Natalie Joseph-Williams
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Madonna MP3 Collection - Madonna Part 2 Mp3, Flac, Wma
Madonna MP3 Collection - Madonna Part 2 mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Electronic / Hip hop / Pop Album: MP3 Collection - Madonna Part 2 Country: Russia Released: 2012 Style: House, Synth-pop, Ballad, Electro, RnB/Swing, Electro House MP3 version RAR size: 1708 mb FLAC version RAR size: 1392 mb WMA version RAR size: 1865 mb Rating: 4.8 Votes: 427 Other Formats: APE MP2 RA MP1 TTA VOX XM Tracklist Hide Credits Beautiful Stranger (Single) - 1999 1-1 Beautiful Stranger 4:24 1-2 Beautiful Stranger (Remix) 10:15 1-3 Beautiful Stranger (Mix) 4:04 Ray Of Light (Remix Album) - 1999 1-4 Ray Of Light (Ultra Violet Mix) 10:46 Drowned World (Substitut For Love (Bt And Sashas Remix) 1-5 9:28 Remix – Bt, Sasha Sky Fits Heaven (Sasha Remix) 1-6 7:22 Remix – Sasha Power Of Goodbay (Luke Slaters Filtered Mix) 1-7 6:09 Remix – Luke Slater 1-8 Candy Perfume Girl (Sasha Remix) 4:52 1-9 Frozen (Meltdown Mix - Long Version 8:09 1-10 Nothing Really Matters (Re-funk-k-mix) 4:23 Skin (Orbits Uv7 Remix) 1-11 8:00 Remix – Orbit* Frozen (Stereo Mcs Mix) 1-12 5:48 Remix – Stereo Mcs* 1-13 Bonus - What It Feels Like For A Girl (remix) 9:50 1-14 Bonus - Dont Tell Me (remix) 4:26 American Pie (Single) - 2000 1-15 American Pie (Album Version) 4:35 American Pie (Richard Humpty Vission Radio Mix) 1-16 4:30 Remix – Richard Humpty Vission* American Pie (Richard Humpty Vission Visits Madonna) 1-17 5:44 Remix – Richard Humpty Vission* Music - 2000 1-18 Music 3:45 1-19 Impressive Instant 3:38 1-20 Runaway Lover 4:47 1-21 I Deserve It 4:24 1-22 Amazing 3:43 -
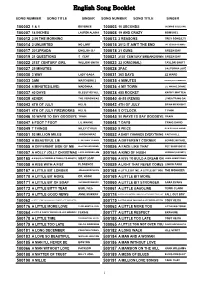
English Song Booklet
English Song Booklet SONG NUMBER SONG TITLE SINGER SONG NUMBER SONG TITLE SINGER 100002 1 & 1 BEYONCE 100003 10 SECONDS JAZMINE SULLIVAN 100007 18 INCHES LAUREN ALAINA 100008 19 AND CRAZY BOMSHEL 100012 2 IN THE MORNING 100013 2 REASONS TREY SONGZ,TI 100014 2 UNLIMITED NO LIMIT 100015 2012 IT AIN'T THE END JAY SEAN,NICKI MINAJ 100017 2012PRADA ENGLISH DJ 100018 21 GUNS GREEN DAY 100019 21 QUESTIONS 5 CENT 100021 21ST CENTURY BREAKDOWN GREEN DAY 100022 21ST CENTURY GIRL WILLOW SMITH 100023 22 (ORIGINAL) TAYLOR SWIFT 100027 25 MINUTES 100028 2PAC CALIFORNIA LOVE 100030 3 WAY LADY GAGA 100031 365 DAYS ZZ WARD 100033 3AM MATCHBOX 2 100035 4 MINUTES MADONNA,JUSTIN TIMBERLAKE 100034 4 MINUTES(LIVE) MADONNA 100036 4 MY TOWN LIL WAYNE,DRAKE 100037 40 DAYS BLESSTHEFALL 100038 455 ROCKET KATHY MATTEA 100039 4EVER THE VERONICAS 100040 4H55 (REMIX) LYNDA TRANG DAI 100043 4TH OF JULY KELIS 100042 4TH OF JULY BRIAN MCKNIGHT 100041 4TH OF JULY FIREWORKS KELIS 100044 5 O'CLOCK T PAIN 100046 50 WAYS TO SAY GOODBYE TRAIN 100045 50 WAYS TO SAY GOODBYE TRAIN 100047 6 FOOT 7 FOOT LIL WAYNE 100048 7 DAYS CRAIG DAVID 100049 7 THINGS MILEY CYRUS 100050 9 PIECE RICK ROSS,LIL WAYNE 100051 93 MILLION MILES JASON MRAZ 100052 A BABY CHANGES EVERYTHING FAITH HILL 100053 A BEAUTIFUL LIE 3 SECONDS TO MARS 100054 A DIFFERENT CORNER GEORGE MICHAEL 100055 A DIFFERENT SIDE OF ME ALLSTAR WEEKEND 100056 A FACE LIKE THAT PET SHOP BOYS 100057 A HOLLY JOLLY CHRISTMAS LADY ANTEBELLUM 500164 A KIND OF HUSH HERMAN'S HERMITS 500165 A KISS IS A TERRIBLE THING (TO WASTE) MEAT LOAF 500166 A KISS TO BUILD A DREAM ON LOUIS ARMSTRONG 100058 A KISS WITH A FIST FLORENCE 100059 A LIGHT THAT NEVER COMES LINKIN PARK 500167 A LITTLE BIT LONGER JONAS BROTHERS 500168 A LITTLE BIT ME, A LITTLE BIT YOU THE MONKEES 500170 A LITTLE BIT MORE DR. -

Administration of Barack H. Obama, 2009 Remarks at a Campaign Rally
Administration of Barack H. Obama, 2009 Remarks at a Campaign Rally for Governor Jon S. Corzine in Camden, New Jersey November 1, 2009 The President. Thank you so much. I am—whoo—fired up! I am fired up. Let me first of all acknowledge some extraordinary public servants who are in the house: Rob Andrews, our wonderful Congressman; Steve Rothman, another great Member of Congress; Gwen Faison, the Mayor of Camden. Thank you, Gwen. To all the other elected officials who are here, I am just glad to be back in Camden. When I was campaigning last year, I said I'd come back once I was President. I couldn't stay away. I like—I just like hanging out in New Jersey. I appreciate all of you who aren't at the Giants/Eagles game. [Laughter] I didn't mean to stir all that up, I'm sorry. All right, settle down now, settle down. Here's the reason I'm back. I am back because we are 2 days away—2 days away from making sure that New Jersey has the kind of quality leadership it deserves, two days away from making sure we're moving forward on education, two days away from making sure that we've got fairness in our economic system, two days away from reelecting Jon Corzine for another 4 years—2 days. Now, at this point in the campaign, you've heard all the arguments. You've seen all the TV ads. You know all the facts of this race. You know that Jon's running for reelection during a challenging time for New Jersey and a challenging time for America. -

Madonna - 1982 - 2009 : the Lyrics Book - 1 SOMMAIRE
Madonna - 1982 - 2009 : The Lyrics Book - www.madonnalex.net 1 SOMMAIRE P.03 P.21 P.51 P.06 P.26 P.56 P.09 P.28 P.59 P.10 P.35 P.66 P.14 P.40 P.74 P.15 P.42 P.17 P.47 Madonna - 1982 - 2009 : The Lyrics Book - www.madonnalex.net 2 ‘Cause you got the best of me Chorus: Borderline feels like I’m going to lose my mind You just keep on pushing my love over the borderline (repeat chorus again) Keep on pushing me baby Don’t you know you drive me crazy You just keep on pushing my love over the borderline Something in your eyes is makin’ such a fool of me When you hold me in your arms you love me till I just can’t see But then you let me down, when I look around, baby you just can’t be found Stop driving me away, I just wanna stay, There’s something I just got to say Just try to understand, I’ve given all I can, ‘Cause you got the best of me (chorus) Keep on pushing me baby MADONNA / Don’t you know you drive me crazy You just keep on pushing my love over the borderline THE FIRST ALBUM Look what your love has done to me 1982 Come on baby set me free You just keep on pushing my love over the borderline You cause me so much pain, I think I’m going insane What does it take to make you see? LUCKY STAR You just keep on pushing my love over the borderline written by Madonna 5:38 You must be my Lucky Star ‘Cause you shine on me wherever you are I just think of you and I start to glow BURNING UP And I need your light written by Madonna 3:45 Don’t put me off ‘cause I’m on fire And baby you know And I can’t quench my desire Don’t you know that I’m burning -

Chapter 1: Parts of Speech Overview, Pp. 1–25
L09NAGUMA10_001-012.qxd 12/11/07 2:28 PM Page 1 Chapter 1: Parts of Speech 14. Leslie always lapses into baby talk when Overview, pp. 1–25 she sees a litter of kittens. Common, Proper, Concrete, and Abstract Nouns, 15. The band included one song that sounded as p. 1 if it had been recorded in an echo chamber. EXERCISE Com, A [or Con] 16. The class presented Ms. Stockdale with a 1. A constitution may have a bill of rights. bouquet of baby’s breath. 2. The Constitution of the United States guar- Com, A 17. The TV weatherperson explained to the antees freedomof speech. P, Con audience how a barometer works. 3. The Works Progress Administration existed 18. In order to get a good batch of cookies, you during the Great Depression. need to use the best oatmeal available. 4. That candidate is a staunch supporter of a Com, A [or Con] 19. A school of killer whales followed in the republican form of government. P, Con wake of the ship. 5. The Articles of Confederation were y of the instructor. 20. The bird-watchers were awe-struck as the approved in 1781. flock of geese lifted into the sky. 6. This document established “a firm league Com, A of friendship” among the states. Pronouns and Antecedents, p. 3 Com, Con Possessive pronouns in items 1 and 3, Ex. A, and 7. The editorial in today’s newspaper items 14 and 15, Ex. B, also may be identified as defended the proposed amendment. possessive adjectives. P, Con 8. -

669014-15 Hartke Libretto
THE GREATER GOOD or THE PASSION OF BOULE DE SUIF Opera in Two Acts Music by Stephen Hartke Text by the composer from Philip Littell’s dramatic adaptation of Guy de Maupassant’s short story, Boule de Suif CD 1 ACT ONE 1 Scene 1: Rouen, the courtyard of the Hôtel de Normandie, 4 AM on a Tuesday in late February 1871. Snow falls in the darkness. The two nuns have already taken their positions, standing motionless a bit to the left, their small carpetbags at their sides. There is a mound of luggage (trunks, suitcases, hatboxes, hampers) closer to center. The only light comes from a dim gas-lamp flickering by the stable door. TITLE CARD (projected on the cyclorama) At three o-clock Monday afternoon it started snowing. TITLE CARD It kept on snowing through the night. Heavily cloaked and muffled, M. and Mme. Carré- Lamadon quickly and quietly enter and go stand near the mound of luggage. They shiver visibly from the cold. TITLE CARD At four in the morning a group of travelers gathered. The Count and Countess enter, affecting a more courtly pace, but clearly chilled to the bone. The stable door opens a crack and dim light spills out. A stable-boy holding a lantern pokes his head out and checks on the gathering travelers. Cornudet lopes in, carrying his belongings in a small 8.669014-15 The Greater Good P & C 2007 Naxos Rights International Ltd. Page 1 parcel tied up with twine. He pauses a moment by the stable door and takes a swig from his rum gourd. -

Stardigio Program
スターデジオ チャンネル:450 洋楽アーティスト特集 放送日:2019/07/08~2019/07/14 「番組案内 (8時間サイクル)」 開始時間:4:00~/12:00~/20:00~ 楽曲タイトル 演奏者名 ■MADONNA 特集 (1) Everybody MADONNA BURNING UP MADONNA HOLIDAY MADONNA LUCKY STAR MADONNA Borderline MADONNA MATERIAL GIRL MADONNA LIKE A VIRGIN MADONNA STAY MADONNA ANGEL MADONNA SHOO-BEE-DOO MADONNA DRESS YOU UP MADONNA INTO THE GROOVE MADONNA GAMBLER MADONNA CRAZY FOR YOU MADONNA ■MADONNA 特集 (2) PAPA DON'T PREACH MADONNA OPEN YOUR HEART MADONNA LIVE TO TELL MADONNA TRUE BLUE MADONNA LA ISLA BONITA ~美しき島 MADONNA SPOTLIGHT MADONNA LIKE A PRAYER MADONNA EXPRESS YOURSELF MADONNA CHERISH MADONNA OH FATHER MADONNA DEAR JESSIE MADONNA KEEP IT TOGETHER MADONNA ■MADONNA 特集 (3) WHO'S THAT GIRL MADONNA CAUSING A COMMOTION MADONNA THE LOOK OF LOVE MADONNA HANKY PANKY MADONNA SOONER OR LATER MADONNA CRY BABY MADONNA VOGUE MADONNA Erotica MADONNA DEEPER AND DEEPER MADONNA BAD GIRL MADONNA FEVER MADONNA BYE BYE BABY MADONNA RAIN MADONNA ■MADONNA 特集 (4) JUSTIFY MY LOVE MADONNA RESCUE ME MADONNA THIS USED TO BE MY PLAYGROUND MADONNA I'LL REMEMBER MADONNA SECRET MADONNA TAKE A BOW MADONNA BEDTIME STORY MADONNA HUMAN NATURE MADONNA DON'T STOP MADONNA YOU'LL SEE(愛をこえて) MADONNA ONE MORE CHANCE MADONNA LOVE DON'T LIVE HERE ANYMORE(Remix)(愛は色あせて) MADONNA ■MADONNA 特集 (5) YOU MUST LOVE ME ~映画「EVITA」より~ MADONNA DON'T CRY FOR ME ARGENTINA [RADIO EDIT] MADONNA ANOTHER SUITCASE IN ANOTHER HALL MADONNA ~映画「EVITA」より~ Frozen [Radio Edit] MADONNA RAY OF LIGHT MADONNA THE POWER OF GOOD-BYE MADONNA NOTHING REALLY MATTERS MADONNA AMERICAN PIE MADONNA ~映画「ネクスト・ベスト・シング」より~ TIME STOOD STILL MADONNA ~映画「ネクスト・ベスト・シング」より~ Music MADONNA Impressive Instant MADONNA Don't Tell Me MADONNA What It Feels Like For A Girl [Radio Edit] MADONNA I Deserve It MADONNA ■MADONNA 特集 (6) Beautiful Stranger MADONNA Die Another Day [Radio Edit] MADONNA AMERICAN LIFE MADONNA HOLLYWOOD MADONNA NOBODY KNOWS ME MADONNA NOTHING FAILS MADONNA LOVE PROFUSION MADONNA MOTHER AND FATHER MADONNA Me Against The Music BRITNEY SPEARS feat. -

The Body .Pdf
Fall from Innocence: The Body STEPHEN KING Level 5 Retold by Robin Waterfield Series Editors: Andy Hopkins and Jocelyn Potter Pearson Education Limited Edinburgh Gate, Harlow, Essex CM20 2JE, England and Associated Companies throughout the world. ISBN 0 582 41817 8 Fall from Innocence: The Body from DIFFERENT SEASONS by Stephen King Copyright © Stephen King 1982 Published by arrangement with Viking Penguin, a division of Penguin Books USA, Inc. This adaptation first published by Penguin Books 1994 Published by Addison Wesley Longman Limited and Penguin Books Ltd. 1998 New edition first published 1999 9 10 Text copyright © Robin Waterfield 1994 Illustrations copyright © Ian Andrew 1994 All rights reserved The moral right of the adapter and of the illustrator has been asserted Typeset by RefineCatch Limited, Bungay, Suffolk Set in 11/14pt Monotype Bembo Printed in Spain by Mateu Cromo, S.A. Pinto (Madrid) All rights reserved; no part of this publication may he reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permission of the Publishers. Published by Pearson Education Limited in association with Penguin Books Ltd., both companies being subsidiaries of Pearson Plc For a complete list of titles available in the Penguin Readers series please write to your local Pearson Education office or contact: Penguin Readers Marketing Department, Pearson Education, Edinburgh Gate, Harlow, Essex, CM20 2JE. Contents page Introduction -

Film Review Race to Nowhere: the Dark Side of America's
Vol. 15, No. 1 International Journal of Multicultural Education 2013 Film Review Race to Nowhere: The Dark Side of America’s Achievement Culture Produced and Co-directed by Vicki Abeles (2010) John Caruso, Jr. Media Review Editor Review Conclusion Note Website Resources Review In 85 minutes Vicki Abeles, producer and co-director of Race to Nowhere, presents personal vignettes that form a montage of parents pressuring their adolescent children to achieve academically and the tragic consequences of failure to meet their rising expectations. The end of the film provides a coherent summation of what communities need to do to reduce the stress levels placed on children by parents. If it takes a whole village to raise a child, then according to the thesis of the film, it requires the entire community to monitor and adjust their expectations of attending college, establishing a career, and living the good life. The bell-shaped curve of intelligence suggests only two percent of students can achieve straight A grades and score in the 98th percentile on the SAT/ACT. The fictional Lake Wobegon platitude of every child being above average in school has become a painful milestone leading to higher rates of stress, 1 Vol. 15, No. 1 International Journal of Multicultural Education 2013 depression and alienation. A majority of middle-class above-average children cannot become the geniuses parents imagine they are without suffering abysmal personal failure, as the film shows. The quality of life in the United States has plateaued, and many communities have experienced an economic decline. College-educated parents no longer feel that they can easily bestow a natural inheritance of their privilege on their children. -

Salvatore Bartolotta UNED Showgirl, Cantautora, Directora De Cine
Mas igualdad. Redes para la igualdad MDNA forever Salvatore Bartolotta UNED Showgirl, cantautora, directora de cine, autora de libros, Madonna en el nuevo milenio no para. El marido Guy Ritchie la dirige en Swept Away 1, remake de la película de 1974 de Lina Wertmüller Travolti da un insolito destino nell’azzurro mare d’agosto. La actriz interpreta el mismo papel que Mariangela Melato con Adriano Giannini, cuyo padre, Giancarlo, también se metió en la piel del mismo personaje. La película fue rodada en Cerdeña durante el verano del 2002. En octubre del mismo año Madonna publica Die Another Day, tema portante de la banda sonora de la homónima película de Lee Tamahori que anticipa la salida de su noveno álbum grabado en estudio. En este film Madonna recita un breve cammeo, el role de una monitora de esgrima. En abril del 2003 sale American Life2, disco con sonoridades electrónico- acústicas y con textos de naturaleza política y espiritual. Según Stephen Thomas Erlewine (2012): American Life is an album performed by a vocalist who has abandoned the U.S. for the U.K. and co-produced by a French techno mastermind, recorded during a time of strife in America, and released just after the country completed a war. Given that context and given that the vocalist is arguably the biggest star in the world, the title can’t help but carry some import, carry the weight of social commentary. And it follows through on that promise, sometimes explicitly and sometimes implicitly, but either way, American Life winds up as the first Madonna record with ambitions as serious as a textbook. -
1 "THE PROGRAM" by David S. Ward and Aaron Latham 10/6/92 Draft
1 "THE PROGRAM" by David S. Ward and Aaron Latham 10/6/92 Draft REVISED BLUE 10/26/92 REVISED PINK 11/2/92 REVISED YELLOW 11/5/92 REVISED GREEN 11/6/92 REVISED GOLDEN ROD 11/11/92 REVISED TAN 11/23/92 SHOOTING DRAFT FADE IN ON BLACK SCREEN SPORTSCASTER'S VOICE (V.O.) Allright, bowl bid ridin' here for E.S.U. Fourth down on the Georgia Tech 18. 4 ticks left. Kane sets 'em down. INSTANT CUT TO: LINE OF TAPED KNUCKLES - NIGHT 2 smashing into the mud, as a football OFFENSIVE LINE comes set, frosted breath steaming across to: The DEFENSIVE LINE digging in, ready to explode. CLOSE ON JOE KANE E.S.U. quarterback, barking signals. The ball is snapped, and we go to SLOW MOTION as the lines crash together in the slop. Joe rolls to the right, looking downfield. A huge DEFENSIVE END bears down on him. Joe jukes. The end whips on by, grabbing for jersey, slipping off. But big NUMBER 75 is closing the gap. On the run, Joe releases a desperation pass toward the end zone, just as 75 catches him and buries him face-down in the swamp. We FOLLOW THE BALL, spiraling through the slanting rain. RAY GRIFFEN, black running back, glances back for it, two DEFENSIVE BACKS with him. All three leap in unison, climbing as high as they can, clutching, clawing for the ball. The ball floats down, kisses off the tangle of fingers, splashes to the ground, and rolls to a stop in the mud. -

A Translation of Alejandra Pizarnik's Poetry
Bard College Bard Digital Commons Senior Projects Spring 2017 Bard Undergraduate Senior Projects Spring 2017 "Nobody knows me I speak the night": A Translation of Alejandra Pizarnik's Poetry Lydia Merriman Herrick Bard College, [email protected] Follow this and additional works at: https://digitalcommons.bard.edu/senproj_s2017 Part of the Latin American Literature Commons This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. Recommended Citation Herrick, Lydia Merriman, ""Nobody knows me I speak the night": A Translation of Alejandra Pizarnik's Poetry" (2017). Senior Projects Spring 2017. 328. https://digitalcommons.bard.edu/senproj_s2017/328 This Open Access work is protected by copyright and/or related rights. It has been provided to you by Bard College's Stevenson Library with permission from the rights-holder(s). You are free to use this work in any way that is permitted by the copyright and related rights. For other uses you need to obtain permission from the rights- holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/or on the work itself. For more information, please contact [email protected]. “Nobody knows me I speak the night”: A Translation of Alejandra Pizarnik’s Poetry Senior Project Submitted to The Division of Languages and Literature of Bard College by Lydia Merriman Herrick Annandale-on-Hudson, New York May 2017 Acknowledgements First, I would like to thank my phenomenal adviser, Melanie Nicholson, for her profound wisdom and guidance these past four years. Her constant academic and personal support has been especially invaluable this year, when her seemingly endless energy continually inspired me.