Disorders of STXBP1?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Childhood Epilepsy: an Update on Diagnosis and Management
American Journal of Neuroscience Review Childhood Epilepsy: An Update on Diagnosis and Management Khaled Saad Department of Pediatrics, Faculty of Medicine, University of Assiut, Assiut 71516, Egypt Article history Abstract: Within the past few years there is a rapid expansion in our Received: 23-10-2014 understanding of epilepsy. The development of new anti-epileptic drugs and Revised: 25-11-2014 refinements to epilepsy surgery are widening the therapeutic options for Accepted: 12-01-2015 epilepsy. In addition, the classification of the epilepsies continues to evolve based on an increased understanding of the molecular genetics of the condition and this includes the recognition of possible novel epilepsy syndromes. This review considers some of these exciting developments, as well as addressing the essential features of the diagnosis, investigations, management and impact of epilepsy in childhood. Keywords: Children, Epilepsy, Seizure, Anti-Epileptic Drugs Introduction guidelines for optimal practices, rational therapy and counseling (Aylwad, 2008; Tamber and Mountz, 2012; Epilepsy is a common heterogeneous neurological Sharma, 2013). problem in children. It exerts a significant physical, psychological, economic and social toll on children and Definitions their caregivers. Fifty million people have epilepsies A seizure is defined as an excessive burst of abnormal globally; more than half of them are children. In the synchronized neuronal activity affecting small or large USA; between 25,000 and 40,000 children will have a neuronal networks that results in clinical manifestations first non-febrile seizure each year. The problem is that are sudden, transient and usually brief. Epilepsy is further compounded in developing countries as they add defined as a disorder of the brain characterized by any of about 75-80% of new cases of epilepsy (Guerrini, 2006; the following conditions: (1) At least two unprovoked (or Tamber and Mountz, 2012; Sharma, 2013). -

Oegtp - Epilepsy Test Requisition Lab Use Only: Patient Information
OEGTP - EPILEPSY TEST REQUISITION LAB USE ONLY: PATIENT INFORMATION: Received date: Name: Notes: Address: Date of Birth: YY/MM/DD Sex: M F Health Card No: TEST REQUEST: See page 2 for gene list for each of the panels below Epilepsy Comprehensive panel: 167 genes Childhood Onset Epilepsy panel: 45 genes Focal Epilepsy panel: 14 genes Brain Malformation Epilepsy panel: 44 genes London Health Sciences Centre – (Molecular Genetics) London Health Sciences Centre Progressive Myoclonic Epilepsy panel: 20 genes Actionable Gene Epilepsy panel: 22 genes Early Infantile Epilepsy panel: 51 genes Single gene test: Carrier Testing/ KnownFamily Mutation SAMPLE COLLECTION: Name of index case in the family (include copy of report) Date drawn: YY/MM/DD EDTA blood (lavender top) (5ml at room temp) Affected Unaffected Date of Birth: Relationship to patient: REFERRING PHYSICIAN: Authorized Signature is Required Gene: RefSeq:NM Physician Name (print): Mutation: Signature: Email: REASON FOR REFERRAL: Clinic/Hospital: Diagnostic Testing Address: Clinical Diagnosis: Telephone: Fax: CC report to: Name: Clinical Presentation: Address: Telephone: Fax: Molecular Genetics Laboratory Victoria Hospital, Room B10-123A 800 Commissioners Rd. E. London, Ontario | N6A 5W9 Pathology and Laboratory Medicine Ph: 519-685-8122 | Fax: 519-685-8279 Page 1 of 6 Page OEGTP (2021/05/28) OEGTP - EPILEPSY TEST PANELS Patient Identifier: COMPREHENSIVE EPILEPSY PANEL: 167 Genes ACTB, ACTG1, ADSL, AKT3, ALDH7A1, AMT, AP3B2, ARFGEF2, ARHGEF9, ARV1, ARX, ASAH1, ASNS, ATP1A3, ATP6V0A2, ATP7A, -

Causes of Mortality in Early Infantile Epileptic Encephalopathy: a Systematic Review
Epilepsy & Behavior 85 (2018) 32–36 Contents lists available at ScienceDirect Epilepsy & Behavior journal homepage: www.elsevier.com/locate/yebeh Review Causes of mortality in early infantile epileptic encephalopathy: A systematic review Graciane Radaelli a,b, Francisco de Souza Santos b, Wyllians Vendramini Borelli b,LeonardoPisanib, Magda Lahorgue Nunes b,d, Fulvio Alexandre Scorza c,d, Jaderson Costa da Costa b,d,⁎ a Federal University of São Paulo (UNIFESP)/Paulista School of Medicine, São Paulo, Brazil b Brain Institute of Rio Grande do Sul (BraIns), Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, RS, Brazil c Laboratory of Neuroscience, Department of Neurology and Neurosurgery, Federal University of São Paulo, São Paulo, SP, Brazil d CNPq, Brazil article info abstract Article history: Introduction: Early infantile epileptic encephalopathy syndrome (EIEE), also known as Ohtahara syndrome, is an Received 6 March 2018 age-dependent epileptic encephalopathy syndrome defined by clinical features and electroencephalographic Revised 25 April 2018 findings. Epileptic disorders with refractory seizures beginning in the neonatal period and/or early infancy Accepted 5 May 2018 have a potential risk of premature mortality, including sudden death. We aimed to identify the causes of death Available online xxxx in EIEE and conducted a literature survey of fatal outcomes. Methods: We performed a literature search in MEDLINE, EMBASE, and Web of Science for data from inception Keywords: “ ”“ ”“ ”“ ” “ ” Ohtahara syndrome until September 2017. The terms death sudden, unexplained death, SUDEP, lethal, and fatal and the “ ”“ ”“ ”“ Early infantile epileptic syndrome medical subject heading terms epileptic encephalopathy, mortality, death, sudden infant death syn- Suppression burst drome,” and “human” were used in the search strategy. -

Neonatal Seizures Revisited
children Review Neonatal Seizures Revisited Konrad Kaminiów 1 , Sylwia Kozak 1 and Justyna Paprocka 2,* 1 Students’ Scientific Society, Department of Pediatric Neurology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, 40-752 Katowice, Poland; [email protected] (K.K.); [email protected] (S.K.) 2 Department of Pediatric Neurology, Faculty of Medical Sciences in Katowice, Medical University of Silesia, 40-752 Katowice, Poland * Correspondence: [email protected] Abstract: Seizures are the most common neurological disorder in newborns and are most prevalent in the neonatal period. They are mostly caused by severe disorders of the central nervous system (CNS). However, they can also be a sign of the immaturity of the infant’s brain, which is characterized by the presence of specific factors that increase excitation and reduce inhibition. The most common disorders which result in acute brain damage and can manifest as seizures in neonates include hypoxic-ischemic encephalopathy (HIE), ischemic stroke, intracranial hemorrhage, infections of the CNS as well as electrolyte and biochemical disturbances. The therapeutic management of neonates and the prognosis are different depending on the etiology of the disorders that cause seizures which can lead to death or disability. Therefore, establishing a prompt diagnosis and implementing appropriate treatment are significant, as they can limit adverse long-term effects and improve outcomes. In this review paper, we present the latest reports on the etiology, pathomechanism, clinical symptoms and guidelines for the management of neonates with acute symptomatic seizures. Keywords: neonatal seizures; pathophysiology; genetics; inborn errors of metabolism Citation: Kaminiów, K.; Kozak, S.; Paprocka, J. -

Epileptic Mechanisms Shared by Alzheimer's Disease
International Journal of Molecular Sciences Review Epileptic Mechanisms Shared by Alzheimer’s Disease: Viewed via the Unique Lens of Genetic Epilepsy Jing-Qiong Kang 1,2 1 Department of Neurology & Pharmacology, Vanderbilt University Medical Center, Nashville, TN 37232-8552, USA; [email protected]; Tel.: +1-615-936-8399; Fax: +1-615-322-5517 2 Vanderbilt Kennedy Center of Human Development, Vanderbilt Brain Institute, Vanderbilt University, Nashville, TN 37232-8522, USA Abstract: Our recent work on genetic epilepsy (GE) has identified common mechanisms between GE and neurodegenerative diseases including Alzheimer’s disease (AD). Although both disorders are seemingly unrelated and occur at opposite ends of the age spectrum, it is likely there are shared mechanisms and studies on GE could provide unique insights into AD pathogenesis. Neurodegen- erative diseases are typically late-onset disorders, but the underlying pathology may have already occurred long before the clinical symptoms emerge. Pathophysiology in the early phase of these diseases is understudied but critical for developing mechanism-based treatment. In AD, increased seizure susceptibility and silent epileptiform activity due to disrupted excitatory/inhibitory (E/I) balance has been identified much earlier than cognition deficit. Increased epileptiform activity is likely a main pathology in the early phase that directly contributes to impaired cognition. It is an enormous challenge to model the early phase of pathology with conventional AD mouse models due to the chronic disease course, let alone the complex interplay between subclinical nonconvulsive epileptiform activity, AD pathology, and cognition deficit. We have extensively studied GE, especially with gene mutations that affect the GABA pathway such as mutations in GABAA receptors and GABA transporter Citation: Kang, J.-Q. -

Abstracts from the 51St European Society of Human Genetics Conference: Electronic Posters
European Journal of Human Genetics (2019) 27:870–1041 https://doi.org/10.1038/s41431-019-0408-3 MEETING ABSTRACTS Abstracts from the 51st European Society of Human Genetics Conference: Electronic Posters © European Society of Human Genetics 2019 June 16–19, 2018, Fiera Milano Congressi, Milan Italy Sponsorship: Publication of this supplement was sponsored by the European Society of Human Genetics. All content was reviewed and approved by the ESHG Scientific Programme Committee, which held full responsibility for the abstract selections. Disclosure Information: In order to help readers form their own judgments of potential bias in published abstracts, authors are asked to declare any competing financial interests. Contributions of up to EUR 10 000.- (Ten thousand Euros, or equivalent value in kind) per year per company are considered "Modest". Contributions above EUR 10 000.- per year are considered "Significant". 1234567890();,: 1234567890();,: E-P01 Reproductive Genetics/Prenatal Genetics then compared this data to de novo cases where research based PO studies were completed (N=57) in NY. E-P01.01 Results: MFSIQ (66.4) for familial deletions was Parent of origin in familial 22q11.2 deletions impacts full statistically lower (p = .01) than for de novo deletions scale intelligence quotient scores (N=399, MFSIQ=76.2). MFSIQ for children with mater- nally inherited deletions (63.7) was statistically lower D. E. McGinn1,2, M. Unolt3,4, T. B. Crowley1, B. S. Emanuel1,5, (p = .03) than for paternally inherited deletions (72.0). As E. H. Zackai1,5, E. Moss1, B. Morrow6, B. Nowakowska7,J. compared with the NY cohort where the MFSIQ for Vermeesch8, A. -

(12) Patent Application Publication (10) Pub. No.: US 2010/0210567 A1 Bevec (43) Pub
US 2010O2.10567A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/0210567 A1 Bevec (43) Pub. Date: Aug. 19, 2010 (54) USE OF ATUFTSINASATHERAPEUTIC Publication Classification AGENT (51) Int. Cl. A638/07 (2006.01) (76) Inventor: Dorian Bevec, Germering (DE) C07K 5/103 (2006.01) A6IP35/00 (2006.01) Correspondence Address: A6IPL/I6 (2006.01) WINSTEAD PC A6IP3L/20 (2006.01) i. 2O1 US (52) U.S. Cl. ........................................... 514/18: 530/330 9 (US) (57) ABSTRACT (21) Appl. No.: 12/677,311 The present invention is directed to the use of the peptide compound Thr-Lys-Pro-Arg-OH as a therapeutic agent for (22) PCT Filed: Sep. 9, 2008 the prophylaxis and/or treatment of cancer, autoimmune dis eases, fibrotic diseases, inflammatory diseases, neurodegen (86). PCT No.: PCT/EP2008/007470 erative diseases, infectious diseases, lung diseases, heart and vascular diseases and metabolic diseases. Moreover the S371 (c)(1), present invention relates to pharmaceutical compositions (2), (4) Date: Mar. 10, 2010 preferably inform of a lyophilisate or liquid buffersolution or artificial mother milk formulation or mother milk substitute (30) Foreign Application Priority Data containing the peptide Thr-Lys-Pro-Arg-OH optionally together with at least one pharmaceutically acceptable car Sep. 11, 2007 (EP) .................................. O7017754.8 rier, cryoprotectant, lyoprotectant, excipient and/or diluent. US 2010/0210567 A1 Aug. 19, 2010 USE OF ATUFTSNASATHERAPEUTIC ment of Hepatitis BVirus infection, diseases caused by Hepa AGENT titis B Virus infection, acute hepatitis, chronic hepatitis, full minant liver failure, liver cirrhosis, cancer associated with Hepatitis B Virus infection. 0001. The present invention is directed to the use of the Cancer, Tumors, Proliferative Diseases, Malignancies and peptide compound Thr-Lys-Pro-Arg-OH (Tuftsin) as a thera their Metastases peutic agent for the prophylaxis and/or treatment of cancer, 0008. -
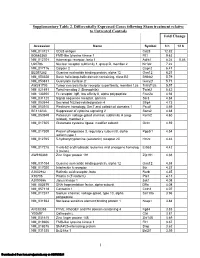
Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

Pediatric Disorders
Neurological Disorder Part 3 - Pediatric Disorders CDKL5 Disorder • Characteristics: • Rare x-linked genetic disorder • CDLK5 mutations cause deficiencies in the protein needed for normal brain development • More common in females; however males with the disorder are affected much more severely than females © Trusted Neurodiagnostics Academy CDKL5 Disorder • Characteristics • CDKL5D mutations can be found in children who have been diagnosed with infantile spasms, Lennox Gastaut syndrome, Rett Syndrome, West Syndrome and autism © Trusted Neurodiagnostics Academy CDKL5 Disorder • Symptoms: • Infantile spasms beginning the first 3 - 6 months of life • Neurodevelopmental impairment • Patients cannot walk, talk, or feed themselves • Repetitive hand movements (stereotypies) © Trusted Neurodiagnostics Academy CDKL5 Disorder • Seizures: • Early onset • Infantile spasms, myoclonic, tonic, tonic-clonic seizures • Status epilepticus and non convulsive status epilepticus can occur © Trusted Neurodiagnostics Academy CDKL5 Disorder • Diagnosis: • Genetic blood testing to confirm the change or mutation on the CDKL5 gene • EEG © Trusted Neurodiagnostics Academy CDKL5 Disorder • EEG Findings: • Early in the disorder • EEG may be normal or slightly abnormal • During progression of the disorder • Some background activity is slow and epileptic discharges can be seen in one or more areas • Burst Suppression • Atypical hypsarrhythmia © Trusted Neurodiagnostics Academy CDKL5 Disorder © Trusted Neurodiagnostics Academy CDKL5 Disorder • Treatment: • Seizures -

STXBP1 Analysis for Early Infantile Epileptic Encephalopathy
STXBP1 Analysis for Early Infantile Epileptic Encephalopathy Clinical Features: Early infantile epileptic encephalopathy (EIEE) [MIM #308350], also known as Ohtahara syndrome, is a severe form of epilepsy characterized by frequent tonic spasms with onset in the first months of life. EEG reveals suppression-burst patterns, characterized by high-voltage bursts alternating with almost flat suppression phases. Seizures are medically intractable with evolution to West syndrome at 3-6 months of age and then Lennox- Gastaut syndrome at 1-3 years of age. EIEE represents less than 1% of all epilepsies occurring in children less than 15 years of age (1). Patients have severe developmental delay and poor prognosis. Molecular Genetics: Mutations of the Syntaxin binding protein 1 (STXBP1) [OMIM #602926] have been identified in patients with early infantile epileptic encephalopathy 4 (EIEE4) [MIM #612164]. The STXBP1 gene maps to 9q34.1 and has 19 coding exons. Syntaxin binding protein 1, more commonly referred to as MUNC18-1, is a neuron specific protein of the SEC1 family of membrane-trafficking proteins. MUNC18-1 is expressed throughout the brain and is a key component for calcium-dependent neurotransmitter release. Sequencing of STXBP1 detected mutations in 4 out of 106 patients with EIEE [2]. Earlier reports identified 4 heterozygous missense mutation in 13 patients with EIEE (2). Affected individuals with microdeletions involving STXBP1 have also been reported (3). Inheritance: STXBP1 mutations are inherited in an autosomal dominant pattern. Most cases are de novo and there has been one family reported with paternal mosaicism of a STXBP1 mutation (4). Resources: Aaron’s Ohtahara Foundation www.ohtahara.org Test methods: Comprehensive sequence coverage of the coding regions and splice junctions of the STXBP1 gene is performed. -

Deciphering the Molecular Profile of Plaques, Memory Decline And
ORIGINAL RESEARCH ARTICLE published: 16 April 2014 AGING NEUROSCIENCE doi: 10.3389/fnagi.2014.00075 Deciphering the molecular profile of plaques, memory decline and neuron loss in two mouse models for Alzheimer’s disease by deep sequencing Yvonne Bouter 1†,Tim Kacprowski 2,3†, Robert Weissmann4, Katharina Dietrich1, Henning Borgers 1, Andreas Brauß1, Christian Sperling 4, Oliver Wirths 1, Mario Albrecht 2,5, Lars R. Jensen4, Andreas W. Kuss 4* andThomas A. Bayer 1* 1 Division of Molecular Psychiatry, Georg-August-University Goettingen, University Medicine Goettingen, Goettingen, Germany 2 Department of Bioinformatics, Institute of Biometrics and Medical Informatics, University Medicine Greifswald, Greifswald, Germany 3 Department of Functional Genomics, Interfaculty Institute for Genetics and Functional Genomics, University Medicine Greifswald, Greifswald, Germany 4 Human Molecular Genetics, Department for Human Genetics of the Institute for Genetics and Functional Genomics, Institute for Human Genetics, University Medicine Greifswald, Ernst-Moritz-Arndt University Greifswald, Greifswald, Germany 5 Institute for Knowledge Discovery, Graz University of Technology, Graz, Austria Edited by: One of the central research questions on the etiology of Alzheimer’s disease (AD) is the Isidro Ferrer, University of Barcelona, elucidation of the molecular signatures triggered by the amyloid cascade of pathological Spain events. Next-generation sequencing allows the identification of genes involved in disease Reviewed by: Isidro Ferrer, University of Barcelona, processes in an unbiased manner. We have combined this technique with the analysis of Spain two AD mouse models: (1) The 5XFAD model develops early plaque formation, intraneu- Dietmar R. Thal, University of Ulm, ronal Ab aggregation, neuron loss, and behavioral deficits. (2)TheTg4–42 model expresses Germany N-truncated Ab4–42 and develops neuron loss and behavioral deficits albeit without plaque *Correspondence: formation. -
Genetic and Phenotypic Heterogeneity Suggest Therapeutic Implications in SCN2A-Related Disorders
doi:10.1093/brain/awx054 BRAIN 2017: Page 1 of 21 | 1 Genetic and phenotypic heterogeneity suggest therapeutic implications in SCN2A-related disorders Markus Wolff,1,Ã Katrine M. Johannesen,2,3,Ã Ulrike B. S. Hedrich,4,Ã Silvia Masnada,5 Guido Rubboli,2,6 Elena Gardella,2,3 Gaetan Lesca,7,8,9 Dorothe´e Ville,10 Mathieu Milh,11,12 Laurent Villard,12 Alexandra Afenjar,13 Sandra Chantot-Bastaraud,13 Cyril Mignot,14 Caroline Lardennois,15 Caroline Nava,16,17 Niklas Schwarz,4 Marion Ge´rard,18 Laurence Perrin,19 Diane Doummar,20 Ste´phane Auvin,21,22 Maria J. Miranda,23 Maja Hempel,24 Eva Brilstra,25 Nine Knoers,25 Nienke Verbeek,25 Marjan van Kempen,25 Kees P. Braun,26 Grazia Mancini,27 Saskia Biskup,28 Konstanze Ho¨rtnagel,28 Miriam Do¨cker,28 Thomas Bast,29 Tobias Loddenkemper,30 Lily Wong-Kisiel,31 Friedrich M. Baumeister,32 Walid Fazeli,33 Pasquale Striano,34 Robertino Dilena,35 Elena Fontana,36 Federico Zara,37 Gerhard Kurlemann,38 Joerg Klepper,39 Jess G. Thoene,40 Daniel H. Arndt,41 Nicolas Deconinck,42 Thomas Schmitt-Mechelke,43 Oliver Maier,44 Hiltrud Muhle,45 Beverly Wical,46 Claudio Finetti,47 Reinhard Bru¨ckner,48 Joachim Pietz,49 Gu¨nther Golla,50 Dinesh Jillella,51 Karen M. Linnet,52 Perrine Charles,53 Ute Moog,54 Eve O˜ iglane-Shlik,55 John F. Mantovani,56 Kristen Park,57 Marie Deprez,58 Damien Lederer,58 Sandrine Mary,58 Emmanuel Scalais,59 Laila Selim,60 Rudy Van Coster,61 Lieven Lagae,62 Marina Nikanorova,2 Helle Hjalgrim,2,3 G.