Woodlands Lodge Bulletin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thatcher, Northern Ireland and Anglo-Irish Relations, 1979-1990
From ‘as British as Finchley’ to ‘no selfish strategic interest’: Thatcher, Northern Ireland and Anglo-Irish Relations, 1979-1990 Fiona Diane McKelvey, BA (Hons), MRes Faculty of Arts, Humanities and Social Sciences of Ulster University A thesis submitted in partial fulfilment of the requirements of the Ulster University for the degree of Doctor of Philosophy August 2018 I confirm that the word count of this thesis is less than 100,000 words excluding the title page, contents, acknowledgements, summary or abstract, abbreviations, footnotes, diagrams, maps, illustrations, tables, appendices, and references or bibliography Contents Acknowledgements i Abstract ii Abbreviations iii List of Tables v Introduction An Unrequited Love Affair? Unionism and Conservatism, 1885-1979 1 Research Questions, Contribution to Knowledge, Research Methods, Methodology and Structure of Thesis 1 Playing the Orange Card: Westminster and the Home Rule Crises, 1885-1921 10 The Realm of ‘old unhappy far-off things and battles long ago’: Ulster Unionists at Westminster after 1921 18 ‘For God's sake bring me a large Scotch. What a bloody awful country’: 1950-1974 22 Thatcher on the Road to Number Ten, 1975-1979 26 Conclusion 28 Chapter 1 Jack Lynch, Charles J. Haughey and Margaret Thatcher, 1979-1981 31 'Rise and Follow Charlie': Haughey's Journey from the Backbenches to the Taoiseach's Office 34 The Atkins Talks 40 Haughey’s Search for the ‘glittering prize’ 45 The Haughey-Thatcher Meetings 49 Conclusion 65 Chapter 2 Crisis in Ireland: The Hunger Strikes, 1980-1981 -

Salisbury Playhouse Salisbury Arts Centre Spring/Summer 2019 Season
SALISBURY PLAYHOUSE SALISBURY ARTS CENTRE SPRING/SUMMER 2019 SEASON THEATRE | DANCE | MUSIC | COMEDY | FILM | EXHIBITIONS | WORKSHOPS | CAFÉS www.wiltshirecreative.co.uk Ticket Sales 01722 320333 1 CONTENTS WELCOME 3 SEE MORE, PAY LESS 4 – 5 FEST WEST 2019 6 SALISBURY INTERNATIONAL ARTS FESTIVAL 7 ONE NIGHT EVENTS AT SALISBURY PLAYHOUSE 8 – 10 SALISBURY PLAYHOUSE | MAIN HOUSE 11 – 22 SALISBURY PLAYHOUSE | THE SALBERG 23 – 33 SALISBURY ARTS CENTRE 34 LIVE MUSIC 35 – 39 THEATRE & DANCE 40 – 43 COMEDY 44 – 45 SILVER SCREEN WEDNESDAY MATINEES 46 FILM NIGHTS 47 LIVE SCREENINGS 48 – 49 VISUAL ARTS EXHIBITIONS 50 – 51 TAKE PART 52 – 53 WORKSHOPS 54 – 58 BECOME A MEMBER & PARTNER WITH US 59 PRICING 60 – 61 EVENT DIARY 62 – 65 2 WELCOME Welcome to the Spring 2019 Season at Salisbury Playhouse and Salisbury Arts Centre. At Salisbury Playhouse we are thrilled to be working with Wales Millennium Centre to produce the first stage production of Agatha Christie’s The Mirror Crack’d (premiering here prior to a national tour) and with York Theatre Royal on a new production of the razor-sharp comedy about The Queen and Mrs Thatcher, Handbagged. We are also delighted to be presenting Barney Norris’s new adaptation of The Remains of the Day, the welcome return of Around the World in 80 Days (prior to a U.S. tour) and Northern Broadsides’ production of Much Ado About Nothing. At Salisbury Arts Centre there’s a packed programme of music, theatre, film, visual art and more, including music from Nick Harper, Cara Dillon and Girls Only Jazz Orchestra, dance from Rosie Kay and Yorke Dance and comedy from Alfie Moore and Stuart Goldsmith. -

City Research Online
Keeble, R. (1996). The Gulf War myth: a study of the press coverage of the 1991 Gulf conflict. (Unpublished Doctoral thesis, City University London) City Research Online Original citation: Keeble, R. (1996). The Gulf War myth: a study of the press coverage of the 1991 Gulf conflict. (Unpublished Doctoral thesis, City University London) Permanent City Research Online URL: http://openaccess.city.ac.uk/7932/ Copyright & reuse City University London has developed City Research Online so that its users may access the research outputs of City University London's staff. Copyright © and Moral Rights for this paper are retained by the individual author(s) and/ or other copyright holders. All material in City Research Online is checked for eligibility for copyright before being made available in the live archive. URLs from City Research Online may be freely distributed and linked to from other web pages. Versions of research The version in City Research Online may differ from the final published version. Users are advised to check the Permanent City Research Online URL above for the status of the paper. Enquiries If you have any enquiries about any aspect of City Research Online, or if you wish to make contact with the author(s) of this paper, please email the team at [email protected]. The Gulf war myth A study of the press coverage of the 1991 Gulf conflict by Richard Keeble PhD in Journalism May 1996; Department of Journalism, City University, London CONTENTS Abstract ix Acknowledgements x Introduction xi-iii A.1 The war problematic xi -
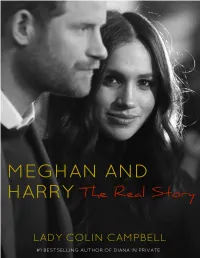
Meghan and Harry That They Would Have to Accept What Was on Offer and Not Demand What Was Not
Contents Title Page Chapter 1 Chapter 2 Chapter 3 Chapter 4 Chapter 5 Chapter 6 Chapter 7 Chapter 8 Chapter 9 Chapter 10 Chapter 11 Chapter 12 Photo Section Copyright CHAPTER 1 On May 19th 2018, when Meghan Markle stepped out of the antique Rolls Royce conveying her and her mother Doria Ragland from the former Astor stately home Cliveden to St. George’s Chapel, Windsor, where she was due to be married at 12 noon, she was a veritable vision of loveliness. At that moment, one of the biggest names of the age was born. As the actress ascended the steps of St. George’s Chapel, its interior and exterior gorgeously decorated in the most lavish and tasteful spring flowers, she was a picture of demure and fetching modesty, stylish elegance, transparent joyousness, and radiant beauty. The simplicity of her white silk wedding dress, designed by Clare Waight Keller of Givenchy, with its bateau neckline, three-quarter length sleeves, and stark, unadorned but stunningly simple bodice and skirt, coupled with the extravagant veil, five metres long and three metres wide, heavily embroidered with two of her favourite flowers (wintersweet and California poppy, as well as the fifty three native flowers of the various Commonwealth countries, and symbolic crops of wheat, and a piece of the blue dress that the bride had worn on her first date with the groom), gave out a powerful message. All bridal gowns make statements. Diana, Princess of Wales, according to her friend Carolyn Pride, used hers to announce to the world, ‘Here I am. -

YKC Spotlight on Art Dookie.Pdf
Spotlight on Art Dookie Dookie by Lucy Dawson Copyright: The Kennel Club Arts Foundation This lovely pastel is of the Welsh Corgi Dookie by Lucy Dawson. Dookie was very special as he was the first Corgi owned by King George VI, Her Majesty The Queen’s father. It was because of Dookie that the then Princess Elizabeth fell in love with the breed and has become one of the longest established breeders of Corgis. Dookie, whose Kennel Name was Rozavel Golden Eagle was bred by Thelma Gray in 1933 and as we know was the first in a long line of Royal Corgis. Dookie was chosen by His Majesty King George VI because he had a slightly longer tail than his litter mates. This appealed to the then Princess Elizabeth as she wanted him to have something to wag so that she would know if he was pleased or not. The artist is Lucy Dawson. She was particularly well known for her book illustrations and also produced a number of postcards under the pseudonym ‘Mac’. Many will recognise this as the name that appears on a lot of her work. She drew this portrait of Dookie at Royal Lodge, Windsor. Dookie by Lucy Dawson Your activity The artist has used pastels for this portrait as she did with most of her work. Have a closer look at it - what do you like about it? It’s a lovely memory of a first childhood pet. Perhaps you could draw a memory you have of when you first got your dog? Maybe it could be the first time they came home, or with the first toy you bought them? Have fun creating a lovely memory to keep!. -

Mackenzi Lee a História Do Mundo Em Cinquenta Cachorros
SUMÁRIO Capa Folha de rosto Sumário Dedicatória Prefácio Domesticação canina: Uma rápida introdução ao notório C.Ã.O. Fazendo a egípcia: Abuwtiyuw, o primeiro registro de nome de cão da história Ca-xoloitzcuintli: Ela é linda, absoluta, é Xoloitzcuintli Panhu pega geral: O ancestral original da mitologia chinesa Argos, o cão leal da Odisseia: O primeiro cachorro morto da literatura ocidental Todos os cães merecem o céu: Rei Yudhisthira e o cão do Mahabharata Peritas, o Grande: O cachorro um tanto mítico de Alexandre, o Grande Gosto muito de te ver, leãozinho chinês: O Pequinês e outros cães-leão da China O cão rei da Noruega não sabe o que faz: A história mítica de regentes ranzinzas São Roque, padroeiro dos cachorros: Senhor, fazei-me instrumento de vossos biscoitinhos Donnchadh, o fiel escudeiro de Roberto I: Caçador de recompensas por acidente Cãoquistadores! Cachorros forçados a serem cúmplices do colonialismo O Pug que sabia demais: Como um cachorro impediu um assassinato real Urian, o Galgo: Um cão mastiga a Igreja católica A guerra dos ossos: Os cachorros da Guerra Civil Inglesa A gravidade da situação: Quando o cachorro de Isaac Newton quase estragou tudo O xógum dos cães: Protegendo os vira-latas do Japão Quero conhaque! Barry e os cães de resgate do passo do Grande São Bernardo “Se quiser um amigo em Washington, adote um cachorro”: Primeiros-cães na Casa Branca O Pug Fortune: Napoleão Bonaparte é osso duro de roer Au au oeste! Lewis, Clark e o Terra-Nova Seaman lideram a descoberta Minha fama de mau-au: Boatswain, o cachorro -

My Shadow Is Pink All Bodies Are Good Bodies
LARRIKIN HOUSE My Shadow Is Pink Scott Stuart Summary My Shadow Is Pink is a beautifully written rhyming story that touches on the subjects of gender identity, self acceptance, equality and diversity. Inspired by the author’s own little boy, the main character likes princesses, fairies and things "not for boys." He soon learns (through the support of his dad) that everyone has a shadow that they sometimes feel they need to hide.This is an important book for a new generation of children (and adults alike) which exemplifies the concepts of unconditional love, respect and positive parenting. Larrikin House 9780648728757 Pub Date: 4/1/21 * An important and timely bookl Empowers LBGTQ children and the wider community with its strong and On Sale Date: 4/1/21 powerful message $16.99 USD Discount Code: LON * Encourages self love and acceptance Hardcover Picture Book * Teaches children the concept of diversity, equality and inclusion * Creates opportunity for open discussion and learning 32 Pages Carton Qty: 15 * Highlights current themes of gender identity Ages 5 to 7, Grades K to 2 * Bright and colorful illustrations by Scott Stuart Juvenile Fiction / Concepts JUV009120 Contributor Bio 10.8 in H | 10 in W | 0.3 in T Scott Stuart is father to a six-year-old boy who loves all things Queen Elsa and princesses. Having worked at | 1 lb Wt The Royal Children’s Hospital, he has seen how important it is for children to feel represented and is committed to creating stories of empowerment. All Bodies Are Good Bodies Charlotte Barkla, Erica Salcedo Summary Bold and beautiful, loud and proud, All Bodies are Good Bodies is an uplifting book about different body features and types. -

Public Spectacle and Ceremony in Britain, 1851-2012 Ryan G
Rollins College Rollins Scholarship Online Master of Liberal Studies Theses Fall 2014 Convocations of Empire: Public Spectacle and Ceremony in Britain, 1851-2012 Ryan G. Hudnall Rollins College - Master of Liberal Studies Program, [email protected] Follow this and additional works at: http://scholarship.rollins.edu/mls Part of the European History Commons Recommended Citation Hudnall, Ryan G., "Convocations of Empire: Public Spectacle and Ceremony in Britain, 1851-2012" (2014). Master of Liberal Studies Theses. 68. http://scholarship.rollins.edu/mls/68 This Open Access is brought to you for free and open access by Rollins Scholarship Online. It has been accepted for inclusion in Master of Liberal Studies Theses by an authorized administrator of Rollins Scholarship Online. For more information, please contact [email protected]. Rollins College Rollins Scholarship Online Masters of Liberal Studies Theses Fall 2014 Convocations of Empire: Public Spectacle and Ceremony in Britain, 1851-2012 Ryan G. Hudnall Follow this and additional works at: http://scholarship.rollins.edu/mls This Open Access is brought to you for free and open access by Rollins Scholarship Online. It has been accepted for inclusion in Masters of Liberal Studies Theses by an authorized administrator of Rollins Scholarship Online. For more information, please contact [email protected]. Convocations of Empire: Public Spectacle and Ceremony in Britain, 1851-2012 A Project Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Liberal Studies by Ryan G. Hudnall December, 2014 Mentor: Dr. R. Barry Levis Reader: Dr. Susan Libby Rollins College Hamilton Holt School Master of Liberal Studies Program Winter Park, Florida Convocations of Empire: Public Spectacle and Ceremony in Britain, 1851-2012 By Ryan G. -

St. Peter's Church, Boxted Flower Festival 11Th & 12Th June 2016
St. Peter’s Church, Boxted Flower Festival 11th & 12th June 2016 Guide to Exhibits The Porch 1. Clean for the Queen Stephen Whybrow, Coordinator of Boxted Litter Pickers ‘Clean for the Queen’ is a campaign launched by Country Life magazine in partnership with Keep Britain Tidy to clear up Britain in time for Her Majesty the Queen’s 90th birthday, which is officially celebrated this weekend. Boxted Litter Pickers comprise about 25 volunteers who have been keeping the roads and lanes of Boxted free from litter since 2008. More volunteers are always welcome. The South Aisle 2. The Royal Yacht Britannia Dot Garner The 83rd in a long line of royal yachts dating back to 1660 and Charles II, Her Majesty's Yacht Britannia was used as a base for 700 royal visits, entertaining and royal holidays, including Charles and Diana’s honeymoon. The Queen described Britannia as a place in which she could truly relax. Britannia is now moored in Edinburgh's port of Leith and is open to the public as a visitor attraction and hospitality venue. 3. 90th Birthday Cake Elaine Mott No birthday is complete without a cake! Buckingham Palace commissioned The Great British Bake Off Winner, Nadiya Hussain, to make the official birthday cake. Given free reign, she made a three‐tier orange drizzle cake with a butter cream and marmalade filling which she described as ‘the complete opposite of a traditional cake’. 4. The Queen’s Award for Voluntary Service Open Door Café The Queen’s Award for Voluntary Service is an annual award given to groups in the voluntary sector to recognise outstanding work done in their communities. -

Country Corgis, Dubois, Idaho
1 / 2 Country-corgis Idaho Country Corgis, Dubois, Idaho. 2,749 likes · 76 talking about this. We strive to raise happy,healthy puppies in a loving environment! Our corgis are part of .... It's simple… we love Pembroke Welsh Corgis. We love them so much we made it our mission to make them available to you. Our puppies are raised with love .... Cardigan Welsh Corgi/. Australian Shepherd mix. 1992-2008: Memorial. Forpaws Corgi and Corgi Mix rescue dogs. Cowboy's Country Corgi's / Shelbyville, TN .... I make awesome corgi dogs AND awesome country music. My family and I breed & sell AKC Pembroke Welsh Corgi puppies raised free of all toxins so you can .... ... Contribute Supplies · Other Ways to Give · Animal Protection & Control · Fort Collins · Loveland · Larimer County · Other Northern Colorado communities. Learn more about Rogue Country Corgis in Oregon. See puppy pictures, health information and reviews. Visit us now to find the right Pembroke Welsh Corgi for .... Has anyone ever gotten a corgi from “ unique country corgis” I'm thinking of buying one but I don't want to get scammed, just want to make sure they're legit. 0.. 295 Followers, 100 Following, 178 Posts - See Instagram photos and videos from Cowboy's Country Corgis (@cowboyscountrycorgis). Welcome to Country Road Corgis & Pomeranians ... Corgi History - Welsh folklore says the Corgi is the preferred mount of tiny, woodland fairy warriors (fairies .... A Look at the Inseparable Bond The Queen has Shared with Her Corgis Over the Past 50 Years. SUBSCRIBE ... country corgis country corgis, hill country corgis, connie's country corgis, rogue country corgis, unique country corgis, gator country corgis, tiger country corgis, idaho country corgis, big sky country corgis, cross country corgis AKC registered, corgi puppy- family raised-country raised, DM free, AKC registered, Well socialized. -

Ice Prestige Leicht | Extravagant | Stilvoll
ice prestige leicht | extravagant | stilvoll am besten auf eis, verfeinert mit frischer minze und himbeeren. Editorial Julien Backhaus Verleger und Bild: Ismail Gök Herausgeber Das nächste Heft erscheint am 27. Sept. 2018 Negatives Denken Das Interview mit dem Teufel Ich war wirklich neugierig, als mein Freund Georg von der Münch- den für negative Ereignisse, die uns alle eines Tages heimsuchen. ner Verlagsgruppe mir erzählte, dass sie bei FBV ein Buch von Wir sollten vorbereitet sein. Aber die Logik müsste uns raten, dass Napoleon Hill veröffentlichen werden, das a) bisher nie veröffent- wir uns auf das Positive konzentrieren. Es ist eine Sache, Notfall- licht wurde und b) ein Interview mit dem Teufel enthält. Ich wollte pläne in der Schublade zu haben, aber eine andere Sache, sich täg- uns sofort das Recht sichern, dieses Interview in Auszügen ver- lich auf das Negative zu fokussieren. Das grenzt an Dummheit. Das öffentlichen zu können. In diesem Interview lesen Sie, wie es der wirklich Entscheidende dabei ist, dass wir ein Bewusstsein schaffen. Teufel schafft, uns zu beherrschen. Und zwar täglich. Man sagt, der Wir dürfen nicht passiv durch die Weltgeschichte laufen und gar Teufel steckt im Detail. Und seine Antworten im Interview beweisen nicht merken, was in uns vorgeht. Wir müssen stets in der Lage sein, das. Denn in dem er sich in unsere Gedankenwelt einschleicht und uns und unsere Gedanken aus der Vogelperspektive zu betrachten. uns kleine negative Gedanken einpflanzt, gewinnt er durch unsere Dann haben wir die Kontrolle und können aktiv eingreifen. Es hat Angst vor Armut oder Kritik die Kontrolle über uns. -
Lake City Reporter
1A SUNDAY, JULY 29, 2012 | YOUR COMMUNITY NEWSPAPER SINCE 1874 | $1.00 Lake City Reporter LAKECITYREPORTER.COM First Federal Volunteering SUNDAY EDITION marks 50th helps local anniversary. 1C teen cope. 1D Jarvis target TONY BRITT/Lake City Reporter LCPD Chief Argatha Gilmore, right, with Lt. Clint VanBennekom at the scene of a fatal shooting Friday night in Lake City. of grand jury go before a grand Circuit state attorney was appointed to 3rd Circuit State Attorney jury. the case by Gov. RIck Scott. Shooting is subject of complaint by Former Assistant A grand jury is scheduled Aug. 20 in State Attorney Tallahassee, said David Collins, Jarvis’s a former assistant. Michael J. San attorney. Filippo filed the com- Jarvis was elected in 2008 as state leaves one By LAURA HAMPSON plaint against Jarvis. attorney for the Third Judicial Circuit, [email protected] Following the Jarvis which covers Columbia, Dixie, Hamilton, complaint, a Florida Lafayette, Madison, Suwannee and Following a complaint and an inves- Department of Law Enforcement inves- Taylor counties. dead, two tigation, Third Judicial Circuit State tigation found enough information to Attorney Robert L. “Skip” Jarvis Jr. will move forward. Brad King, Fifth Judicial JARVIS continued on 3A in custody Recycling in Debby’s wake By LAURA HAMPSON [email protected] A Lake City man was fatally shot Friday during an argument and the two suspects hijacked a car before leading police on a chase, according to reports. After the pursuit, police say they found more than $20,000 worth of cocaine on the suspects. Carlos Lamar Williams, 31, was shot multiple times Williams at Wayne Drive Apartments, where he lived, and was pro- nounced dead at Lake City Medical Center, according to a release from Steve Shaw, public information officer for the Lake City Police Department.