACT The goal of this article is to establish a correlation between the clinical manifestations of opioid-induced hyperalgesia and hyperkatifeia with the morphological and functional connectivity changes seen in the human brain that can be caused by long-term prescription opioid use. This will be accomplished by reviewing the imaging results found in a small but unique study that demonstrated morphological and functional connectivity changes in long-term prescription opioid users. The primary regions that were affected were the amygdala and the white matter tracts connected to it. Therefore, by reviewing the known functions of the amygdala and the white matter tracts - uncinate fasciculus, stria terminalis, and ventral amygdalofugal- and then doing a comparative analysis between the signs and symptoms of the clinical syndromes of opioid-induced hyperalgesia and hyperkatifeia a very obvious correlation has been recognized. Keywords: amygdala, POATS, opioid-induced neuron atrophy, intracellular messenger phosphokinase C, and NMDA receptors. *Author for Correspondence: E-mail [email protected] 1. INTRODUCTION physiological and behavioral functions [2], the majority of existing studies have been done on There has been an enormous increase in the heroin and methadone users. long-term use of prescription opioids over the past decade and a half. The use of opioids for The most frequently prescribed opioids are pain management can cause several hydrocodone [3] and oxycodone [4].