LIBRO DEGLI ABSTRACTS Congress Proceedings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

24–25 March 2021
VIRTUAL EVENT ROME INTER-MEETING Rome Interventional Radiotherapy Meeting 24–25 March 2021 Registration and information: www.gemelliart.it/interacts Endorsed by La Multiprofessionalità in Radioterapia Interventistica (Brachiterapia) (sessione in Italiano) 24 March 17:00 Apertura dei lavori Luca Tagliaferri (Roma) Introduzione: Maria Antonietta Gambacorta (Roma), Stefano Durante (Bologna) Maurizio Zega (Roma) 17:20 Formazione multiprofessionale: la radioterapia interventistica per le neoplasie prostatiche Moderatori: Giancarlo Mattiucci (Roma) 17:20 Lettura: La tecnica HDR (informazioni pratiche procedurali) Luca Tagliaferri (Roma) 17:50 Lettura: La tecnica LDR (informazioni pratiche procedurali) Andrea Vavassori (Milano) 18:20 Discussant: Sara Scalise (Roma), Carmela Galdieri (Milano) 18:30 Aspetti relazionali in RT interventistica Moderatori: Daniela Chieffo (Roma) 18:30 Lettura: Progetto HAPPY—Humanity Assurance Protocol in interventional radiotheraPY Patrizia Cornacchione (Roma) 18:40 Lettura: Progetto SPIRIT (Supporto Psicologico In Radioterapia InTerventistica: approccio EMDR) Loredana Dinapoli (Roma) 18:50 Discussant: Lisa Vicenzi (Ancona), Gianni Penduzzu (Torino) 19:00 Ricerca ed evidenze, la multiprofessionalità che funziona Moderatori: Cristiana Vidali (Trieste) 19:00 Lettura: Le nuove competenze del TSRM nella ricerca Moreno Zanardo (Milano) 19:10 Lettura: Il ruolo dell’infermiere nella ricerca Antonello Cocchieri (Roma) 19:20 Discussant: Patrizia Cornacchione (Roma), Elena Cristofori (Roma) 19:30 Discussione Moderatori: Vitaliana -

INTERNAZIONALI DI TENNIS D'abruzzo ORDER of PLAY - Wednesday, 24 April 2019
INTERNAZIONALI DI TENNIS D'ABRUZZO ORDER OF PLAY - Wednesday, 24 April 2019 CENTER COURT GRANDSTAND COURT 1 Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 10:00 am [WC] Giulio ZEPPIERI (ITA) Oscar OTTE (GER) [3] Jurij RODIONOV (AUT) [13] 1 vs vs vs Dominik KOEPFER (GER) [11] Bernabe ZAPATA MIRALLES (ESP) Jose HERNANDEZ-FERNANDEZ (DOM) followed by followed by Not Before 11:00 am TBF 6/4 6/7(4) 4/4 [WC] Alessio DE BERNARDIS (ITA) Maximilian MARTERER (GER) [1] [ITF] Riccardo BONADIO (ITA) Giuseppe TRESCA (ITA) 2 vs vs vs Gastao ELIAS (POR) Kimmer COPPEJANS (BEL) [10] Tomislav BRKIC (BIH) Nikola CACIC (SRB) followed by followed by followed by after suitable rest Kimmer COPPEJANS (BEL) Thomaz BELLUCCI (BRA) Alexey VATUTIN (RUS) Sander GILLE (BEL) 3 vs vs vs Facundo ARGUELLO (ARG) [16] Viktor GALOVIC (CRO) [14] Enzo COUACAUD (FRA) Rudolf MOLLEKER (GER) followed by followed by followed by Denys MOLCHANOV (UKR) Philipp OSWALD (AUT) Stefano TRAVAGLIA (ITA) [5] Igor ZELENAY (SVK) [1] Filip POLASEK (SVK) [3] 4 vs vs vs Andrea PELLEGRINO (ITA) ALTERNATE [ITF] Riccardo BONADIO (ITA) David PEREZ SANZ (ESP) Not Before 5:00 pm followed by [ITF] Javier BARRANCO COSANO (ESP) Federico GAIO (ITA) Raul BRANCACCIO (ITA) 5 vs vs Salvatore CARUSO (ITA) [4] [WC] Lorenzo MUSETTI (ITA) Giulio ZEPPIERI (ITA) followed by Julian OCLEPPO (ITA) Andrea VAVASSORI (ITA) 6 vs Jonathan EYSSERIC (FRA) Andrei VASILEVSKI (BLR) [4] Luca del Federico 23 April 2019 at 20:27 Carmelo Di dio Tournament Director Order of Play released Challenger Supervisor ANY MATCH ON ANY COURT MAY BE MOVED MATCHES WILL BE CALLED FROM THE Romano Grillotti PLAYERS' LOUNGE & LOCKER-ROOM Referee Singles Lucky-Loser Sign-in Deadline : 9.30 am Doubles Alternate Sign-in Deadline : 10.30 am Singles Alternate Sign-in Deadline : 9.30 am. -

Italian Books
Italian Books I Philobiblon Rome London New York In collaboration with Govi Rare Books, New York Italian Books I Spring 2019 Preface We are very pleased to present Philobiblon’s new publishing initiative Italian Books, a series of numbered catalogues devoted to the important place of Italian culture on the world stage. The catalogues will feature manuscripts, documents, printed books, engravings, drawings, and artist’s books produced in Italy, as well as Italian books printed outside the country, translations attesting to the impact of Italian culture abroad, including volumes finely bound by sought-after Italian binders, and those once owned by great protagonists of Italian book collecting. Together these selections will illuminate a journey into the multifarious Italian book world in the broadest and richest sense. After all, the history of the book itself is a fascinating narrative, an uninterrupted medley of fruitful cultural transfers and the migration of ideas. In this regard, Italy has always represented a unique crossroad among cultures, the custodian of ancient past, as well as the gateway between Western and Eastern worlds, whose academies, art collections, libraries, printing houses, and bookshops have provided, over the centuries, fertile meeting grounds for generations of scholars, bibliophiles, and connoisseurs. In the first decades of the twentieth century, two international exhibitions paid homage to the Italian book. The Mostra Storica dell’Arte della Stampa in Italia opened in Leipzig in 1914 and presented the magnificence of Italian book production from the fifteenth to the eighteenth century. The splendid Exposition du Livre Italien followed in Paris in 1926, mounted at the Bibliothèque Nationale and the Musée des Arts Décoratifs. -

EMILIA-ROMAGNA OPEN ORDER of PLAY - Tuesday, 25 May 2021
EMILIA-ROMAGNA OPEN ORDER OF PLAY - Tuesday, 25 May 2021 CENTER COURT GRAND STAND COURT 1 COURT 5 Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 10:00 am Matt REID (AUS) [WC] Marco CECCHINATO (ITA) Sam QUERREY (USA) Emil RUUSUVUORI (FIN) Michael VENUS (NZL) 1 vs vs vs vs [Q] Raul BRANCACCIO (ITA) Yoshihito NISHIOKA (JPN) [8] [LL] Norbert GOMBOS (SVK) Nathaniel LAMMONS (USA) Jackson WITHROW (USA) followed by followed by followed by followed by Oliver MARACH (AUT) [WC] Andreas SEPPI (ITA) Aljaz BEDENE (SLO) [7] Steve JOHNSON (USA) Aisam-Ul-Haq QURESHI (PAK) 2 vs vs vs vs Sebastian KORDA (USA) Salvatore CARUSO (ITA) Jiri VESELY (CZE) Raven KLAASEN (RSA) Ben MCLACHLAN (JPN) [2] followed by followed by followed by followed by [WC] David MARRERO (ESP) Gianluca MAGER (ITA) Gilles SIMON (FRA) Jaume MUNAR (ESP) David VEGA HERNANDEZ (ESP) 3 vs vs vs vs Lorenzo MUSETTI (ITA) [Q] Pedro MARTINEZ (ESP) [Q] Mikael YMER (SWE) Roman JEBAVY (CZE) Aleksandr NEDOVYESOV (KAZ) followed by followed by followed by followed by after suitable rest Max PURCELL (AUS) Marcus DANIELL (NZL) Andrey GOLUBEV (KAZ) Richard GASQUET (FRA) [5] Luke SAVILLE (AUS) Philipp OSWALD (AUT) [3] Andrea VAVASSORI (ITA) 4 vs vs vs vs [Q] Daniel ALTMAIER (GER) Marco CECCHINATO (ITA) Simone BOLELLI (ITA) Marcelo AREVALO (ESA) Andreas SEPPI (ITA) Maximo GONZALEZ (ARG) Matwe MIDDELKOOP (NED) [4] followed by Sander GILLE (BEL) Joran VLIEGEN (BEL) [1] 5 vs [WC] Francesco PASSARO (ITA) Stefano TRAVAGLIA (ITA) Sergio Palmieri Thomas Schrader Romano Grillotti Carlos Sanches/Carmelo Di Dio Tournament Director Tour Manager Referee ATP Supervisor Order of Play released : 24 May 2021 at 15:58 Singles Lucky-Loser Sign-in Deadline : 9.30 AM MATCHES WILL BE CALLED ANY MATCH ON ANY COURT Doubles Alternate Sign In Deadline : 9.30 AM FROM THE PLAYERS' LOUNGE & MAY BE MOVED LOCKER-ROOM. -

Radioterapia Personalizzata: Un Nuovo Paradigma in Oncologia
XXX CONGRESSO NAZIONALE AIRO XXXII CONGRESSO NAZIONALE AIRB XI CONGRESSO NAZIONALE AIRO GIOVANI 2020 Virtual 9-12 Dicembre Radioterapia personalizzata: un nuovo paradigma in oncologia Associazione Italiana Radioterapia e Oncologia clinica XXX CONGRESSO NAZIONALE AIRO XXXII CONGRESSO NAZIONALE AIRB XI CONGRESSO NAZIONALE AIRO GIOVANI Virtual 9-12 Dicembre 2020 Comitati Presidente AIRO Vittorio Donato Presidente AIRB Monica Mangoni AIRO GIOVANI Presidente Eletto AIRO Renzo Corvò Presidente Eletto AIRB Stefano Pergolizzi Coordinatore: Isacco Desideri CONSIGLIO DIRETTIVO AIRO CONSIGLIO DIRETTIVO AIRB CONSIGLIO DIRETTIVO AIRO GIOVANI Andrea R. Filippi Pierluigi Bonomo Paolo Borghetti Maria Antonietta Gambacorta Liliana Belgioia Francesca De Felice Giuseppe Iatì Michele Fiore Carlo Greco Alessandro Magli Francesco Marampon Valerio Nardone Marcello Mignogna Isabella Palumbo COMMISSIONE SCIENTIFICA AIRO Luigi Marafioti Coordinatore: Barbara A. Jereczek-Fossa Roberto Pacelli Alessio Bruni SEGRETARIO ALLA PRESIDENZA Michela Buglione di Monale e Bastia Daniela Musio Pierfrancesco Franco Domenico Genovesi SEGRETARIO AMMINISTRATIVO Icro Meattini Gianpiero Catalano Anna Merlotti Stefano Pergolizzi Marco Trovò 2 XXX CONGRESSO NAZIONALE AIRO XXXII CONGRESSO NAZIONALE AIRB XI CONGRESSO NAZIONALE AIRO GIOVANI Virtual 9-12 Dicembre 2020 Comitati COORDINATORI GRUPPI REGIONALI AIRO COORDINATORI GRUPPI DI STUDIO AIRO ESTRO Salvatrice Campoccia Filippo Alongi Umberto Ricardi Elisa D’Angelo Stefano Arcangeli Vincenzo Valentini Luigi Marafioti Fabio Arcidiacono -

Padova, 29 Luglio 2018 SERGIO GUTIERREZ-FERROL É IL RE DELL'atp COUNTRY 2001 TEAM Tomislav Brkic E Ante Pavic Conquistano Il
Padova, 29 luglio 2018 SERGIO GUTIERREZ-FERROL É IL RE DELL’ATP COUNTRY 2001 TEAM Tomislav Brkic e Ante Pavic conquistano il tabellone di doppio Lo spagnolo Sergio Gutierrez-Ferrol, dopo aver sfiorato il titolo la scorsa settimana, è riuscito a conquistare il primo titolo ATP Challenger in carriera proprio sui campi del Centro Sportivo 2000, dove dal 21 al 29 luglio, all’ATP Country 2001 Team, si sono affrontati alcuni tra i migliori giocatori internazionali. Fin dai primissimi turni i match disputati sono stati seguiti da un pubblico appassionato ed attento: più di 13.000 persone nella settimana del torneo hanno assistito a partite di assoluto valore ed hanno potuto osservare da vicino giocatori professionisti come Simone Bolelli, davisman italiano, Tommy Robredo, ex n.5 del mondo, Gerald Melzer, Thomaz Bellucci e giovani promesse italiane come Gian Marco Moroni, Jacopo Berrettini ed Edoardo Eremin. La scelta di effettuare una sessione serale, con un centrale allestito per l’occasione di luci e tribune, ha riscosso un successo quasi inaspettato, portando più di mille spettatori all’ultimo match di giornata fin dal martedì. La giornata di domenica è dedicata alle finali: nel primo incontro a scendere in campo, non riescono Walter Trusendi e Andrea Vavassori a contenere il gioco esplosivo di Ante Pavic e Tomislav Brkic cedendo con il punteggio di 6/2 7/6(4). Simpatica l’intervista al croato Pavic “so che tifavate tutti per loro in quanto italiani” afferma ridendo “ragazzi, mi dispiace, sarà per l’anno prossimo. A Padova mi trovo sempre molto bene anche perché il mio nome, Ante, è la traduzione di Antonio, come il Santo della vostra città”. -

Gazetka Turnieju Poznań Open 2019
środa, 5 czerwca 2019 PLAN GIER NA ŚRODĘ KORT CENTRALNY Rameez Junaid (Australia)/Enrique Lopez Perez (Hiszpania) Godzina 10 NASTĘPNIE Druga runda gry pojedynczej Andreas Siljestrom (Szwecja)/Elias Ymer (Szwecja) – Dennis [6] Pedro Martinez (Hiszpania) – [Q] Andrea Vavassori Novak (Austria)/Sebastian Ofner (Austria) (Włochy) NASTĘPNIE KORT NUMER 2 Andrea Arnaboldi (Włochy) – [7] Sebastian Ofner (Austria) Godzina 10 NASTĘPNIE [11] Joao Domingues (Portugalia) – [ITF] Sekou Bangoura (Stany [13] Alessandro Giannessi (Włochy) – Sumit Nagal (Indie) Zjednoczone) NASTĘPNIE NASTĘPNIE [16] Blaz Rola (Słowenia) – Tommy Robredo (Hiszpania) [8] Gianluca Mager (Włochy) – [ITF] Christopher Heyman NIE PRZED 17.30 (Belgia) Pierwsza runda gry podwójnej NASTĘPNIE [1] Ze Zhang (Chiny)/Mao-Xin Gong (Chiny) – [WC] Michał Pierwsza runda gry podwójnej Dembek (Polska)/Florin Mergea (Rumunia) Sergio Galdos (Peru)/Pedro Sousa (Portugalia) – [2] Nathaniel Lammons (Stany Zjednoczone)/Fernando Romboli (Brazylia) KORT NUMER 1 NASTĘPNIE Godzina 10 [3] Andrea Vavassori (Włochy)/David Vega Hernandez (Hiszpa- Jose Hernandez-Fernandez (Dominikana) – [12] Filippo Baldi nia) – Sander Gille (Belgia)/Tallon Griekspoor (Holandia) (Włochy) NASTĘPNIE SKRÓTY: [10] Quentin Halys (Francja) – Norbert Gombos (Słowacja) [WC] – dzika karta NASTĘPNIE [Q] – kwalifikant Pierwsza runda gry podwójnej [1] – numer rozstawienia Pedro Martinez (Hiszpania)/Mark Vervoort (Holandia) – [4] [ITF] – zawodnik z listy ITF Trudne zadanie Robredo iszpański tenisista Tommy Robredo w drugiej rundzie poznańskiego chal- Hlengera na kortach Parku Tenisowego Olim- pia zmierzy się z rozstawionym z nume- rem szesnastym Blazem Rolą. W pierwszej rundzie Robredo po ponad dwugodzinnym spotkaniu wygrał z Włochem Jacopo Ber- rettinim w trzech setach. 37-latek uwielbia grę na mączce przy wysokiej temperaturze, co oznacza, że nie jest bez szans w starciu z dziewięć lat młodszym Słoweńcem. -
ATP E COPPA DAVIS, TORINO CAPITALE DEL TENNIS DI LUCIANO BORGHESAN L Tennis Mondiale Conquista La Convocazioni, Ma È Un Privilegio Giovani
INFORMAZIONI E ATTIVITÀ STA PALAZZO CERIANA MAYNERI SPORTING COLO DELLA MPA SPORTI C.so Stati Uniti 27, Torino C.so G. Agnelli 45, Torino CIR NG ANNO 13 - NUMERO 04 MENSILE - Luogo di pubblicazione: Torino. €1,00 Poste Italiane SPA Spedizione in abbonamentopostale D.L. 353/2003 (conv. in 27/02/2004 n. 46) WWW.SPORTING.TO.IT Circolo della Stampa Sporting ASD Art. 1 comma 1 CNS TORINO N. 10 - 2011 MAGGIO 2021 ATP E COPPA DAVIS, TORINO CAPITALE DEL TENNIS DI LUCIANO BORGHESAN l tennis mondiale conquista la convocazioni, ma è un privilegio giovani... Il Circolo della Stampa Torino”. Iprima Capitale del Regno d’Ita- avere a disposizione una rosa così Sporting è un fi ore all’occhiello Ancora una volta, quindi, Torino lia e i torinesi si appassionano al ampia e competitiva”. del tennis che tutti portiamo vo- torna Capitale, questa volta del gioco che agli albori fu tanto pra- Il presidente della Federazione lentieri”. tennis. Sarà una bella occasione ticato da re e principi. A metà no- Italiana Tennis Angelo Binaghi, I candidati alla maglia azzurra per farla conoscere nel mondo, vembre da Londra arrivano le ATP da sempre estimatore del Circolo per la Davis sono davvero tanti, come già avvenne nel 2006. Al- Finals con i più forti otto giocatori della Stampa Sporting, è entu- ma i commenti al momento si cuni campioni favoriti per la loro al mondo e subito dopo la Coppa siasta della “doppietta” torinese, concentrano sulle ATP Finals, an- partecipazione alle ATP Finals Davis vedrà i nostri azzurri impe- ATP Finals e Coppa Davis: “Il che per non condizionare le dif- hanno già espresso la loro soddi- gnati contro le nazionali di USA e vasto mondo dei tennisti italiani fi cili scelte del nuovo capitano. -

Jerusalem Volvo Open 2019 ORDER of PLAY - Tuesday, 21 May 2019
Jerusalem Volvo Open 2019 ORDER OF PLAY - Tuesday, 21 May 2019 CENTER COURT COURT 3 COURT 6 Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 10:00 am Zhizhen ZHANG (CHN) Tom JOMBY (FRA) Frederico FERREIRA SILVA (POR) 1 vs vs vs [Q] Enrico DALLA VALLE (ITA) [WC] Edan LESHEM (ISR) Dimitar KUZMANOV (BUL) followed by followed by Not Before 11:30 am Jamie CERRETANI (USA) [WC] Yshai OLIEL (ISR) [ITF] Arthur RINDERKNECH (FRA) Luis David MARTINEZ (VEN) [1] 2 vs vs vs [Q] Julian OCLEPPO (ITA) Thai-Son KWIATKOWSKI (USA) [5] David MARRERO (ESP) Fernando ROMBOLI (BRA) followed by followed by followed by Brayden SCHNUR (CAN) [1] Joao MENEZES (BRA) LUCKY LOSER 3 vs vs vs Carlos BOLUDA-PURKISS (ESP) Teymuraz GABASHVILI (RUS) Alessandro BEGA (ITA) followed by Not Before 2:30 pm Not Before 2:30 pm After suitable rest After suitable rest [ITF] Tom JOMBY (FRA) Saketh MYNENI (IND) [ITF] Baptiste CREPATTE (FRA) Arthur RINDERKNECH (FRA) Goncalo OLIVEIRA (POR) 4 vs vs vs Roberto ORTEGA-OLMEDO (ESP) [15] [WC] Tuna ALTUNA (TUR) Evan KING (USA) Danilo PETROVIC (SRB) Julian OCLEPPO (ITA) followed by followed by [ITF] Benjamin LOCK (ZIM) Ariel BEHAR (URU) Courtney John LOCK (ZIM) Gonzalo ESCOBAR (ECU) 5 vs vs Luca MARGAROLI (SUI) John-Patrick SMITH (AUS) Andrea VAVASSORI (ITA) [4] Sem VERBEEK (NED) [2] Or Shachar 20 May 2019 at 17:46 Valery Lutkov Tournament Director Order of Play released Challenger Supervisor ANY MATCH ON ANY COURT MAY BE MOVED Denis Zivkovic MATCHES WILL BE CALLED FROM THE Dima Leifman Tour Manager PLAYERS' LOUNGE & LOCKER-ROOM Referee Singles Lucky-Loser/Alternate Sign-in Deadline : 9:30 am Doubles Alternate Sign-in Deadline : 11:00 am. -
![Thomaz BELLUCCI (BRA) [15] Jan CHOINSKI (GBR) Blaz ROLA (SLO) [4] Jelle SELS (NED) Ariel BEHAR (URU) Ante PAVIC (CRO) Blaz ROLA](https://docslib.b-cdn.net/cover/4395/thomaz-bellucci-bra-15-jan-choinski-gbr-blaz-rola-slo-4-jelle-sels-ned-ariel-behar-uru-ante-pavic-cro-blaz-rola-9904395.webp)
Thomaz BELLUCCI (BRA) [15] Jan CHOINSKI (GBR) Blaz ROLA (SLO) [4] Jelle SELS (NED) Ariel BEHAR (URU) Ante PAVIC (CRO) Blaz ROLA
Citta Di Como ORDER OF PLAY - Thursday, 29 August 2019 CAMPO CENTRALE CAMPO 1 CAMPO 2 CAMPO 5 Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 1:30 pm [LL] Fabien REBOUL (FRA) Facundo MENA (ARG) Alejandro TABILO (CHI) [14] 1 vs vs vs Pedro SOUSA (POR) [3] Facundo BAGNIS (ARG) [9] Alex MOLCAN (SVK) followed by followed by Not Before 12:00 noon Thomaz BELLUCCI (BRA) [15] Jan CHOINSKI (GBR) Blaz ROLA (SLO) [4] 2 vs vs vs Dmitry POPKO (KAZ) Salvatore CARUSO (ITA) [2] [PR] Daniel ALTMAIER (GER) Not Before 1:30 pm Not Before 1:30 pm followed by Matches Start At: 1:30 pm after suitable rest Tommy ROBREDO (ESP) [11] or Alejandro TABILO (CHI) [14] or Romain ARNEODO (MON) Jelle SELS (NED) Alex MOLCAN (SVK) Christopher O'CONNELL (AUS) [12] Julian OCLEPPO (ITA) 3 vs vs vs vs Sadio DOUMBIA (FRA) [LL] Fabien REBOUL (FRA) or [Alt] Riccardo BONADIO (ITA) or Ariel BEHAR (URU) Pedro SOUSA (POR) [3] Andrej MARTIN (SVK) [6] Gonzalo ESCOBAR (ECU) [2] followed by followed by followed by after suitable rest after suitable rest Thomaz BELLUCCI (BRA) [15] or Ante PAVIC (CRO) Alessandro GIANNESSI (ITA) [8] Dmitry POPKO (KAZ) Blaz ROLA (SLO) 4 vs vs vs Sebastian OFNER (AUT) [10] Jan CHOINSKI (GBR) or [WC] Andrea ARNABOLDI (ITA) Salvatore CARUSO (ITA) [2] Federico ARNABOLDI (ITA) Not Before 6:00 pm followed by followed by court & time to be arranged Simone BOLELLI (ITA) [WC] Riccardo BALZERANI (ITA) Stefano TRAVAGLIA (ITA) [1] Andrea PELLEGRINO (ITA) Francesco FORTI (ITA) 5 vs vs vs Viktor GALOVIC (CRO) [13] Andrea VAVASSORI (ITA) [Alt] Sadio DOUMBIA (FRA) David VEGA HERNANDEZ (ESP) [4] Fabien REBOUL (FRA) Paolo Carobbio Sebastiano Cavarra Carl Baldwin Tournament Director Referee Challenger Supervisor Order of Play released : 28 August 2019 at 19:14 Singles Lucky-Loser Sign-in Deadline : 9:30 AM MATCHES WILL BE CALLED ANY MATCH ON ANY COURT Doubles Alternate Sign-in Deadline : 1:00 PM FROM THE PLAYERS' LOUNGE & MAY BE MOVED Singles Alternate Sign-in Deadline : 9:30 AM LOCKER-ROOM. -
Julian OCLEPPO
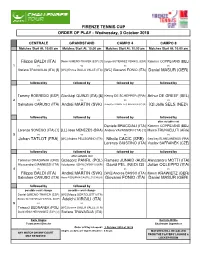
FIRENZE TENNIS CUP ORDER OF PLAY - Wednesday, 3 October 2018 CENTRALE GRANDSTAND CAMPO 4 CAMPO 8 Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 10:00 am Matches Start At: 10:00 am Filippo BALDI (ITA) Daniel GIMENO-TRAVER (ESP) [7] Sergio GUTIERREZ-FERROL (ESP) Kimmer COPPEJANS (BEL) 1 vs vs vs vs Stefano TRAVAGLIA (ITA) [5] [WC] Enrico DALLA VALLE (ITA) [WC] Giovanni FONIO (ITA) Daniel MASUR (GER) followed by followed by followed by followed by Tommy ROBREDO (ESP) Gianluigi QUINZI (ITA) [8] Kenny DE SCHEPPER (FRA) Arthur DE GREEF (BEL) 2 vs vs vs vs Salvatore CARUSO (ITA) Andrej MARTIN (SVK) Roberto CARBALLES BAENA (ESP) [2] [Q] Jelle SELS (NED) followed by followed by followed by followed by after suitable rest Daniele BRACCIALI (ITA) Kimmer COPPEJANS (BEL) Lorenzo SONEGO (ITA) [1] [LL] Joao MENEZES (BRA) Andrea VAVASSORI (ITA) [1] Marco TRUNGELLITI (ARG) 3 vs vs vs vs Johan TATLOT (FRA) [WC] Andrea PELLEGRINO (ITA) Nikola CACIC (SRB) Geoffrey BLANCANEAUX (FRA) Lorenzo GIUSTINO (ITA) Vaclav SAFRANEK (CZE) followed by followed by followed by followed by after suitable rest Tomislav DRAGANJA (CRO) Grzegorz PANFIL (POL) Rameez JUNAID (AUS) Alessandro MOTTI (ITA) Alessandro GIANNESSI (ITA) Volodoymyr UZHYLOVSKYI (UKR) David PEL (NED) [3] Julian OCLEPPO (ITA) 4 vs vs vs vs Filippo BALDI (ITA) Andrej MARTIN (SVK) [WC] Andrea BASSO (ITA) Kevin KRAWIETZ (GER) Salvatore CARUSO (ITA) Hans PODLIPNIK-CASTILLO (CHI) [4] Giovanni FONIO (ITA) Daniel MASUR (GER) followed by followed by possible court change possible court change Daniel GIMENO-TRAVER (ESP) [WC] Marco BORTOLOTTI (ITA) Sergio GUTIERREZ-FERROL (ESP) Adelchi VIRGILI (ITA) 5 vs vs Tomasz BEDNAREK (POL) [WC] Enrico DALLA VALLE (ITA) David VEGA HERNANDEZ (ESP) [2] Stefano TRAVAGLIA (ITA) Carlo Alagna Carmelo Di Dio Tournament Director Challenger Supervisor Order of Play released : 2 October 2018 at 18:29 Singles Lucky-Loser Sign-in Deadline : 9.30 am MATCHES WILL BE CALLED ANY MATCH ON ANY COURT FROM THE PLAYERS' LOUNGE & MAY BE MOVED LOCKER-ROOM. -

Former Atp No. 1 Players and Multiple Grand Slam Champions
PRODUCTION TEAM Editor-in-Chief: Joshua Rey Managing Editor: Nanette Duxin Senior Editor: Maria Garcia-Planas Art Directors: Celine Lenoir Cedric Pucheu Editors: ATP WELCOME Florian Gardetto Greg Sharko In my first year as Chairman of the ATP, it gives me great Contributors: pleasure to welcome you to the 2020 ATP Tour season. Nicola Arzani Fabienne Benoit The ATP has played a central part in my life in so many ways George Ciz over the years, and it is a true honour to have the opportunity Martin Dagahs Mark Epps to serve as ATP Chairman at such an exciting time in the history Cecilia Ghe of our sport. Chris Giles Brendan Gilson Simon Higson The Tour has enjoyed a significant period of growth over the past Susie Hygate decade due to the strength of its global platform of tournaments, Edward La Cava Josh Meiseles as well as the superstar athletes that have transcended sport. Photography: I look forward to building on that success as we seek to maximise Getty Images the growth opportunities for the Tour in the years ahead. Wonderhatch ATP - Peter Staples The ATP Tour is one of the few truly global sports properties, taking place across 64 tournaments in 30 countries, in addition ATP London to the four Grand Slams. The level of content the Tour generates Palliser House, Palliser Road across 11 months of the year is phenomenal, kicking off with London W14 9EB United Kingdom the inaugural ATP Cup in Australia in January, and culminating Tel: +44 207 381 7890 with the Nitto ATP Finals in London in November.