Moftah Hussin Alhagamhmad
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sanjay Kumar Gupta
The human CCHC-type Zinc Finger Nucleic Acid Binding Protein (CNBP) binds to the G-rich elements in target mRNA coding sequences and promotes translation Das humane CCHC-Typ-Zinkfinger-Nukleinsäure-Binde-Protein (CNBP) bindet an G-reiche Elemente in der kodierenden Sequenz seiner Ziel-mRNAs und fördert deren Translation Doctoral thesis for a doctoral degree at the Graduate School of Life Sciences, Julius-Maximilians-Universität WürzBurg, Section: Biomedicine suBmitted By Sanjay Kumar Gupta from Varanasi, India WürzBurg, 2016 1 Submitted on: …………………………………………………………..…….. Office stamp Members of the Promotionskomitee: Chairperson: Prof. Dr. Alexander Buchberger Primary Supervisor: Dr. Stefan Juranek Supervisor (Second): Prof. Dr. Utz Fischer Supervisor (Third): Dr. Markus Landthaler Date of Public Defence: …………………………………………….………… Date of Receipt of Certificates: ………………………………………………. 2 Summary The genetic information encoded with in the genes are transcribed and translated to give rise to the functional proteins, which are building block of a cell. At first, it was thought that the regulation of gene expression particularly occurs at the level of transcription By various transcription factors. Recent discoveries have shown the vital role of gene regulation at the level of RNA also known as post-transcriptional gene regulation (PTGR). Apart from non-coding RNAs e.g. micro RNAs, various RNA Binding proteins (RBPs) play essential role in PTGR. RBPs have been implicated in different stages of mRNA life cycle ranging from splicing, processing, transport, localization and decay. In last 20 years studies have shown the presence of hundreds of RBPs across eukaryotic systems many of which are widely conserved. Given the rising numBer of RBPs and their link to human diseases it is quite evident that RBPs have major role in cellular processes and their regulation. -
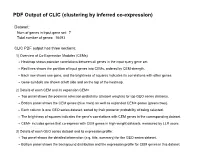
PDF Output of CLIC (Clustering by Inferred Co-Expression)
PDF Output of CLIC (clustering by inferred co-expression) Dataset: Num of genes in input gene set: 7 Total number of genes: 16493 CLIC PDF output has three sections: 1) Overview of Co-Expression Modules (CEMs) Heatmap shows pairwise correlations between all genes in the input query gene set. Red lines shows the partition of input genes into CEMs, ordered by CEM strength. Each row shows one gene, and the brightness of squares indicates its correlations with other genes. Gene symbols are shown at left side and on the top of the heatmap. 2) Details of each CEM and its expansion CEM+ Top panel shows the posterior selection probability (dataset weights) for top GEO series datasets. Bottom panel shows the CEM genes (blue rows) as well as expanded CEM+ genes (green rows). Each column is one GEO series dataset, sorted by their posterior probability of being selected. The brightness of squares indicates the gene's correlations with CEM genes in the corresponding dataset. CEM+ includes genes that co-express with CEM genes in high-weight datasets, measured by LLR score. 3) Details of each GEO series dataset and its expression profile: Top panel shows the detailed information (e.g. title, summary) for the GEO series dataset. Bottom panel shows the background distribution and the expression profile for CEM genes in this dataset. Overview of Co-Expression Modules (CEMs) with Dataset Weighting Scale of average Pearson correlations Num of Genes in Query Geneset: 7. Num of CEMs: 1. 0.0 0.2 0.4 0.6 0.8 1.0 Ctr9 Rtf1 Paf1 Cdc73 Leo1 Wdr61 Pex2 Ctr9 Rtf1 -

Protein Identities in Evs Isolated from U87-MG GBM Cells As Determined by NG LC-MS/MS
Protein identities in EVs isolated from U87-MG GBM cells as determined by NG LC-MS/MS. No. Accession Description Σ Coverage Σ# Proteins Σ# Unique Peptides Σ# Peptides Σ# PSMs # AAs MW [kDa] calc. pI 1 A8MS94 Putative golgin subfamily A member 2-like protein 5 OS=Homo sapiens PE=5 SV=2 - [GG2L5_HUMAN] 100 1 1 7 88 110 12,03704523 5,681152344 2 P60660 Myosin light polypeptide 6 OS=Homo sapiens GN=MYL6 PE=1 SV=2 - [MYL6_HUMAN] 100 3 5 17 173 151 16,91913397 4,652832031 3 Q6ZYL4 General transcription factor IIH subunit 5 OS=Homo sapiens GN=GTF2H5 PE=1 SV=1 - [TF2H5_HUMAN] 98,59 1 1 4 13 71 8,048185945 4,652832031 4 P60709 Actin, cytoplasmic 1 OS=Homo sapiens GN=ACTB PE=1 SV=1 - [ACTB_HUMAN] 97,6 5 5 35 917 375 41,70973209 5,478027344 5 P13489 Ribonuclease inhibitor OS=Homo sapiens GN=RNH1 PE=1 SV=2 - [RINI_HUMAN] 96,75 1 12 37 173 461 49,94108966 4,817871094 6 P09382 Galectin-1 OS=Homo sapiens GN=LGALS1 PE=1 SV=2 - [LEG1_HUMAN] 96,3 1 7 14 283 135 14,70620005 5,503417969 7 P60174 Triosephosphate isomerase OS=Homo sapiens GN=TPI1 PE=1 SV=3 - [TPIS_HUMAN] 95,1 3 16 25 375 286 30,77169764 5,922363281 8 P04406 Glyceraldehyde-3-phosphate dehydrogenase OS=Homo sapiens GN=GAPDH PE=1 SV=3 - [G3P_HUMAN] 94,63 2 13 31 509 335 36,03039959 8,455566406 9 Q15185 Prostaglandin E synthase 3 OS=Homo sapiens GN=PTGES3 PE=1 SV=1 - [TEBP_HUMAN] 93,13 1 5 12 74 160 18,68541938 4,538574219 10 P09417 Dihydropteridine reductase OS=Homo sapiens GN=QDPR PE=1 SV=2 - [DHPR_HUMAN] 93,03 1 1 17 69 244 25,77302971 7,371582031 11 P01911 HLA class II histocompatibility antigen, -

An Overview of Crohn's Disease: an Explanation and Analysis of the Event Planning Process Claire Wilcox Grand Valley State University
Grand Valley State University ScholarWorks@GVSU Honors Projects Undergraduate Research and Creative Practice 4-25-2014 Chronically Ill but Chronically Fabulous: An Overview of Crohn's Disease: An Explanation and Analysis of the Event Planning Process Claire Wilcox Grand Valley State University Follow this and additional works at: http://scholarworks.gvsu.edu/honorsprojects Recommended Citation Wilcox, Claire, "Chronically Ill but Chronically Fabulous: An Overview of Crohn's Disease: An Explanation and Analysis of the Event Planning Process" (2014). Honors Projects. 318. http://scholarworks.gvsu.edu/honorsprojects/318 This Open Access is brought to you for free and open access by the Undergraduate Research and Creative Practice at ScholarWorks@GVSU. It has been accepted for inclusion in Honors Projects by an authorized administrator of ScholarWorks@GVSU. For more information, please contact [email protected]. Chronically Ill but Chronically Fabulous 1 Chronically Ill but Chronically Fabulous: An Overview of Crohn's Disease An Explanation and Analysis of the Event Planning Process Claire Wilcox Grand Valley State University HNR 499 Dr. J. Chamberlain Prof. Nelson Van Elderen April 25, 2014 Chronically Ill but Chronically Fabulous 2 Dedications I would like to thank, first and foremost, my Holy Father in Heaven. Without His constant guidance, provision, and healing I would not be where I am. It is through his power that I have been able to study abroad and succeed academically and socially in college. He walked with me through my physical and mental pain, lifted me up when it seemed impossible to go on, caught my tears in his cradled hands, and cheered me on through it all – simply fighting for his beloved child. -

An Empirical Model of Information System to Improve Performance Ability in Patients with Crohn’S Disease
International Journal of Control and Automation Vol.7, No.9 (2014), pp.305-316 http://dx.doi.org/10.14257/ijca.2014.7.9.27 An Empirical Model of Information System to Improve Performance Ability in Patients with Crohn’s Disease Seong-Ran Lee Department of Medical Information, Kongju National University [email protected] Abstract This paper is to develop an empirical model of information system to improve performance ability in patients with Crohn’s disease. The pairwise t-test was done to compare the before and after intervention effect of performance ability in patients with Crohn’s disease. The results of this findings are as follows. Firstly, comparing the mean scores in the stress status, respondents’ score(52.07±0.82) after intervention a statistically significantly decreased than respondents(76.25±1.49) before intervention(t=1.94, p=.026). Secondly, this paper found that the performance ability in patients with Crohn’s disease was increased by 68.92- 82.95% compared with the previous status. Therefore, this paper will provide framework of a system development for managing the patients with Crohn’s disease according to information system . Keywords: Empirical model, Information system, Performance ability, Crohn’s disease 1. Introduction Crohn’s disease is a type of inflammatory bowel disease that may affect any part of the gastrointestinal tract from mouth to anus. Symptoms often include: abdominal pain, diarrhea (which may be bloody if inflammation is severe), fever and weight loss, Other complications may occur outside the gastrointestinal tract and include: anemia, skin rashes, arthritis, inflammation of the eye, and tiredness. -

Genome-Wide Determination of On-Target and Off-Target Characteristics for RNA-Guided DNA Methylation by Dcas9 Methyltransferases.” Gigascience 7 (3): Giy011
Genome-wide determination of on- target and off-target characteristics for RNA-guided DNA methylation by dCas9 methyltransferases The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Lin, L., Y. Liu, F. Xu, J. Huang, T. F. Daugaard, T. S. Petersen, B. Hansen, et al. 2018. “Genome-wide determination of on-target and off-target characteristics for RNA-guided DNA methylation by dCas9 methyltransferases.” GigaScience 7 (3): giy011. doi:10.1093/ gigascience/giy011. http://dx.doi.org/10.1093/gigascience/giy011. Published Version doi:10.1093/gigascience/giy011 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:37068160 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA GigaScience, 7, 2018, 1–19 doi: 10.1093/gigascience/giy011 Advance Access Publication Date: 19 February 2018 Research RESEARCH Genome-wide determination of on-target and off-target characteristics for RNA-guided DNA methylation by dCas9 methyltransferases Lin Lin1,2,†,YongLiu1,†, Fengping Xu3,4,5,†,JinrongHuang3,4,5,†, Tina Fuglsang Daugaard1, Trine Skov Petersen1, Bettina Hansen1, Lingfei Ye3,QingZhou3,4, Fang Fang3,4,LingYang3,4, Shengting Li1,3, Lasse Fløe1, Kristopher Torp Jensen1, Ellen Shrock6, Fang Chen3,4,5, Huanming Yang3,4,7,JianWang3,4,XinLiu3,4,XunXu3,4,∗, Lars Bolund1,3,4,2,8,9, Anders Lade Nielsen1 and Yonglun Luo1,3,4,2,8,9,10,∗ 1Department of Biomedicine, Aarhus University, Aarhus, Denmark, 2Danish Regenerative Engineering Alliance for Medicine, Department of Biomedicine, Aarhus University, Aarhus, Denmark, 3BGI-Shenzhen, Shenzhen 518083, China, 4China National GeneBank-Shenzhen, BGI-Research, Shenzhen 518083, China, 5Department of Biology, University of Copenhagen, Copenhagen, Denmark, 6Department of Genetics, Harvard Medical School, Boston, MA, USA, 7James D. -

Supplementary File 1
Supplementary Materials Figure S1. RNA sequencing quality control report. The upper panel showed per base sequence quality of (a) miRNA from 786-O and ACHN, and (b) RNA from 786-O and ACHN; the lower panel showed the per sequence quality scores of (c) miRNA from 786-O and ACHN, and (d) RNA from 786-O and ACHN. The quality score from 15 to 99 bp fell into the green background, indicating good quality calls. The majority read > 35 indicated good sequencing quality. Table S1. The list of miRNA with significant changes (ACHN vs 786-O) #miRNA Fold Change #miRNA Fold Change #miRNA Fold Change hsa-let-7a-2-3p -490.00 hsa-miR-192-5p 21.37 hsa-miR-323a-3p 135.76 hsa-let-7c-3p -10.30 hsa-miR-194-3p 31.18 hsa-miR-323b-3p 53.75 hsa-miR-100-3p -26.39 hsa-miR-194-5p 21.87 hsa-miR-326 -16.46 hsa-miR-100-5p -63.93 hsa-miR-195-5p 8.31 hsa-miR-329-3p 101.81 hsa-miR-105-5p -288.00 hsa-miR-196a-3p 5.28 hsa-miR-329-5p 436 hsa-miR-1185-1-3p 32.08 hsa-miR-199b-5p -9.75 hsa-miR-335-3p 73.67 hsa-miR-1185-2-3p 37.22 hsa-miR-203a-3p 222.25 hsa-miR-335-5p 71.58 hsa-miR-1185-5p 91.13 hsa-miR-205-5p -5.12 hsa-miR-337-3p 1696 hsa-miR-1197 7.38 hsa-miR-20b-5p 5.28 hsa-miR-337-5p 12141 hsa-miR-125b-1-3p -301.58 hsa-miR-211-5p 118 hsa-miR-34b-3p 1110.62 hsa-miR-125b-2-3p 5.91 hsa-miR-215-5p 18.88 hsa-miR-34b-5p 796.38 hsa-miR-1262 16.28 hsa-miR-218-5p 14.37 hsa-miR-34c-3p 10751 hsa-miR-1266-5p 6.62 hsa-miR-224-5p 118 hsa-miR-34c-5p 836.81 hsa-miR-127-3p 1723.39 hsa-miR-2277-3p 6.65 hsa-miR-3614-5p 141 hsa-miR-127-5p 4334.00 hsa-miR-2682-3p 6.63 hsa-miR-3617-5p -140 hsa-miR-1271-5p -

Novel Gene Discovery in Primary Ciliary Dyskinesia
Novel Gene Discovery in Primary Ciliary Dyskinesia Mahmoud Raafat Fassad Genetics and Genomic Medicine Programme Great Ormond Street Institute of Child Health University College London A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy University College London 1 Declaration I, Mahmoud Raafat Fassad, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. 2 Abstract Primary Ciliary Dyskinesia (PCD) is one of the ‘ciliopathies’, genetic disorders affecting either cilia structure or function. PCD is a rare recessive disease caused by defective motile cilia. Affected individuals manifest with neonatal respiratory distress, chronic wet cough, upper respiratory tract problems, progressive lung disease resulting in bronchiectasis, laterality problems including heart defects and adult infertility. Early diagnosis and management are essential for better respiratory disease prognosis. PCD is a highly genetically heterogeneous disorder with causal mutations identified in 36 genes that account for the disease in about 70% of PCD cases, suggesting that additional genes remain to be discovered. Targeted next generation sequencing was used for genetic screening of a cohort of patients with confirmed or suggestive PCD diagnosis. The use of multi-gene panel sequencing yielded a high diagnostic output (> 70%) with mutations identified in known PCD genes. Over half of these mutations were novel alleles, expanding the mutation spectrum in PCD genes. The inclusion of patients from various ethnic backgrounds revealed a striking impact of ethnicity on the composition of disease alleles uncovering a significant genetic stratification of PCD in different populations. -

Redalyc.Crohn Disease
Autopsy and Case Reports E-ISSN: 2236-1960 [email protected] Hospital Universitário da Universidade de São Paulo Brasil Geller, Stephen A.; de Campos, Fernando P. F. Crohn disease Autopsy and Case Reports, vol. 5, núm. 2, abril-junio, 2015, pp. 5-8 Hospital Universitário da Universidade de São Paulo São Paulo, Brasil Available in: http://www.redalyc.org/articulo.oa?id=576060829002 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Image in focus Imagem em foco Crohn disease Stephen A Gellerab, Fernando P F de Camposc Geller SA, Campos FPF. Crohn disease. Autopsy Case Rep [Internet]. 2015; 5(2):5-8. http://dx.doi.org/10.4322/acr.2015.001 Dr. Stephen A Geller personal archive Aretaeus of Cappadocia (1st century CE) described patient dying after a prolonged dysentery-like course. a young man with chronic and recurring abdominal Louis XIII, King of France (1601-1643) died at the age distress possibly representing the first recorded instance of 42 after decades of abdominal pain, fever, bloody of Crohn disease (CD).1-3 More evidence that this disease diarrhea and rectal/perianal abscesses.4 However, it was was extant for many years comes from the description in 1761 that Giovanni Battista Morgagni (1682-1771), of the 10th century English king, Alfred “the great,” a towering figure in the history of medicine, described who suffered for many years from what was a typical a 20-year-old man with typical regional ileitis, who enteritis but also had anal fistula and/or abscess.4 In died. -

RNA Splicing in the Transition from B Cells
RNA Splicing in the Transition from B Cells to Antibody-Secreting Cells: The Influences of ELL2, Small Nuclear RNA, and Endoplasmic Reticulum Stress This information is current as of September 24, 2021. Ashley M. Nelson, Nolan T. Carew, Sage M. Smith and Christine Milcarek J Immunol 2018; 201:3073-3083; Prepublished online 8 October 2018; doi: 10.4049/jimmunol.1800557 Downloaded from http://www.jimmunol.org/content/201/10/3073 Supplementary http://www.jimmunol.org/content/suppl/2018/10/05/jimmunol.180055 http://www.jimmunol.org/ Material 7.DCSupplemental References This article cites 44 articles, 16 of which you can access for free at: http://www.jimmunol.org/content/201/10/3073.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 24, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2018 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology RNA Splicing in the Transition from B Cells to Antibody-Secreting Cells: The Influences of ELL2, Small Nuclear RNA, and Endoplasmic Reticulum Stress Ashley M. -

Umb 3 Lat Umb2'2006 Corectat3.Qxd
Archives of the Balkan Medical Union vol. 50, no. 3, pp. 399-405 Copyright © 2015 CELSIUS September 2015 REVIEW THE GENESIS OF INFLAMMATORY BOWEL DISEASE YESTERDAY, TODAY, TOMORROW DORINA CALAGIU1, MIRCEA DICULESCU1,2, ROXANA MARIA NEMEÆ3, CORINA SILVIA POP1,4 1„Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania 2Gastroenterology and Hepatology Center, Fundeni Clincal Insitute, Bucharest, Romania 3”Marius Nasta” Institute National of Pneumology, Bucharest, Romania 4Emergency University Hospital, Bucharest, Romania SUMMARY RÉSUMÉ The discovery of Inflammatory Bowel Disease (IBD) has had a La genèse de la maladie inflammatoire de l’intestin hier, à tumultuous trajectory, beginning with its recognition as a medical présent, demain entity to defining and understanding. The genesis of the two diseases included in the spectrum of IBD is the same with the La découverte de la maladie inflammatoire de l'intestin (MII) a eu one of humanity, the earliest descriptions belonging to ancient une trajectoire tumultueuse, en commençant par sa reconnais- Greeks, but the differentiation between them and other intestinal sance comme une entité médicale à la définition et la pathologies took place years later. Even establishing the names of compréhension. La genèse de ces deux maladies incluses dans le Ulcerative colitis (UC) and Crohn’s disease (CD) encountered spectre de l'IBD est la même avec celle de l'humanité, les difficulties. With the beginning of the modern era, remarkable premières descriptions appartenant aux Grecs anciens, mais la progress has been made in the field of medicine - both in under- différenciation entre eux et d'autres pathologies intestinales a eu standing the diseases and in treating it. -

Combinatorial Strategies Using CRISPR/Cas9 for Gene Mutagenesis in Adult Mice
Combinatorial strategies using CRISPR/Cas9 for gene mutagenesis in adult mice Avery C. Hunker A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2019 Reading Committee: Larry S. Zweifel, Chair Sheri J. Mizumori G. Stanley McKnight Program Authorized to Offer Degree: Pharmacology 2 © Copyright 2019 Avery C. Hunker 3 University of Washington ABSTRACT Combinatorial strategies using CRISPR/Cas9 for gene mutagenesis in adult mice Avery C. Hunker Chair of the Supervisory Committee: Larry Zweifel Department of Pharmacology A major challenge to understanding how genes modulate complex behaviors is the inability to restrict genetic manipulations to defined cell populations or circuits. To circumvent this, we created a simple strategy for limiting gene knockout to specific cell populations using a viral-mediated, conditional CRISPR/SaCas9 system in combination with intersectional genetic strategies. A small single guide RNA (sgRNA) directs Staphylococcus aureus CRISPR-associated protein (SaCas9) to unique sites on DNA in a Cre-dependent manner resulting in double strand breaks and gene mutagenesis in vivo. To validate this technique we targeted nine different genes of diverse function in distinct cell types in mice and performed an array of analyses to confirm gene mutagenesis and subsequent protein loss, including IHC, cell-type specific DNA sequencing, electrophysiology, Western blots, and behavior. We show that these vectors are as efficient as conventional conditional gene knockout and provide a viable alternative to complex genetic crosses. This strategy provides additional benefits of 4 targeting gene mutagenesis to cell types previously difficult to isolate, and the ability to target genes in specific neural projections for gene inactivation.